Abstract
Background
Oxidative stress and redox-regulating enzymes may have roles both in lymphomagenesis and resistance to lymphoma therapy. Previous studies from the pre-rituximab era suggest that antioxidant enzyme expression is related to prognosis in diffuse large B-cell lymphoma (DLBCL), although these results cannot be extrapolated to patient populations undergoing modern treatment modalities. In this study we assessed expression of the oxidative stress markers 8-hydroxydeoxyguanosine (8-OHdG) and nitrotyrosine and the antioxidant enzymes thioredoxin (Trx), manganese superoxide dismutase (MnSOD) and glutamate-cysteine ligase (GCL) via immunohistochemistry in 106 patients with DLBCL. All patients were treated with CHOP-like therapy combined with rituximab. Immunostaining results were correlated with progression-free survival, disease-specific survival and traditional prognostic factors of DLBCL.
Results
Strong 8-OHdG immunostaining intensity was associated with extranodal involvement (p = 0.00002), a high International Prognostic Index (p = 0.002) and strong Trx (p = 0.011) and GCL (p = 0.0003) expression. Strong Trx staining intensity was associated with poor progression-free survival (p = 0.046) and poor disease-specific survival (p = 0.015). Strong GCL immunostaining intensity predicted poor progression-free survival (p = 0.049). Patients with either strong Trx or strong nitrotyrosine expression showed significantly poorer progression-free survival (p = 0.003) and disease-specific survival (p = 0.031) compared with the other patients.
Conclusions
The redox state-regulating enzymes GCL and Trx are promising markers in the evaluation of DLBCL prognosis in the era of modern immunochemotherapy.
Similar content being viewed by others
Background
Of lymphomas, diffuse large B-cell lymphoma (DLBCL) accounts for 30% to 40%. DLBCL comprises three different subtypes as determined by gene expression profiling: the germinal center (GC) type, the activated B-cell type and a third heterogeneous type that cannot be included in either of the two other categories [1]. In routine practice the subtypes are classified by means of by immunohistochemical grouping (Hans' algorithm) into GC and non-GC subtypes [2]. Standard treatment for DLBCL consists of CHOP (cyclophosphamide, doxorubicin, vincristine and prednisone) or CHOP-type regimens and rituximab. Rituximab has revolutionized the treatment of DLBCL by increasing survival in all International Prognostic Index (IPI) classes [3]. New molecular markers predicting the outcome of DLBCL are still important in order to optimize treatment.
Production of reactive oxygen species (ROS) is common to all aerobic cells, but excessive oxidative stress may lead to variable pathological conditions. The most important factor in the redox environment is the creation and elimination of ROS. These are important cellular mediators and their formation is strictly controlled under physiological circumstances. They are mostly formed in the mitochondria as a by-product of oxygen metabolism. The ROS generated in mitochondria plus, for example, hydrogen peroxide and superoxide, can affect cellular signaling pathways by activating signaling cascades or redox-sensitive transcriptional factors. In many pathological conditions, e.g. atherosclerosis, diabetes and cancer, ROS creation and elimination is out of control, leading to excessive amounts [4–8]. Antioxidants are important in the elimination of ROS, thus maintaining the normal physiological state [9].
Redox proteins can be used in the evaluation of oxidative stress. Manganese superoxide dismutase (MnSOD) is a mitochondrial enzyme and it is the most important superoxide dismutase in physiological conditions. Normally, MnSOD makes ROS less harmful by reducing superoxide anions to hydrogen peroxide, which is then neutralized to water and oxygen [10]. Thioredoxin (Trx) functions by reducing oxidized proteins by way of cysteine thiol-disulfide exchange and therefore it limits the damage caused by oxidative stress [11]. Gamma cysteine ligase (GCL) is a rate-limiting enzyme in the creation of glutathione (GSH). Glutathione reduces disulfide bonds and thus repairs oxidative damage by serving as an electron donor [12]. 8-Hydroxydeoxyguanosine (8-OHdG) and nitrotyrosine are markers of oxidative damage. 8-OHdG is an end-product of oxidative damage to DNA [13]. Nitrotyrosine in its free form and in proteins marks oxidative damage to protein structures [14]. Nitrotyrosine can also by itself cause DNA damage [15] and bring about apoptosis [16].
An oxidatively balanced redox status may affect carcinogenesis by modulating DNA in particular, but also other cellular structures [10]. On the other hand, oxidative stress mediates the effects of many cytostatic drugs by causing sublethal DNA damage and thus activating apoptosis. Oxidative stress markers are prognostically important, e.g. in breast cancer [17, 18], ovarian carcinoma [19], head and neck squamous cell carcinoma [20] and acute myeloid leukemia [21]. The prognostic role of oxidative stress in DLBCL has been evaluated in two previous studies in the pre-rituximab era, with conflicting results. The present study was undertaken to evaluate the role of oxidative stress and counteracting enzymes in more detail in DLBCL patients treated with modern immunochemotherapy.
Results
Strong cytoplasmic 8-OHdG staining intensity was associated with extranodal involvement (p = 0.00002) and a high IPI score (divided into two groups, 0-2 and 3-5) (p = 0.002). There were no other significant associations between clinical prognostic parameters and staining intensities of the studied markers. The staining intensities of Trx, GCL and nitrotyrosine correlated with the percentage of malignant positive cells. Intensities were discovered to be better suited to assess survival estimates. Staining patterns were discovered and analyzed in our previous study [22]. The staining intensity of cytoplasmic 8-OHdG correlated with high Trx (p = 0.011) and GCL (p = 0.0003) intensities. There were no other associations between the studied oxidative stress markers and antioxidant enzymes.
Overall 5-year progression-free survival was 81.4% and overall 5-year DLBCL-specific survival was 87.6%. Strong Trx staining intensity was associated with poor progression-free survival (p = 0.046) and poor disease-specific survival (p = 0.015) (Figure 1). The rate of 5-year progression-free survival was 85.1% in patients with negative to moderate Trx intensity and 57.4% in those with strong Trx intensity. Patients with strong cytoplasmic nitrotyrosine immunostaining had poor progression-free survival (p = 0.006; 5-year survival 85.8% in patients with negative to moderate staining and 55.7% in those with strong positivity). Moderate to strong GCL staining intensity was associated with worse prognosis, 5-year progression-free survival being 87.0% versus 70.8% (p = 0.049). Likewise, 5-year disease-specific survival was 94.6% (negative to light GCL immunostaining) versus 77.5% (moderate to strong GCL immunostaining) (p = 0.062). MnSOD and 8-OHdG staining results were not associated with progression-free or disease-specific survival.
Progression-free survival (A) and DLBCL-specific survival (B) of all patients. Strong Trx intensity was associated with both poor progression-free (C) and disease-specific (D) survival. Nitrotyrosine as a marker of nitrosative stress was a marker of poor prognosis (E). GCL-positive patients had worse disease-specific survival (F) and a trend towards shorter disease-specific survival (G). Patients with strong nitrotyrosine and/or Trx expression had significantly worse relapse-free (H) and DLBCL-specific (I) survival than other patients. Trx intensity was a powerful prognostic indicator in the non-GC group (J), but not in patients with GC phenotype.
Patients with either strong Trx or strong nitrotyrosine immunostaining intensities had significantly poorer progression-free survival (p = 0.003) and disease-specific survival (p = 0.031) compared with the other patients. In patients with a non-GC phenotype, strong Trx expression was associated with progression-free survival (p = 0.010); this was not observed in patients with a GC-phenotype. The rate of 5-year progression-free survival was 78.4% in patients with negative to moderate Trx immunostaining and it was 31.6% in those with strong Trx intensity in the non-GC phenotype group.
Discussion
This is the first study in which the prognostic value of oxidative stress markers and antioxidant enzymes in DLBCL patients treated by means of modern immunochemotherapy has been assessed. We discovered that low immunoexpression of GCL, Trx and nitrotyrosine was associated with favorable progression-free survival and Trx was also significant as regards disease-specific survival. Intensive Trx immunostaining also revealed a high-risk group when only non-GC phenotype patients were included. Staining of GCL was almost significant as regards prediction of poor disease-specific survival. Our results suggest that excessive antioxidant and high nitrotyrosine expression are associated with adverse prognosis.
The prognostic role of oxidative stress in lymphomas has been studied previously, with conflicting results. A study by Tome et al. (2005) [23] concerned analysis of the levels of antioxidant enzymes and redox-associated proteins. Their results suggested that the group with the worst prognosis were those with decreased expression of antioxidant enzymes, including catalase, glutathione peroxidase and MnSOD, and increased expression of Trx. In a study by Andreadis et al. (2007) [24], the expression of genes in the glutathione family was examined. Their data suggested that overexpression of these genes correlated with worse prognosis. They used the redox signature score created by Tome et al. [23] and found that their results were exactly the opposite, i.e. overexpression of antioxidants and redox-state proteins correlated with poor prognosis. However, in neither of these studies had the patients received modern immunochemotherapy. Because prognostic markers are highly associated with the therapeutic modality used, the results cannot be extrapolated to patient populations undergoing modern treatments. We have previously carried out thorough evaluation of the expression of oxidative stress markers in different forms of lymphoma. In a recent study [22] we found that high levels of GCL and nitrotyrosine, and also low levels of MnSOD correlated with poor prognosis, but the number of patients with DLBCL in that study was only 18. The aim of the present study was to assess the relationships between antioxidant enzymes, oxidative stress markers and prognosis in cases of diffuse large B-cell lymphoma treated in the rituximab era.
At first glance the results reported by Andreadis et al. and Tome et al. seem to be contradictory, but when evaluating the data according to the expression of individual enzymes, the differences are not so striking. Comparing the results reported by Tome et al. and those in the current study, most are contradictory, as their data indicated that antioxidant function would be a cellular protector. Both our study and theirs showed that strong intensity of Trx was associated with worse prognosis. In the study by Andreadis et al. the authors came to the same conclusion as ourselves, i.e. that the GSH system is related to poor prognosis and excessive antioxidant expression worsens the prognosis. Because the biological functions are complex and antioxidant enzymes may have both positive and negative effects on malignant cell growth, the expression of these markers should probably be analyzed individually and also possibly disease-specifically. Redox state-regulating enzymes may have prognostic value regardless of treatment, since our results are largely in line with those in two previous studies where different treatments were applied. The expression of 8-OHdG, the most commonly used marker of oxidative DNA damage, is a significant prognostic factor in various solid malignancies, but in DLBCL it does not seem to have a prognostic role. Nevertheless, high cytoplasmic 8-OHdG expression, which reflects ROS-derived mitochondrial DNA adduct formation, was associated with features of aggressive disease such as high IPI class and extranodal involvement. Expression of 8-OHdG was associated with high Trx and GCL expression and this suggests therefore that these enzymes might be induced under heavy oxidative stress in DLBCL cells.
Rituximab has revolutionized DLBCL treatment and patient prognosis. However, some patients still succumb to their lymphomas. IPI scoring is at the moment the only clinically relevant prognostic scoring system. Results regarding the prognostic value of gene expression profiling-based grouping are contradictory [25, 26]. Unfortunately, IPI scoring can no longer identify a patient population with a 5-year prognosis of less than 50%. Therefore, reliable biological prognostic factors and especially factors describing basic biological phenomena which might serve as predictors of treatment results are needed. Our results indicate that oxidative stress markers have correlations with prognosis in cases of DLBCL. Preclinical data indicate that GSH induces resistance against key lymphoma chemotherapeutic agents. In vitro, drugs such as indomethacin can counteract this adverse effect by reducing GSH levels [27]. This implies that drugs that suppress GSH might be therapeutically beneficial in lymphomas with high GSH expression. This may also have relevance to the Trx system [28]. Trx is an activator of nuclear factor κB (NF-κB), which inhibits apoptosis and increases proliferation [29]. Non-GC-type DLBCL is characterized by constitutional activation of NF-κB. It has been suggested that high levels of NF-κB may be a sign of adverse prognosis [30, 31]. Our observation of strong Trx intensity and poor prognosis in non-GC phenotype patients might be explained by activation of NF-κB and its anti-apoptotic properties through Trx overexpression.
Resistance to doxorubicin [27] and vincristine [32] has been linked to increased amounts of intracellular GSH. Cyclophosphamide treatment depletes GSH and increases the amount of oxidative stress in human ovarian granulosa cells [33]. Therefore, it is plausible that an increased amount of GSH limits the effectiveness of cyclophosphamide and might be connected to lymphoma chemoresistance. Our results may partly be explained by activation of GCL, which increases the amount of GSH and may therefore bring about resistance to chemotherapy. Doxorubicin sensitivity has also been linked to an excessive amount of Trx [34].
Conclusions
In conclusion, oxidative stress and cellular redox state-regulating enzymes seem to play an important role in DLBCL also in the era of modern therapies. They are of prognostic relevance and may participate in chemoresistance. These results should be authenticated in a prospective study and the role of chemoresistance should be studied in lymphoma cell culture models. If the results can be confirmed in vitro they probably should be taken into account in phase I-II clinical trials dealing with patients with antioxidant enzyme-overexpressing chemoresistant DLBCL.
Methods
Patient material
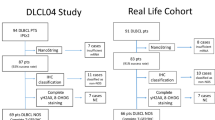
Table 1 summarizes the characteristics of the patients included in the study. There were 106 patients with histologically confirmed DLBCL from whom paraffin-embedded tissue sections from diagnostic lymph nodes, extralymphatic tumor site samples or coarse needle biopsy samples were available. Detailed patient information was collected in each case. The lymphomas were diagnosed and treated at Oulu University Hospital and Kuopio University Hospital between the years 2003-2009. Diagnoses were reviewed by an experienced hematopathologist. The diagnostic work-up included history and physical examination, blood chemistry, bone marrow biopsy and aspiration and whole body computer tomography. The median age of the patients was 64.6 years (21-90 yr). CHOP-like therapy combined with rituximab antibody treatment was given to all patients. Involved field radiotherapy was applied after immunochemotherapy at the sites of bulk disease with residual masses according to individual discretion. DLBCL phenotypes were divided into three groups according to Hans' algorithm: (i) a GCB phenotype with positive CD-10 and/or bcl-6 and negative MUM-1 immunostaining; (ii) a non-GCB phenotype with positive MUM-1 and positive or negative bcl-6 and negative CD-10 immunostaining; (iii) a third type consisting of cases with characteristics of both previous types [2]. The ethical committee of the Northern Ostrobothnia Hospital District has approved the study design (reference number 42/2010).
Immunohistochemical staining and sample evaluation
We used immunohistochemistry to study the expression of 8-OHdG, nitrotyrosine, Trx, MnSOD and GCL, using identical methods as in our recent work with different lymphoma entities. We have previously characterized the expression of the used antibodies in several malignant and pre-malignant tissues [18, 19, 22, 35, 36]. Sample evaluation in lymphomas has also been described earlier [22]. The cytoplasmic expression was diffuse in 8-OHdG, nitrotyrosine, Trx and GCL. MnSOD expression was granulated, in line with its previously described mitochondrial location. The nuclear staining was throughout negative in nitrotyrosine, MnSOD and GCL. 8-OHdG and Trx showed positive and diffuse staining in some of the malignant cells. The nuclear membrane was pronounced in some of the samples stained with 8-OHdG. 8-OHdG and nitrotyrosine expression in malignant cells was uniform. Trx, MnSOD and GCL showed variable intensity in malignant cell staining in few cases. These samples were coded by using the more dominant intensity. The staining results were evaluated only in malignant lymphoma cells, since in our previous work stromal staining extent or intensity did not show any clinical significance. The staining intensity of 8-OHdG, nitrotyrosine, Trx and MnSOD was divided into two groups: negative to moderate, and strong. The staining intensity of cytoplasmic GCL was divided into two groups: negative to light, and moderate to strong. We also created a combination group from Trx and nitrotyrosine immunostaining results: (i) either nitrotyrosine or Trx immunostaining intensity strong; (ii) all other immunostaining results.
Statistical analyses
Progression-free survival was calculated from the date of diagnosis to the date of relapse or date of disease-associated death. Disease-specific survival was calculated from the date of diagnosis to the date of death caused by lymphoma. To assess the relationship between clinical parameters and oxidative stress marker expression levels we used Pearson's chi-square test. Survival estimates were calculated by using Kaplan-Meier analyses and statistical significance was determined by the log-rank test. Values of p under 0.05 were considered statistically significant. All statistical analyses were performed using the Statistical Package for the Social Sciences, v. 18.0 (Chicago, IL, USA).
References
Alizadeh AA, Eisen MB, Davis RE, Ma C, Lossos IS, Rosenwald A, et al.: Distinct types of diffuse large B-cell lymphoma identified by gene expression profiling. Nature 2000, 403: 503–511. 10.1038/35000501
Hans CP, Weisenburger DD, Greiner TC, Gascoyne RD, Delabie J, Ott G, et al.: Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood 2004, 103: 275–282. 10.1182/blood-2003-05-1545
Ziepert M, Hasenclever D, Kuhnt E, Glass B, Schmitz N, Pfreundschuh M, et al.: Standard International prognostic index remains a valid predictor of outcome for patients with aggressive CD20+ B-cell lymphoma in the rituximab era. J Clin Oncol 2010, 28: 2373–2380. 10.1200/JCO.2009.26.2493
Haidari M, Ali M, Gangehei L, Chen M, Zhang W, Cybulsky MI: Increased oxidative stress in atherosclerosis-predisposed regions of the mouse aorta. Life Sci 2010, 87: 100–110. 10.1016/j.lfs.2010.05.016
Doran DE, Weiss D, Zhang Y, Griendling KK, Taylor WR: Differential effects of AT1 receptor and Ca2+ channel blockade on atherosclerosis, inflammatory gene expression, and production of reactive oxygen species. Atherosclerosis 2007, 195: 39–47. 10.1016/j.atherosclerosis.2006.11.030
Baynes JW: Role of oxidative stress in development of complications in diabetes. Diabetes 1991, 40: 405–412. 10.2337/diabetes.40.4.405
Kinnula VL, Crapo JD: Superoxide dismutases in malignant cells and human tumors. Free Radic Biol Med 2004, 36: 718–744. 10.1016/j.freeradbiomed.2003.12.010
Karihtala P, Winqvist R, Syvaoja JE, Kinnula VL, Soini Y: Increasing oxidative damage and loss of mismatch repair enzymes during breast carcinogenesis. Eur J Cancer 2006, 42: 2653–2659. 10.1016/j.ejca.2006.05.037
Mates JM, Segura JA, Alonso FJ, Marquez J: Intracellular redox status and oxidative stress: implications for cell proliferation, apoptosis, and carcinogenesis. Arch Toxicol 2008, 82: 273–299. 10.1007/s00204-008-0304-z
Karihtala P, Soini Y: Reactive oxygen species and antioxidant mechanisms in human tissues and their relation to malignancies. APMIS 2007, 115: 81–103. 10.1111/j.1600-0463.2007.apm_514.x
Holmgren A, Lu J: Thioredoxin and thioredoxin reductase: current research with special reference to human disease. Biochem Biophys Res Commun 2010, 396: 120–124. 10.1016/j.bbrc.2010.03.083
Franklin CC, Backos DS, Mohar I, White CC, Forman HJ, Kavanagh TJ: Structure, function, and post-translational regulation of the catalytic and modifier subunits of glutamate cysteine ligase. Mol Aspects Med 2009, 30: 86–98. 10.1016/j.mam.2008.08.009
Kasai H: Analysis of a form of oxidative DNA damage, 8-hydroxy-2'-deoxyguanosine, as a marker of cellular oxidative stress during carcinogenesis. Mutat Res 1997, 387: 147–163. 10.1016/S1383-5742(97)00035-5
Pfeiffer S, Schmidt K, Mayer B: Dityrosine formation outcompetes tyrosine nitration at low steady-state concentrations of peroxynitrite. Implications for tyrosine modification by nitric oxide/superoxide in vivo. J Biol Chem 2000, 275: 6346–6352. 10.1074/jbc.275.9.6346
Murata M, Kawanishi S: Oxidative DNA damage induced by nitrotyrosine, a biomarker of inflammation. Biochem Biophys Res Commun 2004, 316: 123–128. 10.1016/j.bbrc.2004.02.022
Moulian N, Truffault F, Gaudry-Talarmain YM, Serraf A, Berrih-Aknin S: In vivo and in vitro apoptosis of human thymocytes are associated with nitrotyrosine formation. Blood 2001, 97: 3521–3530. 10.1182/blood.V97.11.3521
Sova H, Jukkola-Vuorinen A, Puistola U, Kauppila S, Karihtala P: 8-Hydroxydeoxyguanosine: a new potential independent prognostic factor in breast cancer. Br J Cancer 2010, 102: 1018–1023. 10.1038/sj.bjc.6605565
Karihtala P, Kauppila S, Soini Y, Jukkola-Vuorinen A: Oxidative stress and counteracting mechanisms in hormone receptor positive, triple-negative and basal-like breast carcinomas. BMC Cancer 2011, 11: 262. 10.1186/1471-2407-11-262
Karihtala P, Soini Y, Vaskivuo L, Bloigu R, Puistola U: DNA adduct 8-hydroxydeoxyguanosine, a novel putative marker of prognostic significance in ovarian carcinoma. Int J Gynecol Cancer 2009, 19: 1047–1051. 10.1111/IGC.0b013e3181ad0f0d
Salzman R, Pacal L, Kankova K, Tomandl J, Horakova Z, Tothova E, et al.: High perioperative level of oxidative stress as a prognostic tool for identifying patients with a high risk of recurrence of head and neck squamous cell carcinoma. Int J Clin Oncol 2010, 15: 565–570. 10.1007/s10147-010-0108-z
Zhou FL, Zhang WG, Wei YC, Meng S, Bai GG, Wang BY, et al.: Involvement of oxidative stress in the relapse of acute myeloid leukemia. J Biol Chem 2010, 285: 15010–15015. 10.1074/jbc.M110.103713
Pasanen AK, Kuitunen H, Haapasaari KM, Karihtala P, Kyllonen H, Soini Y, et al.: Expression and Prognostic Evaluation of Oxidative Stress Markers in an Immunohistochemical Study of B-cell Derived Lymphomas. Leuk Lymphoma, in press.
Tome ME, Johnson DB, Rimsza LM, Roberts RA, Grogan TM, Miller TP, et al.: A redox signature score identifies diffuse large B-cell lymphoma patients with a poor prognosis. Blood 2005, 106: 3594–3601. 10.1182/blood-2005-02-0487
Andreadis C, Gimotty PA, Wahl P, Hammond R, Houldsworth J, Schuster SJ, et al.: Members of the glutathione and ABC-transporter families are associated with clinical outcome in patients with diffuse large B-cell lymphoma. Blood 2007, 109: 3409–3416. 10.1182/blood-2006-09-047621
Gutierrez-Garcia G, Cardesa-Salzmann T, Climent F, Gonzalez-Barca E, Mercadal S, Mate JL, Sancho JM, Arenillas L, Serrano S, Escoda L, Martinez S, Valera A, Martinez A, Jares P, Pinyol M, Garcia-Herrera A, Martinez-Trillos A, Gine E, Villamor N, Campo E, Colomo L, Lopez-Guillermo A, Grup per l'Estudi dels Limfomes de Catalunya I Balears (GELCAB): Gene-expression profiling and not immunophenotypic algorithms predicts prognosis in patients with diffuse large B-cell lymphoma treated with immunochemotherapy. Blood 2011, 117: 4836–4843. 10.1182/blood-2010-12-322362
Ott G, Ziepert M, Klapper W, Horn H, Szczepanowski M, Bernd HW, et al.: Immunoblastic morphology but not the immunohistochemical GCB/nonGCB classifier predicts outcome in diffuse large B-cell lymphoma in the RICOVER-60 trial of the DSHNHL. Blood 2010, 116: 4916–4925. 10.1182/blood-2010-03-276766
Asano T, Tsutsuda-Asano A, Fukunaga Y: Indomethacin overcomes doxorubicin resistance by decreasing intracellular content of glutathione and its conjugates with decreasing expression of gamma-glutamylcysteine synthetase via promoter activity in doxorubicin-resistant leukemia cells. Cancer Chemother Pharmacol 2009, 64: 715–721. 10.1007/s00280-008-0920-6
Zhang H, Go YM, Jones DP: Mitochondrial thioredoxin-2/peroxiredoxin-3 system functions in parallel with mitochondrial GSH system in protection against oxidative stress. Arch Biochem Biophys 2007, 465: 119–126. 10.1016/j.abb.2007.05.001
Hirota K, Murata M, Sachi Y, Nakamura H, Takeuchi J, Mori K, et al.: Distinct roles of thioredoxin in the cytoplasm and in the nucleus. A two-step mechanism of redox regulation of transcription factor NF-kappaB. J Biol Chem 1999, 274: 27891–27897. 10.1074/jbc.274.39.27891
Djavaheri-Mergny M, Javelaud D, Wietzerbin J, Besancon F: NF-kappaB activation prevents apoptotic oxidative stress via an increase of both thioredoxin and MnSOD levels in TNFalpha-treated Ewing sarcoma cells. FEBS Lett 2004, 578: 111–115. 10.1016/j.febslet.2004.10.082
Pavan A, Spina M, Canzonieri V, Sansonno S, Toffoli G, De Re V: Recent prognostic factors in diffuse large B-cell lymphoma indicate NF-kappaB pathway as a target for new therapeutic strategies. Leuk Lymphoma 2008, 49: 2048–2058. 10.1080/10428190802444176
Tsai SY, Sun NK, Lu HP, Cheng ML, Chao CC: Involvement of reactive oxygen species in multidrug resistance of a vincristine-selected lymphoblastoma. Cancer Sci 2007, 98: 1206–1214. 10.1111/j.1349-7006.2007.00513.x
Tsai-Turton M, Luong BT, Tan Y, Luderer U: Cyclophosphamide-induced apoptosis in COV434 human granulosa cells involves oxidative stress and glutathione depletion. Toxicol Sci 2007, 98: 216–230. 10.1093/toxsci/kfm087
Yokomizo A, Ono M, Nanri H, Makino Y, Ohga T, Wada M, et al.: Cellular levels of thioredoxin associated with drug sensitivity to cisplatin, mitomycin C, doxorubicin, and etoposide. Cancer Res 1995, 55: 4293–4296.
Soini Y, Haapasaari KM, Vaarala MH, Turpeenniemi-Hujanen T, Kärjä V, Karihtala P: 8-hydroxydeguanosine and nitrotyrosine are prognostic factors in urinary bladder carcinoma. Int J Clin Exp Pathol 2011, 3: 267–275.
Pylväs M, Puistola U, Kauppila S, Soini Y, Karihtala P: Oxidative stress-induced antioxidant enzyme expression is an early phenomenon in ovarian carcinogenesis. Eur J Cancer 2010, 46: 1661–1667. 10.1016/j.ejca.2010.02.006
Acknowledgements
The authors would like to thank Anne Bisi for her skillful technical assistance. This work was supported by the Cancer Society of Northern Finland (AKP), the Northern Finnish Medical Society Duodecim (OK), the Finnish Medical Foundation (PK) and the Orion-Farmos foundation (PK).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
PP, LL and AKP participated in the design of the study, contributed to the evaluation of immunostainings and drafted the manuscript. KMH, EJ and YS helped in study design, evaluated immunostaining results, and and critically revised the manuscript. TTH contributed to study design and was also responsible for manuscript preparation. RB undertook statistical analyses. PK and OK participated in the design of the study, helped in statistical analyses and wrote the different stages of the manuscript. All authors read and approved the final manuscript.
Outi Kuittinen and Peeter Karihtala contributed equally to this work.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Peroja, P., Pasanen, A.K., Haapasaari, KM. et al. Oxidative stress and redox state-regulating enzymes have prognostic relevance in diffuse large B-cell lymphoma. Exp Hematol Oncol 1, 2 (2012). https://doi.org/10.1186/2162-3619-1-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/2162-3619-1-2