Abstract
Purpose
Increased glycolytic activity with accumulation of extracellular lactate is regarded as a hallmark of cancer. In lymphomas, FDG-PET has undeniable diagnostic and prognostic value, corroborating that these tumours are avid for glucose. However, the role of glycolytic metabolism-related molecules in lymphoma is not well known. Here, we aimed to evaluate the clinical and prognostic significance of a panel of glycolytic metabolism-related molecules in primary non-Hodgkin lymphomas (NHL) and to test in vitro the putative therapeutic impact of lactate transport inhibition.
Methods
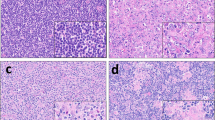
We assessed, by immunohistochemistry, the expression of the metabolism-related molecules MCT1, MCT2, MCT4, CD147, GLUT1, LDHA and CAIX in both tumour and stroma compartments of tissue sections obtained from 104 NHL patients. In addition, the lymphoma-derived cell lines OZ and DOHH-2 were used to evaluate the effect of AZD3965 on their viability and on apoptosis induction, as well as on extracellular lactate accumulation.
Results
We found that expression of MCT1 in the NHL tumour compartment was significantly associated with a poor clinicopathological profile. We also found that MCT4 and CAIX were present in the stromal compartment and correlated with an aggressive phenotype, while MCT1 was absent in this compartment. In addition, we found that AZD3965-mediated disruption of MCT1 activity led to inhibited NHL cell viability and extracellular lactate accumulation, while increasing apoptotic cell death.
Conclusions
Our results indicate that elevated glycolytic activity is associated with NHL aggressiveness, pointing at metabolic cooperation, mediated by MCT1 and MCT4, between tumour cells and their surrounding stroma. MCT1 may serve as a target to treat NHL (diffuse large B cell lymphoma) patients with high MCT1/low MCT4 expressing tumours. Further (pre-)clinical studies are required to allow the design of novel therapeutic strategies aimed at e.g. reprogramming the tumour microenvironment.




Similar content being viewed by others
References
J.O. Armitage, R.D. Gascoyne, M.A. Lunning, F. Cavalli, Non-Hodgkin lymphoma. Lancet 390, 298–310 (2017). https://doi.org/10.1016/S0140-6736(16)32407-2
B.C. Chiu, N. Hou, Epidemiology and etiology of non-hodgkin lymphoma. Cancer Treat Res 165, 1–25 (2015). https://doi.org/10.1007/978-3-319-13150-4_1
J. Ferlay, I. Soerjomataram, R. Dikshit, S. Eser, C. Mathers, M. Rebelo, D.M. Parkin, D. Forman, F. Bray, Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136, E359–E386 (2015). https://doi.org/10.1002/ijc.29210
S.H. Swerdlow, E. Campo, S.A. Pileri, N.L. Harris, H. Stein, R. Siebert, R. Advani, M. Ghielmini, G.A. Salles, A.D. Zelenetz, E.S. Jaffe, The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood 127, 2375–2390 (2016). https://doi.org/10.1182/blood-2016-01-643569
J.O. Armitage, Staging non-Hodgkin lymphoma. CA Cancer J Clin 55, 368–376 (2005)
B.D. Cheson, R.I. Fisher, S.F. Barrington, F. Cavalli, L.H. Schwartz, E. Zucca, T.A. Lister, Alliance, Australasian Leukaemia and Lymphoma Group, Eastern Cooperative Oncology Group, European Mantle Cell Lymphoma Consortium, Italian Lymphoma Foundation, European Organisation for Research, Treatment of Cancer/Dutch Hemato-Oncology Group, Grupo Español de Médula Ósea, German High-Grade Lymphoma Study Group, German Hodgkin’s Study Group, Japanese Lymphoma Study Group, Lymphoma Study Association, NCIC Clinical Trials Group, Nordic Lymphoma Study Group, Southwest Oncology Group, United Kingdom National Cancer Research Institute, Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: The Lugano classification. J Clin Oncol 32, 3059–3068 (2014). https://doi.org/10.1200/JCO.2013.54.8800
A. Gallamini, C. Zwarthoed, A. Borra, Positron emission tomography (PET) in oncology. Cancers 6, 1821–1889 (2014). https://doi.org/10.3390/cancers6041821
M.S. Hofman, R.J. Hicks, How we read oncologic FDG PET/CT. Cancer Imaging 16, 35 (2016). https://doi.org/10.1186/s40644-016-0091-3
T.C. El-Galaly, M. Hutchings, Imaging of non-hodgkin lymphomas: Diagnosis and response-adapted strategies. Cancer Treat Res 165, 125–146 (2015). https://doi.org/10.1007/978-3-319-13150-4_5
P. Johnson, H. McKenzie, How I treat advanced classical Hodgkin lymphoma. Blood 125, 1717–1723 (2015). https://doi.org/10.1182/blood-2014-09-551556
I. Platzek, (18)F-Fluorodeoxyglucose PET/MR imaging in lymphoma. PET Clin 11, 363–373 (2016). https://doi.org/10.1016/j.cpet.2016.05.001
C.L. Wright, J.J. Maly, J. Zhang, M.V. Knopp, Advancing precision nuclear medicine and molecular imaging for lymphoma. PET Clin 12, 63–82 (2017). https://doi.org/10.1016/j.cpet.2016.08.005
K. Miyazaki, Treatment of diffuse large B-cell lymphoma. J Clin Exp Hematop 56, 79–88 (2016). https://doi.org/10.3960/jslrt.56.79
D. Hanahan, R.A. Weinberg, Hallmarks of cancer: The next generation. Cell 144, 646–674 (2011). https://doi.org/10.1016/j.cell.2011.02.013
U.E. Martinez-Outschoorn, M. Peiris-Pages, R.G. Pestell, F. Sotgia, M.P. Lisanti, Cancer metabolism: A therapeutic perspective. Nat Rev Clin Oncol 14, 113 (2017). https://doi.org/10.1038/nrclinonc.2017.1
J.R. Doherty, J.L. Cleveland, Targeting lactate metabolism for cancer therapeutics. J Clin Invest 123, 3685–3692 (2013). https://doi.org/10.1172/JCI69741
U.E. Martinez-Outschoorn, M.P. Lisanti, F. Sotgia, Catabolic cancer-associated fibroblasts transfer energy and biomass to anabolic cancer cells, fueling tumor growth. Semin Cancer Biol 25, 47–60 (2014). https://doi.org/10.1016/j.semcancer.2014.01.005
G. van Niekerk, A.M. Engelbrecht, Role of PKM2 in directing the metabolic fate of glucose in cancer: A potential therapeutic target. Cell Oncol 41, 343–351 (2018). https://doi.org/10.1007/s13402-018-0383-7
J.W. Kim, P. Gao, Y.C. Liu, G.L. Semenza, C.V. Dang, Hypoxia-inducible factor 1 and dysregulated c-Myc cooperatively induce vascular endothelial growth factor and metabolic switches hexokinase 2 and pyruvate dehydrogenase kinase 1. Mol Cell Biol 27, 7381–7393 (2007). https://doi.org/10.1128/MCB.00440-07
A. Le, C.R. Cooper, A.M. Gouw, R. Dinavahi, A. Maitra, L.M. Deck, R.E. Royer, D.L. Vander Jagt, G.L. Semenza, C.V. Dang, Inhibition of lactate dehydrogenase a induces oxidative stress and inhibits tumor progression. Proc Natl Acad Sci U S A 107, 2037–2042 (2010). https://doi.org/10.1073/pnas.0914433107
A. Kumar, S. Kant, S.M. Singh, Novel molecular mechanisms of antitumor action of dichloroacetate against T cell lymphoma: Implication of altered glucose metabolism, pH homeostasis and cell survival regulation. Chem Biol Interact 199, 29–37 (2012). https://doi.org/10.1016/j.cbi.2012.06.005
A. Kumar, S. Kant, S.M. Singh, Antitumor and chemosensitizing action of dichloroacetate implicates modulation of tumor microenvironment: A role of reorganized glucose metabolism, cell survival regulation and macrophage differentiation. Toxicol Appl Pharmacol 273, 196–208 (2013). https://doi.org/10.1016/j.taap.2013.09.005
N.G. Schaefer, J.F. Geschwind, J. Engles, J.W. Buchanan, R.L. Wahl, Systemic administration of 3-bromopyruvate in treating disseminated aggressive lymphoma. Transl Res 159, 51–57 (2012). https://doi.org/10.1016/j.trsl.2011.08.008
J.R. Doherty, C. Yang, K.E. Scott, M.D. Cameron, M. Fallahi, W. Li, M.A. Hall, A.L. Amelio, J.K. Mishra, F. Li, M. Tortosa, H.M. Genau, R.J. Rounbehler, Y. Lu, C.V. Dang, K.G. Kumar, A.A. Butler, T.D. Bannister, A.T. Hooper, K. Unsal-Kacmaz, W.R. Roush, J.L. Cleveland, Blocking lactate export by inhibiting the Myc target MCT1 disables glycolysis and glutathione synthesis. Cancer Res 74, 908–920 (2014). https://doi.org/10.1158/0008-5472.CAN-13-2034
S.H. Swerdlow, E. Campo, N.L.E. Harris, et al., WHO classification of Tumours of Haematopoietic and lymphoid tissues (IARC, Lyon, 2008)
T.A. Lister, D. Crowther, S.B. Sutcliffe, E. Glatstein, G.P. Canellos, R.C. Young, S.A. Rosenberg, C.A. Coltman, M. Tubiana, Report of a committee convened to discuss the evaluation and staging of patients with Hodgkin's disease: Cotswolds meeting. J Clin Oncol 7, 1630–1636 (1989). https://doi.org/10.1200/JCO.1989.7.11.1630
E. Hoster, A. Rosenwald, F. Berger, H.W. Bernd, S. Hartmann, C. Loddenkemper, T.F. Barth, N. Brousse, S. Pileri, G. Rymkiewicz, R. Kodet, S. Stilgenbauer, R. Forstpointner, C. Thieblemont, M. Hallek, B. Coiffier, U. Vehling-Kaiser, R. Bouabdallah, L. Kanz, M. Pfreundschuh, C. Schmidt, V. Ribrag, W. Hiddemann, M. Unterhalt, J.C. Kluin-Nelemans, O. Hermine, M.H. Dreyling, W. Klapper, Prognostic value of Ki-67 index, cytology, and growth pattern in mantle-cell lymphoma: Results from randomized trials of the European mantle cell lymphoma network. J Clin Oncol 34, 1386–1394 (2016). https://doi.org/10.1200/JCO.2015.63.8387
The international non-Hodgkin's lymphoma prognostic factors project, A predictive model for aggressive non-Hodgkin's lymphoma. N Engl J Med 329, 987–994 (1993). https://doi.org/10.1056/NEJM199309303291402
P. Solal-Celigny, Follicular lymphoma international prognostic index. Curr Treat Options in Oncol 7, 270–275 (2006)
M.M. Oken, R.H. Creech, D.C. Tormey, J. Horton, T.E. Davis, E.T. McFadden, P.P. Carbone, Toxicity and response criteria of the eastern cooperative oncology group. Am J Clin Oncol 5, 649–655 (1982)
B.D. Cheson, S.J. Horning, B. Coiffier, M.A. Shipp, R.I. Fisher, J.M. Connors, T.A. Lister, J. Vose, A. Grillo-Lopez, A. Hagenbeek, F. Cabanillas, D. Klippensten, W. Hiddemann, R. Castellino, N.L. Harris, J.O. Armitage, W. Carter, R. Hoppe, G.P. Canellos, Report of an international workshop to standardize response criteria for non-Hodgkin's lymphomas. NCI Sponsored International Working Group. J Clin Oncol 17, 1244 (1999). https://doi.org/10.1200/JCO.1999.17.4.1244
B.D. Cheson, B. Pfistner, M.E. Juweid, R.D. Gascoyne, L. Specht, S.J. Horning, B. Coiffier, R.I. Fisher, A. Hagenbeek, E. Zucca, S.T. Rosen, S. Stroobants, T.A. Lister, R.T. Hoppe, M. Dreyling, K. Tobinai, J.M. Vose, J.M. Connors, M. Federico, V. Diehl, L. International Harmonization, Project on, revised response criteria for malignant lymphoma. J Clin Oncol 25, 579–586 (2007). https://doi.org/10.1200/JCO.2006.09.2403
C. Pinheiro, R.M. Reis, S. Ricardo, A. Longatto-Filho, F. Schmitt, F. Baltazar, Expression of monocarboxylate transporters 1, 2, and 4 in human tumours and their association with CD147 and CD44. J Biomed Biotechnol 2010, 427694 (2010). https://doi.org/10.1155/2010/427694
N.J. Curtis, L. Mooney, L. Hopcroft, F. Michopoulos, N. Whalley, H. Zhong, C. Murray, A. Logie, M. Revill, K.F. Byth, A.D. Benjamin, M.A. Firth, S. Green, P.D. Smith, S.E. Critchlow, Pre-clinical pharmacology of AZD3965, a selective inhibitor of MCT1: DLBCL, NHL and Burkitt's lymphoma anti-tumor activity. Oncotarget 8, 69219–69236 (2017). https://doi.org/10.18632/oncotarget.18215
R.A. Noble, N. Bell, H. Blair, A. Sikka, H. Thomas, N. Phillips, S. Nakjang, S. Miwa, R. Crossland, V. Rand, D. Televantou, A. Long, H.C. Keun, C.M. Bacon, S. Bomken, S.E. Critchlow, S.R. Wedge, Inhibition of monocarboxyate transporter 1 by AZD3965 as a novel therapeutic approach for diffuse large B-cell lymphoma and Burkitt lymphoma. Haematologica 102, 1247–1257 (2017). https://doi.org/10.3324/haematol.2016.163030
S. Granja, D. Tavares-Valente, O. Queiros, F. Baltazar, Value of pH regulators in the diagnosis, prognosis and treatment of cancer. Semin Cancer Biol 43, 17–34 (2017). https://doi.org/10.1016/j.semcancer.2016.12.003
R.S. Jones, M.E. Morris, Monocarboxylate transporters: Therapeutic targets and prognostic factors in disease. Clin Pharmacol Ther 100, 454–463 (2016). https://doi.org/10.1002/cpt.418
V. Miranda-Goncalves, M. Honavar, C. Pinheiro, O. Martinho, M.M. Pires, C. Pinheiro, M. Cordeiro, G. Bebiano, P. Costa, I. Palmeirim, R.M. Reis, F. Baltazar, Monocarboxylate transporters (MCTs) in gliomas: Expression and exploitation as therapeutic targets. Neuro-Oncology 15, 172–188 (2013). https://doi.org/10.1093/neuonc/nos298
F. Morais-Santos, V. Miranda-Goncalves, S. Pinheiro, A.F. Vieira, J. Paredes, F.C. Schmitt, F. Baltazar, C. Pinheiro, Differential sensitivities to lactate transport inhibitors of breast cancer cell lines. Endocr Relat Cancer 21, 27–38 (2014). https://doi.org/10.1530/ERC-13-0132
A. Kumar, S. Kant, S.M. Singh, Targeting monocarboxylate transporter by alpha-cyano-4-hydroxycinnamate modulates apoptosis and cisplatin resistance of Colo205 cells: Implication of altered cell survival regulation. Apoptosis 18, 1574–1585 (2013). https://doi.org/10.1007/s10495-013-0894-7
P. Sonveaux, F. Vegran, T. Schroeder, M.C. Wergin, J. Verrax, Z.N. Rabbani, C.J. De Saedeleer, K.M. Kennedy, C. Diepart, B.F. Jordan, M.J. Kelley, B. Gallez, M.L. Wahl, O. Feron, M.W. Dewhirst, Targeting lactate-fueled respiration selectively kills hypoxic tumor cells in mice. J Clin Invest 118, 3930–3942 (2008). https://doi.org/10.1172/JCI36843
R. Polanski, C.L. Hodgkinson, A. Fusi, D. Nonaka, L. Priest, P. Kelly, F. Trapani, P.W. Bishop, A. White, S.E. Critchlow, P.D. Smith, F. Blackhall, C. Dive, C.J. Morrow, Activity of the monocarboxylate transporter 1 inhibitor AZD3965 in small cell lung cancer. Clin Cancer Res 20, 926–937 (2014). https://doi.org/10.1158/1078-0432.CCR-13-2270
M. Mushtaq, S. Darekar, G. Klein, E. Kashuba, Different mechanisms of regulation of the Warburg effect in Lymphoblastoid and Burkitt lymphoma cells. PLoS One 10, e0136142 (2015). https://doi.org/10.1371/journal.pone.0136142
L. Gan, R. Xiu, P. Ren, M. Yue, H. Su, G. Guo, D. Xiao, J. Yu, H. Jiang, H. Liu, G. Hu, G. Qing, Metabolic targeting of oncogene MYC by selective activation of the proton-coupled monocarboxylate family of transporters. Oncogene 35, 3037–3048 (2016). https://doi.org/10.1038/onc.2015.360
M. Broecker-Preuss, N. Becher-Boveleth, A. Bockisch, U. Duhrsen, S. Muller, Regulation of glucose uptake in lymphoma cell lines by c-MYC- and PI3K-dependent signaling pathways and impact of glycolytic pathways on cell viability. J Transl Med 15(158), 158 (2017). https://doi.org/10.1186/s12967-017-1258-9
C. Pinheiro, V. Penna, F. Morais-Santos, L.F. Abrahao-Machado, G. Ribeiro, E.C. Curcelli, M.V. Olivieri, S. Morini, I. Valenca, D. Ribeiro, F.C. Schmitt, R.M. Reis, F. Baltazar, Characterization of monocarboxylate transporters (MCTs) expression in soft tissue sarcomas: Distinct prognostic impact of MCT1 sub-cellular localization. J Transl Med 12, 118 (2014). https://doi.org/10.1186/1479-5876-12-118
U.E. Martinez-Outschoorn, D. Whitaker-Menezes, M. Valsecchi, M.P. Martinez-Cantarin, A. Dulau-Florea, J. Gong, A. Howell, N. Flomenberg, R.G. Pestell, J. Wagner, C. Arana-Yi, M. Sharma, F. Sotgia, M.P. Lisanti, Reverse Warburg effect in a patient with aggressive B-cell lymphoma: Is lactic acidosis a paraneoplastic syndrome? Semin Oncol 40, 403–418 (2013). https://doi.org/10.1053/j.seminoncol.2013.04.016
M. Gooptu, D. Whitaker-Menezes, J. Sprandio, M. Domingo-Vidal, Z. Lin, G. Uppal, J. Gong, R. Fratamico, B. Leiby, A. Dulau-Florea, J. Caro, U. Martinez-Outschoorn, Mitochondrial and glycolytic metabolic compartmentalization in diffuse large B-cell lymphoma. Semin Oncol 44, 204–217 (2017). https://doi.org/10.1053/j.seminoncol.2017.10.002
L. Mikkilineni, D. Whitaker-Menezes, M. Domingo-Vidal, J. Sprandio, P. Avena, P. Cotzia, A. Dulau-Florea, J. Gong, G. Uppal, T. Zhan, B. Leiby, Z. Lin, B. Pro, F. Sotgia, M.P. Lisanti, U. Martinez-Outschoorn, Hodgkin lymphoma: A complex metabolic ecosystem with glycolytic reprogramming of the tumor microenvironment. Semin Oncol 44, 218–225 (2017). https://doi.org/10.1053/j.seminoncol.2017.10.003
M.I. Mitchell, A.M. Engelbrecht, Metabolic hijacking: A survival strategy cancer cells exploit? Crit Rev Oncol Hematol 109, 1–8 (2017). https://doi.org/10.1016/j.critrevonc.2016.11.010
P. Nilendu, S.C. Sarode, D. Jahagirdar, I. Tandon, S. Patil, G.S. Sarode, J.K. Pal, N.K. Sharma, Mutual concessions and compromises between stromal cells and cancer cells: Driving tumor development and drug resistance. Cell Oncol 41, 353–367 (2018). https://doi.org/10.1007/s13402-018-0388-2
N. Pertega-Gomes, J.R. Vizcaino, C. Gouveia, C. Jeronimo, R.M. Henrique, C. Lopes, F. Baltazar, Monocarboxylate transporter 2 (MCT2) as putative biomarker in prostate cancer. Prostate 73, 763–769 (2013). https://doi.org/10.1002/pros.22620
S.P. Mathupala, P. Parajuli, A.E. Sloan, Silencing of monocarboxylate transporters via small interfering ribonucleic acid inhibits glycolysis and induces cell death in malignant glioma: An in vitro study. Neurosurgery 55, 1410–1419; discussion 1419 (2004)
A. Giatromanolaki, E. Sivridis, S. Arelaki, M.I. Koukourakis, Expression of enzymes related to glucose metabolism in non-small cell lung cancer and prognosis. Exp Lung Res 43(1–8), 167–174 (2017). https://doi.org/10.1080/01902148.2017.1328714
D.E. Jung, J.M. Kim, C. Kim, S.Y. Song, Embigin is overexpressed in pancreatic ductal adenocarcinoma and regulates cell motility through epithelial to mesenchymal transition via the TGF-beta pathway. Mol Carcinog 55, 633–645 (2016). https://doi.org/10.1002/mc.22309
C. Pinheiro, A. Longatto-Filho, C. Scapulatempo, L. Ferreira, S. Martins, L. Pellerin, M. Rodrigues, V.A. Alves, F. Schmitt, F. Baltazar, Increased expression of monocarboxylate transporters 1, 2, and 4 in colorectal carcinomas. Virchows Arch 452, 139–146 (2008). https://doi.org/10.1007/s00428-007-0558-5
C. Pinheiro, S. Granja, A. Longatto-Filho, A.M. Faria, M.C. Fragoso, S.M. Lovisolo, A.M. Lerario, M.Q. Almeida, F. Baltazar, M.C. Zerbini, Metabolic reprogramming: A new relevant pathway in adult adrenocortical tumors. Oncotarget 6, 44403–44421 (2015). https://doi.org/10.18632/oncotarget.5623
I. Valenca, N. Pertega-Gomes, J.R. Vizcaino, R.M. Henrique, C. Lopes, F. Baltazar, D. Ribeiro, Localization of MCT2 at peroxisomes is associated with malignant transformation in prostate cancer. J Cell Mol Med 19, 723–733 (2015). https://doi.org/10.1111/jcmm.12481
R. Karmali, L.I. Gordon, Molecular subtyping in diffuse large B cell lymphoma: Closer to an approach of precision therapy. Curr Treat Options in Oncol 18, 11 (2017). https://doi.org/10.1007/s11864-017-0449-1
B. Kubuschok, G. Held, M. Pfreundschuh, Management of diffuse large B-cell lymphoma (DLBCL). Cancer Treat Res 165, 271–288 (2015). https://doi.org/10.1007/978-3-319-13150-4_11
F. Morais-Santos, S. Granja, V. Miranda-Goncalves, A.H. Moreira, S. Queiros, J.L. Vilaca, F.C. Schmitt, A. Longatto-Filho, J. Paredes, F. Baltazar, C. Pinheiro, Targeting lactate transport suppresses in vivo breast tumour growth. Oncotarget 6, 19177–19189 (2015). https://doi.org/10.18632/oncotarget.3910
A.P. Halestrap, The SLC16 gene family - structure, role and regulation in health and disease. Mol Asp Med 34, 337–349 (2013). https://doi.org/10.1016/j.mam.2012.05.003
X. Xin, X. Zeng, H. Gu, M. Li, H. Tan, Z. Jin, T. Hua, R. Shi, H. Wang, CD147/EMMPRIN overexpression and prognosis in cancer: A systematic review and meta-analysis. Sci Rep 6, 32804 (2016). https://doi.org/10.1038/srep32804
I. Marchiq, J. Albrengues, S. Granja, C. Gaggioli, J. Pouyssegur, M.P. Simon, Knock out of the BASIGIN/CD147 chaperone of lactate/H+ symporters disproves its pro-tumour action via extracellular matrix metalloproteases (MMPs) induction. Oncotarget 6, 24636–24648 (2015). https://doi.org/10.18632/oncotarget.4323
M.G. Slomiany, G.D. Grass, A.D. Robertson, X.Y. Yang, B.L. Maria, C. Beeson, B.P. Toole, Hyaluronan, CD44, and emmprin regulate lactate efflux and membrane localization of monocarboxylate transporters in human breast carcinoma cells. Cancer Res 69, 1293–1301 (2009). https://doi.org/10.1158/0008-5472.CAN-08-2491
J. Afonso, L.L. Santos, V. Miranda-Goncalves, A. Morais, T. Amaro, A. Longatto-Filho, F. Baltazar, CD147 and MCT1-potential partners in bladder cancer aggressiveness and cisplatin resistance. Mol Carcinog 54, 1451–1466 (2014). https://doi.org/10.1002/mc.22222
J. Hao, M.C. Madigan, A. Khatri, C.A. Power, T.T. Hung, J. Beretov, L. Chang, W. Xiao, P.J. Cozzi, P.H. Graham, J.H. Kearsley, Y. Li, In vitro and in vivo prostate cancer metastasis and chemoresistance can be modulated by expression of either CD44 or CD147. PLoS One 7, e40716 (2012). https://doi.org/10.1371/journal.pone.0040716
H. Gao, Q. Jiang, Y. Han, J. Peng, C. Wang, shRNA-mediated EMMPRIN silencing inhibits human leukemic monocyte lymphoma U937 cell proliferation and increases chemosensitivity to adriamycin. Cell Biochem Biophys 71, 827–835 (2015). https://doi.org/10.1007/s12013-014-0270-4
J. Schmidt, I. Bonzheim, J. Steinhilber, I.A. Montes-Mojarro, C. Ortiz-Hidalgo, W. Klapper, F. Fend, L. Quintanilla-Martinez, EMMPRIN (CD147) is induced by C/EBPbeta and is differentially expressed in ALK+ and ALK- anaplastic large-cell lymphoma. Lab Invest 97, 1095–1102 (2017). https://doi.org/10.1038/labinvest.2017.54
Y. Watanabe, H. Suefuji, Y. Hirose, H. Kaida, G. Suzuki, J. Uozumi, E. Ogo, M. Miura, K. Takasu, K. Miyazaki, K. Nakahara, M. Ishibashi, T. Okamura, K. Ohshima, N. Hayabuchi, 18F-FDG uptake in primary gastric malignant lymphoma correlates with glucose transporter 1 expression and histologic malignant potential. Int J Hematol 97, 43–49 (2013). https://doi.org/10.1007/s12185-012-1225-4
Y.M. Liu, X.M. Zhai, Y.W. Wu, Biological correlation between glucose transporters, Ki-67 and 2-deoxy-2-[18F]-fluoro-D-glucose uptake in diffuse large B-cell lymphoma and natural killer/T-cell lymphoma. Genet Mol Res 15 (2016). https://doi.org/10.4238/gmr.15027242
H.K. Shim, W.W. Lee, S.Y. Park, H. Kim, Y. So, S.E. Kim, Expressions of glucose transporter types 1 and 3 and hexokinase-II in diffuse large B-cell lymphoma and other B-cell non-Hodgkin's lymphomas. Nucl Med Biol 36, 191–197 (2009). https://doi.org/10.1016/j.nucmedbio.2008.11.009
V. Jurisic, S. Radenkovic, G. Konjevic, The actual role of LDH as tumor marker, Biochemical and Clinical Aspects. Adv Exp Med Biol 867, 115–124 (2015). https://doi.org/10.1007/978-94-017-7215-0_8
F. Petrelli, M. Cabiddu, A. Coinu, K. Borgonovo, M. Ghilardi, V. Lonati, S. Barni, Prognostic role of lactate dehydrogenase in solid tumors: A systematic review and meta-analysis of 76 studies. Acta Oncol 54, 961–970 (2015). https://doi.org/10.3109/0284186X.2015.1043026
W. Hu, X. Wang, R. Yang, Evaluation of D-dimer and lactate dehydrogenase plasma levels in patients with relapsed acute leukemia. Oncol Lett 12, 591–596 (2016). https://doi.org/10.3892/ol.2016.4657
B.M. William, N.R. Bongu, M. Bast, R.G. Bociek, P.J. Bierman, J.M. Vose, J.O. Armitage, The utility of lactate dehydrogenase in the follow up of patients with diffuse large B-cell lymphoma. Rev Bras Hematol Hemoter 35, 189–191 (2013). https://doi.org/10.5581/1516-8484.20130055
R. Lu, M. Jiang, Z. Chen, X. Xu, H. Hu, X. Zhao, X. Gao, L. Guo, Lactate dehydrogenase 5 expression in non-Hodgkin lymphoma is associated with the induced hypoxia regulated protein and poor prognosis. PLoS One 8, e74853 (2013). https://doi.org/10.1371/journal.pone.0074853
S.J. van Kuijk, A. Yaromina, R. Houben, R. Niemans, P. Lambin, L.J. Dubois, Prognostic significance of carbonic anhydrase IX expression in Cancer patients: A meta-analysis. Front Oncol 6, 69 (2016). https://doi.org/10.3389/fonc.2016.00069
L.Q. Chen, C.M. Howison, C. Spier, A.T. Stopeck, S.W. Malm, M.D. Pagel, A.F. Baker, Assessment of carbonic anhydrase IX expression and extracellular pH in B-cell lymphoma cell line models. Leuk Lymphoma 56, 1432–1439 (2015). https://doi.org/10.3109/10428194.2014.933218
J. Afonso, L.L. Santos, A. Morais, T. Amaro, A. Longatto-Filho, F. Baltazar, Metabolic coupling in urothelial bladder cancer compartments and its correlation to tumor aggressiveness. Cell Cycle 15, 368–380 (2016). https://doi.org/10.1080/15384101.2015.1121329
M. Beloueche-Babari, S. Wantuch, T. Casals Galobart, M. Koniordou, H.G. Parkes, V. Arunan, Y.L. Chung, T.R. Eykyn, P.D. Smith, M.O. Leach, MCT1 inhibitor AZD3965 increases mitochondrial metabolism, facilitating combination therapy and noninvasive magnetic resonance spectroscopy. Cancer Res 77, 5913–5924 (2017). https://doi.org/10.1158/0008-5472.CAN-16-2686
S.E.R. Halford, P. Jones, S. Wedge, S. Hirschberg, S. Katugampola, G. Veal, G. Payne, C. Bacon, S. Potter, M. Griffin, M. Chenard-Poirier, G. Petrides, G. Holder, H.C. Keun, U. Banerji, E.R. Plummer, A first-in-human first-in-class (FIC) trial of the monocarboxylate transporter 1 (MCT1) inhibitor AZD3965 in patients with advanced solid tumours. J Clin Oncol 35, 2516–2516 (2017). https://doi.org/10.1200/JCO.2017.35.15_suppl.2516
R. Le Floch, J. Chiche, I. Marchiq, T. Naiken, K. Ilc, C.M. Murray, S.E. Critchlow, D. Roux, M.P. Simon, J. Pouyssegur, CD147 subunit of lactate/H+ symporters MCT1 and hypoxia-inducible MCT4 is critical for energetics and growth of glycolytic tumors. Proc Natl Acad Sci U S A 108, 16663–16668 (2011). https://doi.org/10.1073/pnas.1106123108
J. Barretina, G. Caponigro, N. Stransky, K. Venkatesan, A.A. Margolin, S. Kim, C.J. Wilson, J. Lehar, G.V. Kryukov, D. Sonkin, A. Reddy, M. Liu, L. Murray, M.F. Berger, J.E. Monahan, P. Morais, J. Meltzer, A. Korejwa, J. Jane-Valbuena, F.A. Mapa, J. Thibault, E. Bric-Furlong, P. Raman, A. Shipway, I.H. Engels, J. Cheng, G.K. Yu, J. Yu, P. Aspesi Jr., M. de Silva, K. Jagtap, M.D. Jones, L. Wang, C. Hatton, E. Palescandolo, S. Gupta, S. Mahan, C. Sougnez, R.C. Onofrio, T. Liefeld, L. MacConaill, W. Winckler, M. Reich, N. Li, J.P. Mesirov, S.B. Gabriel, G. Getz, K. Ardlie, V. Chan, V.E. Myer, B.L. Weber, J. Porter, M. Warmuth, P. Finan, J.L. Harris, M. Meyerson, T.R. Golub, M.P. Morrissey, W.R. Sellers, R. Schlegel, L.A. Garraway, The Cancer cell line encyclopedia enables predictive modelling of anticancer drug sensitivity. Nature 483, 603–607 (2012). https://doi.org/10.1038/nature11003
Acknowledgements
This work was developed under the scope of project NORTE-01-0145-FEDER- 000013, supported by the Northern Portugal Regional Operational Programme (NORTE 2020) under the Portugal Partnership Agreement, through the European Regional Development Fund (FEDER), and through the Competitiveness Factors Operational Programme (COMPETE) and by National funds, through the Foundation for Science and Technology (FCT), under the scope of project POCI-01-0145-FEDER-007038. JA received a fellowship from FCT, ref. SFRH/BPD/116784/2016.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest to disclose.
Research involving human participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of (retrospective) study formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 282 kb)
Rights and permissions
About this article
Cite this article
Afonso, J., Pinto, T., Simões-Sousa, S. et al. Clinical significance of metabolism-related biomarkers in non-Hodgkin lymphoma – MCT1 as potential target in diffuse large B cell lymphoma. Cell Oncol. 42, 303–318 (2019). https://doi.org/10.1007/s13402-019-00426-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13402-019-00426-2