Abstract
Background
Pancreatic cancer (PC) is considered the most lethal cancer and approximately 10% of PC is hereditary. The purpose of the study was to assess attitudes of at-risk family members with two or more relatives affected with pancreas cancer (PC) toward PC risk and future screening options.
Methods
At-risk family members and primary care controls were surveyed regarding perceived PC risk, PC worry/concern, attitude toward cancer screening, screening test accuracy, and intentions regarding PC screening via blood testing or more invasive endoscopic ultrasound (EUS).
Results
PC family members reported greater perceived risk of PC than controls (54% vs. 6%, respectively, p < 0.0001). PC family members also reported higher levels of PC worry/concern than controls (p < 0.0001), although 19% of PC family members indicated they were “not at all concerned” about getting PC. PC family members indicated greater acceptance of a false-negative result on a PC screening test relative to controls (12% vs. 8%, p = 0.02). Both groups reported high (>89%) receptivity to the potential PC screening options presented, though receptivity was greater among PC family members as compared to controls (p < 0.0001) for EUS. In multivariable analyses, degree of PC concern (p < 0.0001) was associated with intention to screen for PC by blood test and EUS, while perceived PC risk was associated with likelihood of undergoing EUS only (p < 0.0001).
Conclusions
Receptivity to screening options for PC appears high. Clinicians should address behavioral and genetic risk factors for PC and foster appropriate concern regarding PC risk among at-risk individuals.
Similar content being viewed by others
Introduction
Pancreatic cancer (PC) is the fourth leading cause of cancer death among men and women in the U.S. [1]. The incidence rates of PC have increased by 1.5% per year since 2004, and in 2012, it is estimated that there will be 43,920 new cases of PC and 37,390 deaths due to this disease [1]. The lifetime risk of PC is about 1 in 71 for males and females [1]. For all stages combined, the 5-year relative survival rate is 6% with survival at earlier stages being 22% [1]. The causes of this deadly disease are not well understood, but approximately 10% of pancreatic cancer is hereditary [2], and a person’s chance of developing this cancer increases two- to three-fold if a first-degree relative (parent, sibling or child) has PC [3]. Presently, the United States Preventive Services Task Force (USPSTF) recommends against routine screening for PC in the general population because of the low prevalence of this malignancy, the limited accuracy and invasiveness of the currently available tests, and the poor outcomes of treatment [4]. However, screening at-risk individuals is receiving increasing support [5–8] with a recommended threshold to offer screening to those who carry a ≥10-fold increased risk [9].
Recent advances in screening technology via serum or stool tests or endoscopic ultrasound (EUS) hold promise for detecting early-stage PC [10–15]. A blood or stool test for early detection of PC would be preferable to EUS because of lower invasiveness and cost, however, biomarkers for PC are elusive and the efficacy of emerging potential serum or stool panels remains unknown with regard to early detection. The ability of EUS to assist in diagnosing pancreatic malignancies has also been demonstrated [16–19]. However, concerns with EUS relate to its invasive nature, cost, accuracy and availability [16]. At the present time, blood and stool tests and EUS remain areas of research as potential screening tools for PC. Studies are underway to provide a stronger rationale for their use among appropriate groups at particular risk for developing PC [20, 21], including a recent report addressing the psychological impact of PC surveillance among at-risk participants in a Dutch PC surveillance study [22]. This study, which included only at-risk individuals who already agreed to surveillance, demonstrated that surveillance was not associated with increased cancer worry or elevated anxiety or depression levels [22]. Understanding the perceptions of at-risk, unaffected PC family members who are not enrolled in surveillance regarding future screening options is important and comparing their perceptions to individuals not at particular risk of PC would fill an existing gap in the literature.
The objective of this study was to evaluate perceived PC risk, PC worry and concern, and receptivity to future PC screening options among at-risk unaffected family members of individuals with PC relative to individuals (controls) who more closely resemble the PC risk profile for the general population. Individuals with a family history of cancer may overestimate their personal cancer risk and report increased cancer-related worry or concern; these factors may in turn positively or negatively influence attitudes and behaviors toward screening among this higher-risk group [23–28]. Furthermore, this study sought to identify factors related to interest in screening for PC and to assess expectations surrounding the accuracy of PC screening tests.
Materials and methods
Study population and study procedures
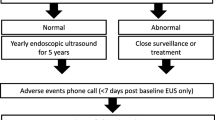
All study procedures were approved by the Mayo Clinic Institutional Review Board and all subjects provided written informed consent to participate. Study subjects were at-risk unaffected family members enrolled in the Mayo Clinic Pancreatic Cancer Family Study, a study conducted as part of the Specialized Program of Research Excellence (SPORE) and Pancreatic Cancer Genetic Epidemiology Consortium studies [3, 29] as well as primary care controls. At-risk family members included those with two or more first- or second-degree relatives affected with pancreatic adenocarcinoma. Control subjects included those attending Mayo Clinic for a general medical exam. Relatives of individuals with PC and controls comprising the comparison group for this study were recruited from 4/27/2004 -1/24/2008. All participants completed a survey addressing perceived PC risk, degree of PC worry/concern, attitude toward cancer screening in general, and intentions regarding uptake of PC screening if it were available as a blood test or endoscopic ultrasound (EUS).
Measures
Demographic and medical history data were collected using a self-report survey instrument. The instrument included items assessing age, sex, race/ethnicity, education, smoking status (current, ever, never), household income, and number of family members affected by cancer.
Perceived risk of PC was assessed in absolute and comparative terms [30]. Specifically, the item “How likely do you think it is that you will get pancreatic cancer sometime in your life?” was used to assess absolute perceived risk. Response options on a 5-point scale ranged from “very likely” to “very unlikely.” Responses were grouped for analysis to reflect “likely” (including the responses “very likely” and “likely”) and “unlikely” (including the responses “no feeling or opinion,” “unlikely,” and “very unlikely”). Comparative risk perception was assessed by the item: “Compared to most people of your same age, sex, and race, what do you think your chances are of getting pancreatic cancer sometime in your life?” Response options included (1) “much higher” chance to (5) “much lower” chance.
Pancreatic cancer worry and concern was assessed by four items adapted from Lerman and colleagues [31]. Three items referred to the time period “during the past month” and queried: “How often have you thought about your chances of getting pancreatic cancer?” “How often have thoughts about your chances of getting pancreatic cancer affected your mood?” and “How often have thoughts about your chances of getting pancreatic cancer affected your ability to perform your daily activities?” Response options included “not at all or rarely,” “sometimes,” “often,” and “a lot”. A fourth item queried: “How concerned are you about getting pancreatic cancer?” to which participants responded using a 4-point Likert-type scale ranging from (1) “extremely concerned” to (4) “not at all concerned”. Cronbach’s alpha for these items was 0.78, demonstrating acceptable internal consistency. For multivariable analysis, responses were categorized as “concerned” (“extremely”/“moderately”) or “not concerned” (“mildly”/“not at all”) for ease of interpretation.
Participants’ willingness to take part in PC screening if it were a blood test or EUS was assessed by two items, using a four-point Likert response format with responses ranging from “very unlikely” to “very likely”. The questions read, “If a blood test were available to screen for pancreatic cancer, how likely is it that you would take it?” and “If a test were available to screen for pancreatic cancer that required an upper endoscopic examination (you would be sedated, or made drowsy, and a flexible tube would be inserted through your mouth into your stomach), how likely is it that you would take it?”
As data are not yet available regarding actual false-negative or false-positive rates for PC screening tests and the concepts themselves can be difficult to understand [32], expectations surrounding the accuracy of a PC screening test were assessed more generally. The following three items were presented: “It would be OK if a test detects less than 100% of people who have pancreatic cancer,” “If a test says I do NOT have pancreatic cancer when I really DO, that is OK with me,” (false-negative) and “If a test says I may have pancreatic cancer when I really do NOT, that is OK with me” (false-positive). A fourth item addressed cancer screening more generally: “It would be OK if a test says cancer may be present in a person who really does NOT have cancer.” These four items were assessed using a “strongly agree” to “strongly disagree” rating scale with a “do not know” option.
Statistical analysis
Data were descriptively summarized using frequencies and percentages for categorical variables, and means and standard deviations for continuous variables. Comparisons between group (PC family members or controls) and psychosocial characteristics, likelihood to undergo screening, and expectations of screening accuracy were evaluated using multivariable logistic regression adjusting for sex, age, smoking, and family history (first degree relatives) of any cancer; odds ratios and 95% confidence intervals (CI) are presented. Because multiple members from the same family could participate in the PC family member group, analyses were also conducted which accounted for possible non-independence using generalized estimating equation (GEE) methodology. Family-specific correlations for screening via blood test and EUS were modeled using an exchangeable covariance matrix. All statistical analyses were performed using SAS 9.2 (SAS Institute Inc., Cary, NC).
Results
Sample characteristics
A total of 378 PC family members and 1528 controls consented and were sent a survey; 361 (96%) PC family members (representing 115 different families) and 1045 (68%) controls completed the survey. Mean ages in the two groups were 53.7 (±14.6) and 65.6 (±10.7) years, respectively (p < 0.001). Relative to controls, PC family members were younger, more likely to be female, current smokers, and have more first degree relatives with any cancer (Table 1).
Perceived pancreatic cancer risk
A majority (54%) of PC family members reported that they were likely to get PC in their lifetime relative to 6% of controls (p < 0.0001). A similar pattern was observed for comparative risk estimates, i.e., perceptions of risk relative to most people of the same age, sex, and race, with a majority (67%) of PC family members reporting a greater risk vs. 5% of controls (p < 0.0001) (Table 2).
Pancreatic cancer related worry/concern
PC family members reported more frequent thoughts in the past month about getting PC (47% vs. 5%, respectively, p < 0.0001), with these thoughts affecting mood. Overall, 81% of PC family members reported some degree of concern (“extreme,” “moderate,” or “mild”) about getting PC relative to 41% of controls, (p < 0.0001) (Table 2).
Expectations surrounding screening test accuracy
A majority (>75%) of both PC family members and controls expressed acceptance of a PC screening test that was not 100% accurate (Table 3). PC family members indicated greater acceptance of a false-negative result on a PC screening test relative to controls (12% vs. 8%, p = 0.002). Acceptance rates for false-positive test results were slightly higher overall than acceptance rates for false-negatives; however no differences were observed between the two groups with regard to acceptance of false-positive results both for a cancer screening test in general, and a screening test for PC (both p > 0.05; Table 3).
Likelihood of undergoing PC screening
Overall, 89% of controls and 95% of PC family members reported that they were “likely” or “extremely likely” to undergo PC screening via a blood test (p = 0.08). Although these rates were comparatively lower for PC screening via EUS, (55% of controls and 75% of PC family members), likelihood of uptake was higher in the PC family member group relative to controls (p < 0.0001). Those who were “likely” vs. “not likely” to undergo PC screening via a blood test differed by group (PC family member vs. control) (p = 0.007), age (p = .001), perceived PC risk (p < 0.0001), and degree of cancer worry/concern (p < 0.0001) in univariable analyses (Table 4). In a multivariable logistic regression model, the likelihood of screening for PC via a blood test was associated with greater degree of cancer worry/concern (p < 0.0001). Group, age, and perceived PC risk were no longer independently associated with screening likelihood by blood test.
Similar analyses were conducted with regard to the likelihood of undergoing screening via EUS. In univariable analyses, likelihood of screening via EUS was associated with the same factors as screening via a blood test: group (p < 0.0001), age (p = 0.002), perceived PC risk (p < 0.0001), and degree of cancer worry/concern (p < 0.0001) (Table 5). In the multivariable context, only perceived PC risk (p < 0.0001) and degree of cancer worry/concern (p < 0.0001) remained significant. Analyses accounting for the possibility that data are correlated within a family did not appreciably change results in any of the models (results not shown).
Discussion
Comprehensive efforts are underway to better understand the etiology of PC, to improve treatment outcomes, and to develop and evaluate effective screening technologies [8, 33]. Receptivity toward potential future screening options for pancreatic cancer among those at significant risk is an important, yet understudied area. Overall, receptivity toward screening was higher among PC family members relative to controls; of the potential screening options studied, receptivity was greater for the less invasive method (blood test vs. EUS). These findings are consistent with qualitative data reported by Lewis [34] and are important with regard to developing early detection methods that will be acceptable to the individuals for whom they are intended. Previous studies including highly-selected, at-risk individuals have reported actual uptake of PC screening ranging between 61% (for EUS) and 67% (for MRI), which reflects variation in individual preferences and provides evidence that uptake cannot always be assumed [6, 8]. Moreover, this study established that individuals who have family members with PC may exhibit greater worry and concern about PC, perceive greater PC risk for themselves and that these psychological responses are independent, positive predictors of intention to undergo screening for PC via blood test (worry/concern) and EUS (worry/concern and perceived risk) were such screening tests to become available in the future.
These findings are consistent with theoretical models of voluntary health behavior that include the construct of perceived vulnerability, such as protection motivation theory [35] and the health belief model [36, 37]. Specifically, these models posit that willingness to undergo invasive procedures would be less likely for an average risk group of individuals, while those with heightened risk perception, greater perceived susceptibility or vulnerability and increased awareness of the severity of the target disease, would express greater likelihood of undergoing even an invasive screening test such as EUS. In this investigation, it was these psychological constructs that were predictive of likelihood of screening in the multivariable context, not group status, suggesting that at-risk individuals (PC family members) who fail to recognize their vulnerability may be no more likely than average-risk individuals (controls) to undergo screening. This point underscores the importance of understanding the nature of risk perception and concern in cancer screening and the importance of allowing such perceptions to appropriately drive screening behavior. It also underscores the importance of appropriate education on risk to family members. In this study, individuals who perceived themselves as likely to get PC in their lifetime were over three times as likely as those who did not hold this perception to be willing to undergo EUS screening, irrespective of group status. Thus, there is a great need to measure and understand the complexities of these constructs more fully in future research on PC, perhaps using multi-dimensional measures of risk beliefs such as the one developed by Hay and colleagues [38, 39].
In this study, PC family members perceived their risk of developing PC during their lifetime as greater compared to others of their same age, sex, and race. They also reported significantly higher levels of PC-related thoughts and concerns. These findings are consistent with the literature on perceived risk and concern among those at increased risk of cancer due to family history. However, previous studies have focused primarily on breast, colorectal, and lung cancer [32, 40–42]. PC is different from these cancers in that there are currently no recommended screening options, and, while there are lifestyle-related factors that affect PC risk such as obesity [43] and cigarette smoking [44], no single factor has been identified that can dramatically reduce risk. Given the current limitations of the science of PC prevention, methods of early detection are needed.
Interestingly in this study, nearly 1 in 5 PC family members indicated they were “not at all worried” about getting PC. This finding could reflect lack of awareness regarding familial risk, a general belief that worry is unproductive, illusion of unique invulnerability [45, 46] or a sense of futility in worrying about this deadly disease based on experience with a family member. Each of these possible explanations warrants empirical study, as lack of worry/concern could lead to complacency among a group of individuals who may benefit greatly from vigilance regarding early warning signs or heightened awareness of developments in screening. Patient education regarding PC risk and recommendations for surveillance among those at high risk is needed [34].
Sensitivity and specificity of screening tests are sophisticated, yet critical concepts for patients to understand prior to undergoing a screening test. The difference observed in this study between PC family members and controls with regard to acceptance of false negatives is a novel finding warranting further study. Greater acceptance of personal false negative test results among PC family members may reflect an experiential bias (relative to controls) that treatment is only rarely successful in changing the course of the disease, thus, “missing” the diagnosis can be viewed with greater acceptance. This interpretation, if valid, may reflect both cognitive (actual knowledge-based) and affective (emotional) responses resulting from experience with the course of PC in their family member. This same logic would support the trend-level findings observed regarding greater global acceptance of missing a diagnosis of PC among PC family members as compared to controls.
This research has several strengths including its focus on cancer of the pancreas, which remains the deadliest cancer. In addition, this research is one of the few psychosocial studies involving a relatively large sample of PC family members that also includes a control group. Finally, the importance and timeliness of the research cannot be understated; the incidence of PC is continuing to rise and effective screening methods are the focus of ongoing translational research. Despite these strengths, several limitations are important to note including non-independence that was unique to the PC family sample. Statistical approaches such as GEE can account for non-independence, but our findings should still be interpreted with caution. Moreover, PC families with BRCA1/2 and CDKN2A mutations were not excluded from the study; these families may have greater familiarity with cancer screening tests and their attitudes may differ in important ways from other PC family members. Second, this was a cross-sectional study assessing behavioral intentions toward hypothetical screening tests; it is inappropriate and premature to extrapolate these findings to future participation in screening tests for pancreatic cancer. Nonetheless, the utility of assessing intentions and acceptability regarding new methods of early cancer detection and prevention prior to their availability has been demonstrated in other cancers (e.g., spiral CT for early detection of lung cancer [32] and HPV vaccination for the prevention of cervical cancer [47]); such research is critical for the successful development and uptake of new strategies to detect and prevent cancer. Finally, as one of the first studies to provide data about receptivity to screening options for PC, it is limited in scope and not comprehensive. The assessments of perceived risk and acceptability of false-negatives/false-positives in this study avoided numeracy concerns but were compromised by imprecision. Future studies should explore concerns related to sensitivity and specificity of potential screening tests in greater detail as well as other barriers to early detection such as cost and availability; whether screening confers actual improvement in survival for PC remains to be determined. Addressing each of these issues in future studies of individuals and families at significant risk of pancreatic cancer will facilitate collective efforts toward the development and implementation of appropriate and acceptable screening methods targeting high-risk individuals.
References
American Cancer Society (ACS): Cancer Facts & Figures 2012. http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-031941.pdf
Hruban RH, Canto M, Goggins M, Schulick R, Klein AP: Update on Familial Pancreatic Cancer. Adv Surg 2010, 44: 293–311. PMCID: PMC2966038
Petersen GM, de Andrade M, Goggins M, Hruban RH, Bondy M, Korczak JF, Gallnger S, Lynch HT, Syngal S, Rabe KG, Seminara D, Klein AP: Pancreatic cancer genetic epidemiology consortium. Cancer Epidemiol Biomarkers Prev 2006, 15: 704–710. 15/4/70410.1158/1055-9965.EPI-05-0734
U.S. Preventive Services Task Force (USPSTF): Screening for Pancreatic Cancer: Recommendation Statement. 2004. http://www.uspreventiveservicestaskforce.org/3rduspstf/pancreatic/pancrers.htm
Verna EC, Hwang C, Stevens PD, Rotterdam H, Stavropoulos SN, Sy CD, Prince MA, Chung WK, Fine RL, Chabot JA, Frucht H: Pancreatic cancer screening in a prospective cohort of high-risk patients: A comprehensive strategy of imaging and genetics. Clin Cancer Res 2010, 16: 5028–5037. 10.1158/1078-0432.CCR-09-3209
Al-Sukhni W, Borgida A, Rothenmund H, Holter S, Semotiuk K, Grant R, Wilson S, Moore M, Narod S, Jhaveri K, Haider MA, Gallinger S: Screening for pancreatic cancer in a high-risk cohort: An eight-year experience. J Gastrointest Surg 2012, 16: 771–783. 10.1007/s11605-011-1781-6
Goggins M, Canto M, Hruban R: Can we screen high-risk individuals to detect early pancreatic carcinoma? J Surg Oncol 2000, 74: 243–248. 10.1002/1096-9098(200008)74:4<243::AID-JSO1>3.0.CO;2-C
Canto MI, Hruban RH, Fishman EK, Kamel IR, Schulick R, Zhang Z, Topazian M, Takahashi N, Fletcher J, Petersen G, Klein AP, Axilbund J, Griffin C, Syngal S, Saltzman JR, Mortele KJ, Lee J, Tamm E, Vikram R, Bhosale P, Margolis D, Farrell J, Goggins M, American Cancer of the Pancras Screening (CAPS) Consortium, American Cancer of the Pancras Screening (CAPS) Consortium: Frequent detection of pancreatic lesions in asymptomatic high-risk individuals. Gastroenterol 2012, 142: 796–804. 10.1053/j.gastro.2012.01.005
Brand RE, Lerch MM, Rubinstein WS, Neoptolemos JP, Whitcomb DC, Hruban RH, Brentnall TA, Lynch HT, Canto MI, Participants of the Fourth International Symposium of Inherited Diseases of the Pancreas, Participants of the Fourth International Symposium of Inherited Diseases of the Pancreas: Advances in counselling and surveillance of patients at risk for pancreatic cancer. Gut 2007, 56: 1460–1469. 10.1136/gut.2006.108456
Canto MI, Goggins M, Hruban RH, Petersen GM, Giardiello FM, Teo C, Fishman EK, Brune K, Axibund J, Griffin C, Ali S, Richman J, Jagannath S, Kantsevoy SV, Kalloo AN: Screening for early pancreatic neoplasia in high-risk individuals: a prosective controlled study. Clin Gastroenterol Hepatol 2006, 4: 766–781. 10.1016/j.cgh.2006.02.005
Gold DV, Goggins M, Modrak DE, Newsome G, Liu M, Shi C, Hruban RH, Goldenberg DM: Detection of early-stage pancreatic adenocarcinoma. Cancer Epidemiol Biomarkers Prev 2010, 19: 2786–2794. PMCID: PMC2976815 10.1158/1055-9965.EPI-10-0667
Li C, Zolotarevsky E, Thompson I, Anderson MN, Simeone DM, Casper JM, Mullenix MC, Lubman DM: A multiplexed bead assay for profiling glycosylation patterns on serum protein biomarkers of pancreatic cancer. Electrophoresis 2011, 32: 2028–2035. 10.1002/elps.201000693
Pan S, Chen R, Crispin DA, May D, Stevens T, McIntosh MW, Bronner MP, Ziogas A, Anton-Culver H, Brentnall TA: Protein alterations associated with pancreatic cancer and chronic pancreatitis found in human plasma using global quantitative proteomics profiling. J Proteome Res 2011, 10: 2359–2376. PMCID: PMC3090497 10.1021/pr101148r
Kisiel JB, Yab TC, Taylor WR, Chari ST, Petersen GM, Mahoney DW, Ahlquist DA: Stool DNA testing for the detection of pancreatic cancer: Identification and assessment of methylation marker candidates. Cancer 2012, 118: 2623–2631. 10.1002/cncr.26558
Wiersema MJ: Accuracy of endoscopic ultrasound in diagnosing and staging pancreatic carcinoma. Pancreatology 2001, 1: 625–632. 10.1159/000055872
Canto MI, Goggins M, Yeo CJ, Griffin C, Axilbund JE, Brune K, Ali SZ, Jaqannath S, Petersen GM, Fishman EK, Piantadosi S, Giardiello FM, Hruban RH: Screening for pancreatic neoplasia in high-risk individuals: an EUS-based approach. Clin Gastroenterol Hepatol 2004, 2: 606–621. 10.1016/S1542-3565(04)00244-7
Jhala NC, Jhala D, Eltoum I, Vickers SM, Wilcox CM, Chhieng DC, Eloubeidi MA: Endoscopic ultrasound-guided fine-needle aspiration biopsy: a powerful tool to obtain samples from small lesions. Cancer 2004, 102: 239–246. 10.1002/cncr.20451
Legmann P, Vignaux O, Dousset B, Baraza AJ, Palazzo L, Dumontier I, Coste J, Louvel A, Roseau G, Couturier D, Bonnin A: Pancreatic tumors: comparison of dual-phase helical CT and endoscopic sonography. AJR Am J Roentgenol 1998, 170: 1315–1322.
Yasuda I, Iwashita T, Doi S, Nakashima M, Moriwaki H: Role of EUS in the early detection of small pancreatic cancer. Dig Endosc 2011,23(Suppl 1):22–25. 10.1111/j.1443-1661.2011.01113.x
Klein AP, Brune KA, Petersen GM, Goggins M, Tersmette AC, Offerhaus GJ, Griffin C, Cameron JL, Yeo CJ, Kern S, Hruban RH: Prospective risk of pancreatic cancer in familial pancreatic cancer kindreds. Cancer Res 2004, 64: 2634–2638. 10.1158/0008-5472.CAN-03-3823
Ries LAG, Melbert D, Krapcho M, Stinchcomb DG, Howlader N, Horner MJ Mariotto A, Miller BA, Feuer EJ, Altekruse SF, Lewis DR, Clegg L, Eisner MP, Reichman M, Edwards B: SEER Cancer Statistics Review, 1975–2005. National Cancer Institute, Bethesda, MD; 2008. http://seer.cancer.gov/csr/1975_2005/,basedonNovember2007SEERdatasubmission,postedtotheSEERwebsite
Harinck F, Nagtegaal T, Kluijt I, Aalfs C, Smets E, Poley JW, Wagner A, van Hooft J, Fockens P, Bruno M, Bleiker EM: Feasibility of a pancreatic cancer surveillance program from a psychological point of view. Genet Med 2011, 13: 1015–1024. 10.1097/GIM.0b013e31822934f5
Lampic C, Thurfjell E, Bergh J, Sjödén PO: Short- and long-term anxiety and depression in women recalled after breast cancer screening. Eur J Cancer 2001, 37: 463–469. 10.1016/S0959-8049(00)00426-3
McCaul KD, Goetz PW: Worry: Health Behavior Constructs: Theory, Measurement, and Research. Accessed from: . Accessed on June 28, 2012 http://dccps.cancer.gov/brp/constructs.worry/index.html
Michielutte R, Dignan MB, Smith BL: Psychosocial Factors Associated with the Use of Breast Cancer Screening by Women Age 60 Years or Over. Health Educ Behav 1999, 26: 625–647. 10.1177/109019819902600505
Petersen GM, Larkin E, Codori AM, Wang CY, Booker SV, Bacon J, Giardiello FM, Boyd PA: Attitudes toward colon cancer gene testing: survey of relatives of colon cancer patients. Cancer Epidemiol Biomarkers Prev 1999, 8: 337–344.
Stefanek ME: Psychosocial aspects of breast cancer. Curr Opin Oncol 1992, 4: 1055–1060. 10.1097/00001622-199212000-00009
Vernon SW: Participation in colorectal cancer screening: a review. J Natl Cancer Inst 1997, 89: 1406–1422. 10.1093/jnci/89.19.1406
Wang L, Bamlet WR, de Andrade M, Boardman LA, Cunningham JM, Thibodeau SN, Petersen GM: Mitochondrial genetic polymorphisms and pancreatic cancer risk. Cancer Epidemiol Biomarkers Prev 2007, 16: 1455–1459. 16/7/145510.1158/1055-9965.EPI-07-0119
Lerman C, Rimer BK: Psychosocial impact of cancer screening. In Psychosocial Effects of Screening for Disease Prevention and Detection. Edited by: Croyle RT. Oxford University Press, New York; 1995:65–81.
Lerman C, Schwartz M: Adherence and psychological adjustment among women at high risk for breast cancer. Breast Cancer Res Treat 1993, 28: 145–155. 10.1007/BF00666427
Sinicrope PS, Rabe KG, Brockman TA, Patten CA, Petersen WO, Slusser J, Yang P, Swensen SJ, Edell ES, de Andrade M, Petersen GM: Perceptions of lung cancer risk and beliefs in screening accuracy of spiral computed tomography among high-risk lung cancer family members. Acad Radiol 2010, 17: 1012–1025. 10.1016/j.acra.2010.04.003
Vincent A, Herman J, Schulick R, Hruban RH, Goggins M: Pancreatic cancer. Lancet 2011, 378: 607–620. 10.1007/s10897-008-9205-9
Lewis ZK, Frost CJ, Venne VL: Pancreatic cancer surveillance among high-risk populations: Knowledge and intent. J Genet Counsel 2009, 18: 229–238. 10.1007/s10897-008-9205-9
Rogers RW: A protection motivation theory of fear appeals and attitude change. J Psychol 1975, 91: 93–114. 10.1080/00223980.1975.9915803
Becker MH: The health belief model and personal health behavior. Health Educ Monogr 1974, 2: 324–508.
Rosenstock IM, Strecher VJ, Becker MH: Social learning theory and the health belief model. Health Educ Q 1988, 15: 175–183. 10.1177/109019818801500203
Hay JL, Primavera LH, Levy A, Shuk E, Ostroff JS: Development and validation of a scale assessing novel cancer-related risk perceptions. Ann Behav Med 2006, 31: S190.
Hay JL, Shuk E, Cruz G, Ostroff J: Thinking Through Cancer Risk: Characerizing Smokers’ Process of Risk Determination. Qualitative Health Res 2005, 15: 1074–1085. 10.1177/1049732305276682
Jones SC, Magee CA, Barrie LR, Iverson DC, Gregory P, Hanks EL, Nelson AE, Nehill CL, Zorbas HM: Australian Women’s Perceptions of Breast Cancer Risk Factors and the Risk of Developing Breast Cancer. Womens Health Issues 2011, 21: 353–360. 10.1016/j.whi.2011.02.004
Mellon S, Berry-Bobovski L, Gold R, Levin N, Tainsky MA: Communication and decision-making about seeking inherited cancer risk information: Findings from female survivor-related focus groups. Psycho-Oncol 2006, 15: 193–208. 10.1002/pon.935
Tilburt JC, James KM, Sinicrope PS, Eton DT, Costello BA, Carey J, Lane MA, Ehlers SL, Erwin PJ, Nowakowski KE, Murad MH: Factors Influencing Cancer Risk Perception in High Risk Populations: A Systematic Review. Hereditary Cancer Clin Pract 2011, 9: 2. PMCID: PMC3118965 10.1186/1897-4287-9-2
Michaud DS, Giovannucci E, Willett WC, Colditz GA, Stampfer MJ, Fuchs CS: Physical activity, obesity, height, and the risk of pancreatic cancer. JAMA 2001, 286: 921–929. 10.1001/jama.286.8.921
Boyle P, Maisonneuve P, Bueno de Mesquita B, Ghadirian P, Howe GR, Zatonski W, Baqhurst P, Moerman CJ, Simard A, Miller AB, Przewoniak K, McMichael AJ, Hsieh CC, Walker AM: Cigarette smoking and pancreas cancer: a case control study of the search programme of the IARC. Int J Cancer 1996, 67: 63–71. 10.1002/(SICI)1097-0215(19960703)67:1<63::AID-IJC12>3.0.CO;2-D
Perloff LS: Social comparison and illusions of invulnerability to negative life events. In Coping with negative life events: Clinical and social psychological perspectives. Edited by: Snyder CR, Ford CE. Plenum Press, New York, NY; 1987:217–242.
Perloff LS, Fetzer BK: Self-other judgments and perceived vulnerability to victimization. J Personality Social Psychol 1986, 50: 502–510.
Allen JD, Coronado GD, Williams RS, Glenn B, Escoffery C, Fernandez M, Tuff RA, Wilson KM, Mullen PD: A systematic review of measures used in studies of human papillomavirus (HPV) vaccine acceptability. Vaccine 2010, 28: 4027–4037. 10.1016/j.vaccine.2010.03.063
Acknowledgments
Sources of funding
This research was supported by the National Cancer Institute grants R01CA97075 and P50 CA102701 (Mayo Clinic Specialized Programs of Research Excellence in Pancreatic Cancer) as well as the Mayo Foundation (Cancer Experience Interest Group).
We would like to acknowledge the study participants as well as the individuals who were involved in their recruitment, including Diane Batzel, Susan Bisping, Jodie Cogswell, Traci Hammer, Margaret Landhuis, Karen Olson, Amy Reynolds, Hiedi Treitline, and Cindy Wong. We also thank Jeff Leirness, Que Luu, Martha Matsumoto, and Dennis Robinson for their contributions to the data management.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors’ contributions
CRB and PSS drafted the manuscript. GMP and CRB made substantial contributions to the analysis and interpretation of the data. KGR performed the statistical analysis. PSS, CAP, RRM, SE, and GMP conceived of the study, participated in its design, and constructed the survey. TAB coordinated the research effort and helped to revise the manuscript. GMP provided critical intellectual content and expertise from the conception to the conclusion of this research. All authors read and approved the final manuscript.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Breitkopf, C.R., Sinicrope, P.S., Rabe, K.G. et al. Factors influencing receptivity to future screening options for pancreatic cancer in those with and without pancreatic cancer family history. Hered Cancer Clin Pract 10, 8 (2012). https://doi.org/10.1186/1897-4287-10-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1897-4287-10-8