Abstract
Background
Ixodes scapularis saliva enables the transmission of infectious agents to the mammalian host due to its immunomodulatory, anesthetic and anti-coagulant properties. However, how I. scapularis saliva influences host cytokine secretion in the presence of the obligate intracellular rickettsial pathogen Anaplasma phagocytophilum remains elusive.
Methods
Bone marrow derived macrophages (BMDMs) were stimulated with pathogen associated molecular patterns (PAMPs) and A. phagocytophilum. Cytokine secretion was measured in the presence and absence of I. scapularis saliva. Human peripheral blood mononuclear cells (PBMCs) were also stimulated with Tumor Necrosis Factor (TNF)-α in the presence and absence of I. scapularis saliva and interleukin (IL)-8 was measured.
Results
I. scapularis saliva inhibits inflammatory cytokine secretion by macrophages during stimulation of Toll-like (TLR) and Nod-like receptor (NLR) signaling pathways. The effect of I. scapularis saliva on immune cells is not restricted to murine macrophages because decreasing levels of interleukin (IL)-8 were observed after TNF-α stimulation of human peripheral blood mononuclear cells. I. scapularis saliva also mitigates pro-inflammatory cytokine response by murine macrophages during challenge with A. phagocytophilum.
Conclusions
These findings suggest that I. scapularis may inhibit inflammatory cytokine secretion during rickettsial transmission at the vector-host interface.
Similar content being viewed by others
Background
Hematophagy occurred independently in more than 14,000 arthropod species and this adaptation required physiological, morphological, behavioral and biochemical changes [1, 2]. Salivary gland secretion is among the most common physiological and biochemical adaptation in hematophagous arthropods and salivary proteins from ticks, mosquitoes, biting flies, fleas and other blood-feeding arthropods ensue defense against host homeostasis and inflammation [1–8]. Combating inflammation is particularly problematic for ixodid ticks because these arthropods have to feed for a prolonged period of time and are exposed to a wide range of immune cells [9, 10]. Pioneering studies have characterized the physiology of tick salivary glands [11] and raised the importance of saliva as an instrumental force for immune evasion [12–15]. Several groups have demonstrated that both proteinaceous and non-proteinaceous components of tick saliva impair the complement system and the function of macrophages, dendritic, T and B cells [8, 16–25]. From these studies it also became apparent that pathogens take advantage of the immunomodulatory properties of vector saliva to colonize the host.
Titus and Ribeiro were the first researchers to describe the role of arthropod salivary glands facilitating parasite transmission. In this seminal work, the authors showed that sandfly salivary glands facilitate Leishmania spp. transmission to the mammalian host [26]. Subsequent studies by many other groups demonstrated that the saliva of arthropod vectors potentiates the transmission of a wide-range of arthropod-borne pathogens, including bacteria, viruses and protozoal organisms. For example, in Ixodes spp., Borrelia burgdorferi outer surface protein C (OspC) binds to salivary protein 15 (Salp15), which then acts as a barrier to protect this spirochete against the host immune response [27]. Sialostatin L2, an I. scapularis cystatin protein also facilitates the growth of the Lyme disease agent B. burgdorferi[28]. In addition, I. ricinus saliva inhibits interferon and Toll-like receptor (TLR) signaling during cell stimulation with B. afzelli[29, 30]. Finally, infection by the tick-borne encephalitis virus can be prevented by immunizing animals against a truncated recombinant form of a tick salivary protein named 64P [31].
Anaplasma phagocytophilum is a pathogen transmitted by ixodid ticks and causes human granulocytic anaplasmosis, an emerging infectious disease in the United States, Europe and Asia [32]. However, it remains mostly unknown whether tick saliva inhibits cytokine secretion by macrophages during stimulation with A. phagocytophilum. Macrophages were recently shown to be important for defense against A. phagocytophilum colonization [33]. In this study, we show that I. scapularis saliva inhibits extracellular and intracellular receptor signaling in both murine and human immune cells. We also demonstrate that tick saliva mitigates A. phagocytophilum-induced cytokine secretion by murine macrophages. This report expands previous scientific knowledge on the immunomodulatory properties of tick saliva and suggests that rickettsial agents may use I. scapularis saliva to inhibit inflammation at the vector-host interface.
Methods
Ethical statements
Blood samples were obtained from healthy, non-pregnant adults. This procedure was approved by the Human Research Review Board (HRRB number: HS-08-135) at the University of California-Riverside. All animal experiments were approved by the Institutional Animal Care and Use Committee (IACUC number: A-20110030BE) at the University of California-Riverside. We used C57BL/6 mice at 6–10 weeks of age purchased from Jackson Laboratories. Experimentation with A. phagocytophilum (HZ strain) was approved by the Biological Use Authorization Committee (BUA number: 20120020) at the University of California-Riverside. A. phagocytophilum was grown in HL-60 cells (ATCC CCL-240). HL-60 cells were maintained in Iscove’s Modified Dulbecco’s Media (IMDM) with L-glutamine and hydroxyethyl piperazineethanesulfonic acid (HEPES) (Thermo Scientific), 20% heat-inactivated fetal bovine serum (FBS) (Sigma) in 5% CO2 and humidified air at 37°C, as previously described [33].
Reagents
Lipopolysaccharide (LPS), Pam3CSK4, Zymosan, Porphyromonas gingivalis (PG)-LPS and muramyl dipeptide (MDP) were obtained from Invivogen. DOTAP was obtained from Roche. Human recombinant TNF-α was purchased from R&D Systems.
Cell isolation and tick saliva collection
The generation of bone marrow-derived macrophages (BMDMs) and tick saliva has been previously described [33–35]. Briefly, mouse femurs were flushed and bone marrow cells were differentiated in complete Dulbecco’s Modified Eagle Medium (DMEM) (Fisher) supplemented with 30% L929 cell-conditioned media, 10% FBS and 1% PSA (100 U/mL penicillin, 100 mg/ml streptomycin, and 0.25μg/ml amphotericin) (Fisher). Cells were cultured at 37°C in a 5% CO2 tissue culture incubator for 5–6 days, with media changed on day 3. Human peripheral blood mononuclear cells (PBMCs) were isolated by using the Polymorphprep protocol (Axis Shield).
We collected I. scapularis saliva 4–5 days after feeding because studies suggest that transmission of A. phagocytophilum initiates slowly between 24 and 48 hours and is enhanced during rapid feeding to repletion around 72 h–96 h post tick attachment [36–38]. Therefore, saliva from I. scapularis would reflect actual conditions during A. phagocytophilum transmission at the vector-host interface. In addition, I. scapularis saliva collection at 24–48 hours is technically very challenging. The alternative would be using salivary glands. However, salivary glands bring a technical artifact to the system because this organ in ticks is rich in intracellular proteins and other immune effectors such as nucleotides, which may skew cytokine response in immune cells. To isolate vector saliva, I. scapularis ticks were allowed to feed on New Zealand white rabbits. A restraining collar was placed around the neck of each rabbit, and their ears were covered prior to tick exposure. Ticks were permitted to engorge for 4–5 days on the ear of a rabbit. Upon harvesting, ticks were rinsed in distilled water and were immediately fixed to glass slides with double-sided tape. A sterile glass micropipette was placed around the hypostome to collect saliva. Salivation was induced by the application of pilocarpine to the scutum of the tick. Saliva was pooled and stored at −80°C for use.
Immune cell stimulation
BMDMs from C57BL/6 mice were stimulated with the TLR agonists LPS (500 ng/ml), Pam3CSK4 (1 μg/ml), Zymosan (10 μg/ml) and PG- LPS (500 ng/ml), the Nod2 stimulant MDP (10 μg/ml) or A. phagocytophilum (multiplicity of infection (MOI) 10 and 50) at indicated dilutions of tick saliva. Human PBMCs were purified by using the Polymorphprep protocol (Axis Shield), plated for 2 hours and incubated with tick saliva for 30 minutes followed by 4 hours of stimulation with 100 ng/ml of Tumor Necrosis Factor (TNF)-α. Pro-inflammatory cytokines such as TNF-α, interleukin (IL)-12p40, IL-6 and IL-1β or the chemokine IL-8 (CXCL8) were measured by ELISA.
ELISA
Mouse TNF-α, IL-1β, IL-6 and human IL-8 were measured with the BD OptEIA Set from BD Biosciences. Mouse IL-12p40 was measured with capture and detection antibodies from eBiosciences. For the ELISA assays, wells were coated with recommended capture antibody dilutions in freshly prepared coating buffer (0.1 M sodium carbonate, pH 9.5). Plates were sealed and incubated overnight at 4°C followed by aspiration. Wells were then washed 3 times with ≥ 300 μL/well of freshly prepared wash buffer (phosphate buffered saline (PBS) with 0.05% Tween-20). After the last wash, plates were inverted and blotted on absorbent paper to remove any residual buffer. Wells were then blocked with ≥ 200 μL/well of assay diluent (PBS with 10% FBS, pH 7.0) and incubated at room temperature for 1 hour. Plates were washed 3 times with wash buffer. Then, standards and sample dilutions were prepared in assay diluent, as recommended (BD Biosciences). 100 μL of samples and standards were pipetted into the wells, incubated for 2 hours at room temperature followed by 5 washes. 100 μL of detection antibodies were diluted in assay diluent and added to each well. Plates were sealed and incubated for 1 hour at room temperature. Plates were washed 5 times. Then, 100 μL of enzyme reagent (BD OptEIA Set from BD Biosciences) were diluted in assay diluent, pipetted into each well and incubated for 30 minutes at room temperature. Wells were aspirated and washed 7 times with wash buffer. 100 μL of substrate solution (BD OptEIA Set from BD Biosciences) were added to each well and incubated for 30 minutes (without plate sealer) at room temperature in the dark. 50 μL of 2 N H2SO4 was added to each well. Absorbance was read in the ELISA plate reader (Bio-Rad) at 450 nm within 30 minutes. Background was corrected by reading the subtract absorbance at 570 nm.
Cell death assay
Cell death was assayed by measuring lactate dehydrogenase (LDH), as recommended by the manufacturer (Takara). Briefly, 100 μL of each sample was placed into a well. Then, a catalyst solution (Takara) was added to the samples and controls. Samples were incubated for 10–30 minutes, at room temperature, protected from light. Reactions were stopped at the end of the incubation period by adding 50 μL of 1 N HCl. Absorbance was measured at 490 nm. The iMark microplate absorbance reader (Bio-Rad) was used according to the manufacturer’s instruction.
Statistical analysis
Data were expressed as means ± standard errors of the means (SEM). The following parametric analyses were used: unpaired Student’s t test (two-group comparisons); one-way analysis of variance (ANOVA) (comparisons of three or more groups); Bonferroni post hoc multiple-comparison tests were used following ANOVA. All statistical calculations were performed using GraphPad Prism version 5.04. Graphs were made using GraphPad Prism version 5.04. P < 0.05 was considered statistically significant.
Results
I. scapularis saliva diminishes inflammatory cytokine secretion by murine macrophages
Tick saliva has immunomodulatory properties [1, 2]. To determine whether tick saliva inhibits macrophage function, we first stimulated mouse BMDMs with LPS in the presence or absence of different dilutions of I. scapularis saliva. Cytokine levels were not altered during BMDM stimulation with tick saliva alone, suggesting that the saliva does not carry any contaminants, pathogen-associated molecular (PAMPs) or danger-associated molecular (DAMPs) patterns. As expected, LPS induced high levels of cytokine secretion in murine BMDMs (Figures 1 and 2). However, I. scapularis saliva inhibited secretion of both TNF-α and IL-12p40 by BMDMs after stimulation with LPS (Figure 1). This effect was more pronounced for TNF-α, as a tick saliva dilution of 1:10000 (v/v) still affected cytokine secretion by BMDMs during LPS stimulation (Figure 1A). A reduction in IL-12p40 secretion by macrophages after LPS stimulation was only observed for a tick saliva dilution of 1:1000 (v/v) and below (Figure 1B).
I. scapularis saliva mitigates LPS-mediated cytokine secretion by murine macrophages. BMDMs (8×105) from C57BL/6 mice were stimulated with LPS (500 ng/ml) for 18 hours, in the presence or absence of indicated dilutions of tick saliva. (A) TNF-α and (B) IL-12p40 were measured by ELISA. Tick saliva was added 2 hours before stimulation. Responses were measured in triplicate and presented as mean ± SEM within the representative experiment. Experiments were repeated three times. *P < .05, One-way ANOVA, post-hoc Bonferroni; (−) non-stimulated cells. NS – not significant.
I. scapularis saliva inhibits TLR-mediated cytokine secretion by macrophages. BMDMs (8×105) from C57BL/6 mice were stimulated with LPS (500 ng/ml), Pam3CSK4 (1 μg/ml), Zymosan (10 μg/ml) and PG- LPS (500 ng/ml) for 18 hours in the presence or absence of tick saliva (1:500 dilution). Tick saliva was added 2 hours before stimulation. (A) IL-6 and (B) IL-12p40 were measured by ELISA. Responses were measured in triplicate and presented as mean ± SEM within the representative experiment. Experiments were repeated three times. *P < .05, Student’s t test. (−) non-stimulated cells. NS – not significant.
We then stimulated mouse BMDMs with a wide range of TLR ligands and measured IL-6 and IL-12p40 secretion in the presence of I. scapularis saliva. Tick saliva 1:500 (v/v) inhibited IL-6 and IL-12p40 secretion by BMDMs when stimulated with TLR agonists, such as LPS, Pam3CSK4, Zymosan and PG-LPS (Figure 2). Next, we stimulated BMDMs with Nod1 and Nod2 agonists to determine whether the effect of I. scapularis saliva on cytokine secretion was restricted to TLRs. Nod1 and Nod2 are considered cytosolic receptors and are part of the Nod-like receptor (NLR) protein family [39]. The Nod1 and Nod2 agonists iE-DAP and MDP did not induce cytokine production in BMDMs during extracellular stimulation (Figure 3; data not shown). However, transfection of MDP to the cytosol using the cationic lipid DOTAP led to secretion of both IL-6 and IL-12p40 by BMDMs (Figure 3). Further, I. scapularis saliva inhibited IL-6 and IL-12p40 secretion mediated by the transfected Nod2 agonist MDP at the saliva dilution of 1:500 (v/v). Taken together, we report that I. scapularis saliva mitigates cytokine secretion by BMDMs during extracellular and cytosolic stimulation of TLR and NLR pathways.
I. scapularis saliva impairs Nod2-mediated cytokine secretion by murine macrophages. BMDMs (1×106) from C57BL/6 mice were stimulated with MDP (10 μg/ml) or DOTAP (10 μg/ml) + MDP (10 μg/ml) for 20 hours, in the presence or absence of tick saliva (1:500). The secretion of (A) IL-6 and (B) IL-12p40 were measured by ELISA. Responses were measured in triplicate and presented as mean ± SEM within the representative experiment. Experiments were repeated three times. *P < .05, Student’s t test. (−) non-stimulated cells. NS – not significant.
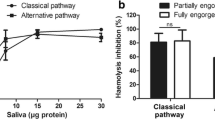
I. scapularis saliva inhibits chemokine secretion by human peripheral blood mononuclear cells
We then tested whether the effect observed for I. scapularis during cytokine secretion was restricted to murine BMDMs. We isolated human PBMCs from the blood of healthy and immunocompetent adults and stimulated these immune cells with the pro-inflammatory cytokine TNF-α. TNF-α has been extensively used to stimulate cytokine secretion in immune cells [40]. We included human PBMCs in our studies for two reasons. First, we would like to show that the inhibitory aspect of tick saliva is not only restricted to murine immune cells. To the contrary, it can also occur during stimulation of human immune cells. Second, PBMCs are a heterogenous group of immune cells. Therefore, we reasoned that PBMCs would be ideal to demonstrate the inhibitory cytokine capacity of tick saliva in a mixed group of immune cells. The chemokine IL-8 (CXCL-8) was used as a read-out in our analysis. PBMCs produced large amounts of IL-8 when stimulated with TNF-α (Figure 4). Similar to our findings observed in murine BMDMs, IL-8 (CXCL8) secretion by PBMCs stimulated with recombinant human TNF-α was diminished in the presence of tick saliva (Figure 4). Overall, our results show that I. scapularis saliva is able to mitigate cytokine and chemokine secretion by both murine and human immune cells.
I. scapularis saliva decreases IL-8 secretion by human peripheral blood mononuclear cells. PBMCs (9×105) were purified and plated for 2 hours. Cells were incubated with tick saliva for 30 minutes followed by 4 hours of stimulation with 100 ng/ml TNF-α. The secretion of IL-8 (CXCL8) was measured by ELISA. Responses were measured in triplicate and presented as mean ± SEM within the representative experiment. *P < .05, Student’s t test. (−) non-stimulated cells. NS – not significant.
I. scapularis saliva lessens inflammatory cytokine secretion by murine macrophages during A. phagocytophilum stimulation
To determine whether the effect of tick saliva was restricted to TLR and NLR ligands, we stimulated BMDMs with the I. scapularis rickettsial pathogen A. phagocytophilum. A. phagocytophilum induced the secretion of large amounts of cytokines by murine macrophages (Figures 5 and 6A-B). Nonetheless, tick saliva was also efficient in reducing cytokines by BMDMs, such as IL-6, IL-12p40 and TNF-α during A. phagocytophilum stimulation (Figure 5). Similar to BMDM stimulation with LPS, the effect of tick saliva was more pronounced on TNF-α secretion by BMDMs during pathogen stimulation. TNF-α secretion was completely abolished when BMDMs were stimulated with A. phagocytophilum in the presence of tick saliva (Figure 5C).
I. scapularis saliva mitigates cytokine secretion by macrophages during A. phagocytophilum stimulation in a dose-dependent manner. BMDMs (1×106) from C57BL/6 mice were stimulated with the wild-type A. phagocytophilum HZ strain (MOI 50) for 18 hours in the presence or absence of tick saliva (1:150 and 1:300 dilution). (A) IL-6, (B) IL-12p40 and (C) TNF-α were measured by ELISA. Responses were measured in triplicate and presented as mean ± SEM within the representative experiment. *P < .05, One-way ANOVA, post-hoc Bonferroni; (-) non-stimulated cells. NS – not significant.
I. scapularis saliva decreases IL-1β secretion by macrophages during A. phagocytophilum stimulation. (A) BMDMs (1×106) from C57BL/6 mice were primed with LPS (500 ng/nl) for 24 hours, washed and then stimulated with the A. phagocytophilum HZ strain (MOIs 10 and 50) for another 24 hours. IL-1β was measured by ELISA. (B) BMDMs (1×106) from C57BL/6 mice were stimulated with the wild-type A. phagocytophilum HZ strain (MOI 50) for 18 hours in the presence or absence of tick saliva (1:150 dilution). IL-1β was measured by ELISA. (C) Cell death was measured using the LDH assay. Responses were measured in triplicate and presented as mean ± SEM within the representative experiment. *P < .05, Student’s t test. (−) non-stimulated cells. NS – not significant.
Overall, the inhibitory effect of tick saliva on cytokine secretion by BMDMs during A. phagocytophilum stimulation was best observed at a 1:150 dilution (v/v). Experiments performed with tick saliva at a 1:300 dilution (v/v) also showed reduction of cytokine secretion by BMDMs during A. phagocytophilum stimulation (Figure 5). However, the effect was milder (although statistically significant) for IL-6 and IL-12p40 (Figure 5A and B). We did not detect a dilution effect on TNF-α secretion by BMDMs at a 1:300 dilution (v/v) (Figure 5C). These results suggest that the inhibition threshold for tick saliva on TNF-α secretion by BMDMs during A. phagocytophilum stimulation is greater than 1:300 (v/v) compared to 1:150 dilution (v/v). It is unclear why more concentrated tick saliva is required to inhibit cytokine secretion during A. phagocytophilum stimulation when compared to individual TLR or NLR agonists. We reasoned that the presence of multiple PAMPs in a pathogen, such as A. phagocytophilum, may require a stronger dose of tick saliva to mitigate cytokine secretion by BMDMs.
I. scapularis saliva inhibits IL-1β secretion by murine macrophages during A. phagocytophilum stimulation
A dogma has emerged in the last few years in which the production and release of IL-1β are the result of a two-tier system: one signal is induced by pattern recognition receptors or pro-inflammatory cytokines, which activates the transcription and translation of IL-1β via the transcription factor nuclear factor (NF)-κB. This signal is also referred to as priming and it is typically done by LPS stimulation of immune cells. The second signal is mediated by the inflammasome, a protein scaffold that cleaves IL-1β into its mature form through caspase-1 activation [41–43]. Our studies show that IL-1β secretion triggered by A. phagocytophilum during BMDM stimulation does not require LPS priming. To the contrary, LPS priming in BMDMs before A. phagocytophilum stimulation inhibited IL-1β secretion in a dose-dependent manner (Figure 6A). These results are consistent with the lack of genes for LPS and peptidoglycan synthesis in the A. phagocytophilum genome [44] and suggest that molecules other than LPS may prime BMDMs for the production of pro-IL-1β. Further, tick saliva inhibited A. phagocytophilum-induced IL-1β secretion by BMDMs (Figure 6B). IL-1β secretion may be coupled to a cell death phenomenon named pyroptosis [45]. We did not detect high levels of cell death during A. phagocytophilum stimulation of BMDMs in the absence of tick saliva (~10-15%) (Figure 6C). However, this is not entirely surprising, as A. phagocytophilum does not cause much cell death during infection [32, 46]. Based on these findings, we conclude that in the A. phagocytophilum model, cytokine secretion is a better indicator of the anti-inflammatory features of tick saliva when compared to cell death.
Discussion
Inflammation is characterized by complex interactions between innate and adaptive immunity [47]. Pro-inflammatory cytokines and chemokines recruit immune cells to the site of tick feeding. Tick salivary proteins then mitigate the secretion of cytokines by immune cells, thereby, diminishing inflammation [1, 2, 4]. Despite significant progress in the past decades, how ectoparasites, such as ticks, regulate host innate immune signaling during transmission of the rickettsial agent A. phagocytophilum to the mammalian host remains mostly elusive. In this study, we demonstrate that I. scapularis saliva has the ability to inhibit cytokine secretion by murine and human immune cells. These findings are supported by our results showing that extracellular and cytosolic stimulation of macrophages with PAMPs can be inhibited by I. scapularis saliva. We also performed experiments with A. phagocytophilum and demonstrated that similar mitigation effects occur in macrophages. The implications for these findings are wide in scope as ticks, mosquitoes, biting flies, fleas and blood-feeding bugs have also evolved similar strategies for modulating host defenses [2].
We reported an effect of tick saliva on TLR and NLR signaling in macrophages. Although the effect of tick saliva was previously demonstrated during TLR stimulation of dendritic cells [29, 30, 48–50], whether I. scapularis saliva affects the response to stimulation of murine macrophages and human peripheral blood mononuclear cells had not been determined. Macrophages and peripheral blood mononuclear cells are important because these immune cells respond to A. phagocytophilum infection [33, 51]. To our knowledge, we describe for the first time that secretion of IL-6 and IL-12p40 after stimulation with the Nod2 ligand MDP was diminished in macrophages during treatment with tick saliva. Nod2 has emerged as a critical regulator for immunity and inflammation since it activates canonical and non-canonical NF-κB signaling, mitogen-activated protein kinases, cytokines, chemokines and antimicrobial reactive oxygen species [39].
Previously, we showed that A. phagocytophilum is partially recognized by the NLRC4 inflammasome [52], a protein scaffold that regulates the secretion of IL-1β and IL-18 [45]. We also demonstrated that mice deficient in caspase-1 and asc, essential components of the inflammasome, were more susceptible than wild-type animals to A. phagocytophilum infection. These findings were due to the absence of IL-18 secretion and reduced interferon (IFN)-γ levels in the peripheral blood. It is unclear how I. scapularis saliva regulates IL-1β secretion by macrophages during A. phagocytophilum stimulation. However, it is possible that multiple salivary proteins regulate IL-1β secretion during hematophagy. Ticks have large genomes and carry many gene paralogs [53]. These gene paralogs may act redundantly to provide inhibition of immune protein scaffolds in the mammalian host. Two earlier articles provided experimental support for this hypothesis. Ramachandra and Wikel showed that salivary gland extracts from the tick Dermacentor andersoni reduced IL-1 levels during the early phases of tick feeding [54], whereas Fuchsberger et al., 1995 determined that human IL-1β secretion was mitigated when treated with LPS and salivary gland extracts from partially fed adult female Rhipicephalus appendiculatus[55].
In addition, A. phagocytophilum may need redundant mechanisms of innate immune recognition to trigger IL-1β secretion. Secretion of IL-1β requires NF-κB activation to generate pro-IL-1β [56, 57]. Dumler and colleagues demonstrated that A. phagocytophilum triggers TLR2 activation during immune cell stimulation [58]. TLR activation is known to initiate NF-κB signaling in immune cells [59]. More recently, our group participated in a study showing that receptor interacting protein-2 (RIP2) affects A. phagocytophilum infection in mice [60]. RIP2 is an adaptor molecule for the innate immune receptors Nod1/2, which also regulates NF-κB signaling [61]. Finally, assembly of a multi-protein complex coined “inflammasome” is critical for IL-1β secretion [56, 57]. We previously demonstrated that the inflammasome is critical for immunity against A. phagocytophilum infection [52]. Taken together, our findings reinforce the notion that A. phagocytophilum immunity is multi-factorial, and suggests a holistic inhibitory effect of tick saliva on innate immunity. This is important because a pathogen such as A. phagocytophilum may need multiple layers of immune evasion during transmission. Therefore, the holistic properties of tick saliva may be a major strategy of host immune evasion during pathogen transmission.
The above hypothesis is supported by several lines of evidence. Post-genomic approaches show that A. phagocytophilum actively modulates gene expression in ticks [62, 63]. Recently, the P11 salivary protein was shown to be required for A. phagocytophilum migration from hemocytes to the salivary glands in ticks [64]. Another salivary gland protein named SALP16 was deemed important for A. phagocytophilum survival within the tick vector [65]. A. phagocytophilum alters the monomeric/filamentous (G/F) actin ratio leading to the translocation of phosphorylated/G-actin to the nucleus [66]. This event affects salp16 gene transcription in association with the RNA polymerase II (RNAPII) and the TATA-binding protein. Fikrig and colleagues have also demonstrated that A. phagocytophilum appears to increase the ability of I. scapularis to survive in cold temperatures by up-regulating an antifreeze glycoprotein [67] and α1, 3- fucosyltransferases, which are important for pathogen colonization [68]. On the other hand, the Janus kinase (JAK)-signaling transducer activator of transcription (STAT) pathway seems to be important for the restriction of A. phagocytophilum infection in ticks. Clearly, further studies are necessary to determine the contribution of salivary proteins to A. phagocytophilum pathogenesis and immunity.
Elucidating the underlying effect of tick saliva in vivo should be considered a high-priority in tick research. Several experiments show that findings obtained in vitro may sometimes differ from those occurring in vivo, and mRNA and protein levels do not necessarily correlate well [1]. In vivo characterization of tick salivary proteins, however, is not a trivial task. The presence of multiple paralogues in the I. scapularis genome [53] make the use of siRNA or dsRNA technology challenging because of known off-target effects [69]. Another technical limitation is the lack of strategies to introduce and/or delete genes in ticks. Thereby, we were unable to generate knock-out, knock-in or transgenic I. scapularis. The development of this technology would enable researchers to characterize tick salivary proteins and clarify underlying events at the vector-pathogen-host interface. Despite all these technical restrictions, we posit that I. scapularis saliva may inhibit cytokine secretion during rickettsial transmission. We look forward with reasonable confidence that our findings may be used as a prelude for future in-vivo experimentation.
Conclusions
To facilitate blood-feeding habits and counteract homeostasis and inflammation in the host, arthropod vectors have evolved a sophisticated pharmacological portfolio. Our studies add to a continuum of research over the past 20–30 years and show that I. scapularis saliva diminishes cytokine secretion by mouse and human immune cells during TLR and NLR stimulation. We also show that cytokine response by macrophages is diminished in the presence of I. scapularis saliva during A. phagocytophilum stimulation. Taken together, our findings should pave the ground for new research directions in the field of A. phagocytophilum pathogenesis and immunity and may have direct implications for understanding how ticks circumvent defenses promoted by the mammalian immune system.
Abbreviations
- TLRs:
-
Toll-like receptors
- NLRs:
-
Nod-like receptors
- NF-κB:
-
Nuclear factor
- IL:
-
Interleukin
- TNF-α:
-
Tumor Necrosis Factor
- PAMPs:
-
Pathogen Associated Molecular Patterns
- LPS:
-
Lipopolysaccharide
- MDP:
-
Muramyl dipeptide
- BMDMs:
-
Bone marrow-derived macrophages
- PBMCs:
-
Peripheral blood mononuclear cells.
References
Francischetti IM, Sa-Nunes A, Mans BJ, Santos IM, Ribeiro JM: The role of saliva in tick feeding. Front Biosci. 2009, 14: 2051-2088.
Fontaine A, Diouf I, Bakkali N, Misse D, Pages F, Fusai T, Rogier C, Almeras L: Implication of haematophagous arthropod salivary proteins in host-vector interactions. Parasit Vectors. 2011, 4: 187-10.1186/1756-3305-4-187.
Andersen JF: Structure and mechanism in salivary proteins from blood-feeding arthropods. Toxicon. 2010, 56 (7): 1120-1129. 10.1016/j.toxicon.2009.11.002.
Chmelar J, Calvo E, Pedra JH, Francischetti IM, Kotsyfakis M: Tick salivary secretion as a source of antihemostatics. J Proteomics. 2012, 75 (13): 3842-3854. 10.1016/j.jprot.2012.04.026.
Valenzuela JG: Exploring tick saliva: from biochemistry to ‘sialomes’ and functional genomics. Parasitology. 2004, 129 (Suppl): S83-S94.
Paesen GC, Adams PL, Nuttall PA, Stuart DL: Tick histamine-binding proteins: lipocalins with a second binding cavity. Biochim Biophys Acta. 2000, 1482 (1–2): 92-101.
Dai J, Narasimhan S, Zhang L, Liu L, Wang P, Fikrig E: Tick histamine release factor is critical for Ixodes scapularis engorgement and transmission of the Lyme disease agent. PLoS Pathog. 2010, 6 (11): e1001205-10.1371/journal.ppat.1001205.
Hovius JW, Levi M, Fikrig E: Salivating for knowledge: potential pharmacological agents in tick saliva. PLoS Med. 2008, 5 (2): e43-10.1371/journal.pmed.0050043.
Brossard M, Wikel SK: Tick immunobiology. Parasitology. 2004, 129 (Suppl): S161-S176.
Titus RG, Bishop JV, Mejia JS: The immunomodulatory factors of arthropod saliva and the potential for these factors to serve as vaccine targets to prevent pathogen transmission. Parasite Immunol. 2006, 28 (4): 131-141.
Bowman AS, Sauer JR: Tick salivary glands: function, physiology and future. Parasitology. 2004, 129 (Suppl): S67-S81.
Kaufman WR: Tick-host interaction: a synthesis of current concepts. Parasitol Today. 1989, 5 (2): 47-56. 10.1016/0169-4758(89)90191-9.
Ribeiro JM: Role of saliva in tick/host interactions. Exp Appl Acarol. 1989, 7 (1): 15-20. 10.1007/BF01200449.
Nuttall PA: Displaced tick-parasite interactions at the host interface. Parasitology. 1998, 116 (Suppl): S65-S72.
Wikel SK: Tick modulation of host immunity: an important factor in pathogen transmission. Int J Parasitol. 1999, 29 (6): 851-859. 10.1016/S0020-7519(99)00042-9.
Bowman AS, Dillwith JW, Sauer JR: Tick salivary prostaglandins: Presence, origin and significance. Parasitol Today. 1996, 12 (10): 388-396. 10.1016/0169-4758(96)10061-2.
Oliveira CJ, Sa-Nunes A, Francischetti IM, Carregaro V, Anatriello E, Silva JS, Santos IK, Ribeiro JM, Ferreira BR: Deconstructing tick saliva: non-protein molecules with potent immunomodulatory properties. J Biol Chem. 2011, 286 (13): 10960-10969. 10.1074/jbc.M110.205047.
Valenzuela JG, Charlab R, Mather TN, Ribeiro JM: Purification, cloning, and expression of a novel salivary anticomplement protein from the tick, Ixodes scapularis. J Biol Chem. 2000, 275 (25): 18717-18723. 10.1074/jbc.M001486200.
Schuijt TJ, Coumou J, Narasimhan S, Dai J, Deponte K, Wouters D, Brouwer M, Oei A, Roelofs JJ, van Dam AP: A tick mannose-binding lectin inhibitor interferes with the vertebrate complement cascade to enhance transmission of the Lyme disease agent. Cell Host Microbe. 2011, 10 (2): 136-146. 10.1016/j.chom.2011.06.010.
Ashish J, Garg R, Boone CD, Anguita J, Krueger JK, IJ : Conformational rearrangement within the soluble domains of the CD4 receptor is ligand-specific. J Biol Chem. 2008, 283 (5): 2761-2772.
Juncadella IJ, Garg R, Ananthnarayanan SK, Yengo CM, Anguita J: T-cell signaling pathways inhibited by the tick saliva immunosuppressor, Salp15. FEMS Immunol Med Microbiol. 2007, 49 (3): 433-438. 10.1111/j.1574-695X.2007.00223.x.
Garg R, Juncadella IJ, Ramamoorthi N, Ashish Ananthanarayanan SK, Thomas V, Rincon M, Krueger JK, Fikrig E, Yengo CM: CD4 is the receptor for the tick saliva immunosuppressor, Salp15. J Immunol. 2006, 177 (10): 6579-6583.
Anguita J, Ramamoorthi N, Hovius JW, Das S, Thomas V, Persinski R, Conze D, Askenase PW, Rincon M, Kantor FS: Salp15, an Ixodes scapularis salivary protein, inhibits CD4(+) T cell activation. Immunity. 2002, 16 (6): 849-859. 10.1016/S1074-7613(02)00325-4.
Hovius JW, de Jong MA, den Dunnen J, Litjens M, Fikrig E, van der Poll T, Gringhuis SI, Geijtenbeek TB: Salp15 binding to DC-SIGN inhibits cytokine expression by impairing both nucleosome remodeling and mRNA stabilization. PLoS Pathog. 2008, 4 (2): e31-10.1371/journal.ppat.0040031.
Hannier S, Liversidge J, Sternberg JM, Bowman AS: Characterization of the B-cell inhibitory protein factor in Ixodes ricinus tick saliva: a potential role in enhanced Borrelia burgdoferi transmission. Immunology. 2004, 113 (3): 401-408. 10.1111/j.1365-2567.2004.01975.x.
Titus RG, Ribeiro JM: Salivary gland lysates from the sand fly Lutzomyia longipalpis enhance Leishmania infectivity. Science. 1988, 239 (4845): 1306-1308. 10.1126/science.3344436.
Ramamoorthi N, Narasimhan S, Pal U, Bao F, Yang XF, Fish D, Anguita J, Norgard MV, Kantor FS, Anderson JF: The Lyme disease agent exploits a tick protein to infect the mammalian host. Nature. 2005, 436 (7050): 573-577. 10.1038/nature03812.
Kotsyfakis M, Horka H, Salat J, Andersen JF: The crystal structures of two salivary cystatins from the tick Ixodes scapularis and the effect of these inhibitors on the establishment of Borrelia burgdorferi infection in a murine model. Mol Microbiol. 2010, 77 (2): 456-470. 10.1111/j.1365-2958.2010.07220.x.
Lieskovska J, Kopecky J: Effect of tick saliva on signalling pathways activated by TLR-2 ligand and Borrelia afzelii in dendritic cells. Parasite Immunol. 2012, 34 (8–9): 421-429.
Lieskovska J, Kopecky J: Tick saliva suppresses IFN signalling in dendritic cells upon Borrelia afzelii infection. Parasite Immunol. 2012, 34 (1): 32-39. 10.1111/j.1365-3024.2011.01345.x.
Labuda M, Trimnell AR, Lickova M, Kazimirova M, Davies GM, Lissina O, Hails RS, Nuttall PA: An antivector vaccine protects against a lethal vector-borne pathogen. PLoS Pathog. 2006, 2 (4): e27-10.1371/journal.ppat.0020027.
Severo MS, Stephens KD, Kotsyfakis M, Pedra JH: Anaplasma phagocytophilum: deceptively simple or simply deceptive?. Future Microbiol. 2012, 7 (6): 719-731. 10.2217/fmb.12.45.
Chen G, Severo MS, Sakhon OS, Choy A, Herron MJ, Felsheim RF, Wiryawan H, Liao J, Johns JL, Munderloh UG: Anaplasma phagocytophilum LPDA1 affects host-derived immunopathology during microbial colonization. Infect Immun. 2012, 80 (9): 3194-3205. 10.1128/IAI.00532-12.
Eisenbarth SC, Colegio OR, O’Connor W, Sutterwala FS, Flavell RA: Crucial role for the Nalp3 inflammasome in the immunostimulatory properties of aluminium adjuvants. Nature. 2008, 453 (7198): 1122-1126. 10.1038/nature06939.
Ribeiro JM, Zeidner NS, Ledin K, Dolan MC, Mather TN: How much pilocarpine contaminates pilocarpine-induced tick saliva?. Med Vet Entomol. 2004, 18 (1): 20-24. 10.1111/j.0269-283X.2003.0469.x.
Katavolos P, Armstrong PM, Dawson JE, Telford SR: Duration of tick attachment required for transmission of granulocytic ehrlichiosis. J Infect Dis. 1998, 177 (5): 1422-1425. 10.1086/517829.
Hodzic E, Fish D, Maretzki CM, De Silva AM, Feng S, Barthold SW: Acquisition and transmission of the agent of human granulocytic ehrlichiosis by Ixodes scapularis ticks. J Clin Microbiol. 1998, 36 (12): 3574-3578.
Vignes-des F, Piesman J, Heffernan R, Schulze TL, Fish D, Stafford KC: Effect of tick removal on transmission of Borrelia burgdorferi and Ehrlichia phagocytophila by Ixodes scapularis nymphs. J Infect Dis. 2001, 183 (5): 773-778. 10.1086/318818.
Ting JP, Duncan JA, Lei Y: How the noninflammasome NLRs function in the innate immune system. Science. 2010, 327 (5963): 286-290. 10.1126/science.1184004.
Sun SC: The noncanonical NF-κB pathway. Immunol Rev. 2012, 246 (1): 125-140. 10.1111/j.1600-065X.2011.01088.x.
Tiemi Shio M, Eisenbarth SC, Savaria M, Vinet AF, Bellemare MJ, Harder KW, Sutterwala FS, Bohle DS, Descoteaux A, Flavell RA: Malarial hemozoin activates the NLRP3 inflammasome through Lyn and Syk kinases. PLoS Pathog. 2009, 5 (8): e1000559-10.1371/journal.ppat.1000559.
Schroder K, Zhou R, Tschopp J: The NLRP3 inflammasome: a sensor for metabolic danger?. Science. 2010, 327 (5963): 296-300. 10.1126/science.1184003.
Latz E: The inflammasomes: mechanisms of activation and function. Curr Opin Immunol. 2010, 22 (1): 28-33. 10.1016/j.coi.2009.12.004.
Hotopp JC, Lin M, Madupu R, Crabtree J, Angiuoli SV, Eisen JA, Seshadri R, Ren Q, Wu M, Utterback TR: Comparative genomics of emerging human ehrlichiosis agents. PLoS Genet. 2006, 2 (2): e21-10.1371/journal.pgen.0020021.
Strowig T, Henao-Mejia J, Elinav E, Flavell R: Inflammasomes in health and disease. Nature. 2012, 481 (7381): 278-286. 10.1038/nature10759.
Rikihisa Y: Anaplasma phagocytophilum and Ehrlichia chaffeensis: subversive manipulators of host cells. Nat Rev Microbiol. 2010, 8 (5): 328-339. 10.1038/nrmicro2318.
Newton K, Dixit VM: Signaling in innate immunity and inflammation. Cold Spring Harb Perspect Biol. 2012, 4 (3): 1-19.
Oliveira CJ, Carvalho WA, Garcia GR, Gutierrez FR, Silva JS, Ferreira BR, de Miranda Santos IK: Tick saliva induces regulatory dendritic cells: MAP-kinases and Toll-like receptor-2 expression as potential targets. Vet Parasitol. 2009, 167: 288-297.
Cavassani KA, Aliberti JC, Dias AR, Silva JS, Ferreira BR: Tick saliva inhibits differentiation, maturation and function of murine bone-marrow-derived dendritic cells. Immunology. 2005, 114 (2): 235-245. 10.1111/j.1365-2567.2004.02079.x.
Sa-Nunes A, Bafica A, Lucas DA, Conrads TP, Veenstra TD, Andersen JF, Mather TN, Ribeiro JM, Francischetti IM: Prostaglandin E2 is a major inhibitor of dendritic cell maturation and function in Ixodes scapularis saliva. J Immunol. 2007, 179 (3): 1497-1505.
Kim HY, Rikihisa Y: Roles of p38 mitogen-activated protein kinase, NF-κB, and protein kinase C in proinflammatory cytokine mRNA expression by human peripheral blood leukocytes, monocytes, and neutrophils in response to Anaplasma phagocytophila. Infect Immunity. 2002, 70 (8): 4132-4141. 10.1128/IAI.70.8.4132-4141.2002.
Pedra JH, Sutterwala FS, Sukumaran B, Ogura Y, Qian F, Montgomery RR, Flavell RA, Fikrig E: ASC/PYCARD and caspase-1 regulate the IL-18/IFN-γ axis during Anaplasma phagocytophilum infection. J Immunol. 2007, 179 (7): 4783-4791.
Pagel Van Zee J, Geraci NS, Guerrero FD, Wikel SK, Stuart JJ, Nene VM, Hill CA: Tick genomics: the Ixodes genome project and beyond. Int J Parasitol. 2007, 37 (12): 1297-1305. 10.1016/j.ijpara.2007.05.011.
Ramachandra RN, Wikel SK: Modulation of host-immune responses by ticks (Acari: Ixodidae): effect of salivary gland extracts on host macrophages and lymphocyte cytokine production. J Med Entomol. 1992, 29 (5): 818-826.
Fuchsberger N, Kita M, Hajnicka V, Imanishi J, Labuda M, Nuttall PA: Ixodid tick salivary gland extracts inhibit production of lipopolysaccharide-induced mRNA of several different human cytokines. Exp Appl Acarol. 1995, 19 (11): 671-676. 10.1007/BF00145255.
Franchi L, Munoz-Planillo R, Nunez G: Sensing and reacting to microbes through the inflammasomes. Nature Immunol. 2012, 13 (4): 325-332. 10.1038/ni.2231.
Davis BK, Wen H, Ting JP: The inflammasome NLRs in immunity, inflammation, and associated diseases. Annu Rev Immunol. 2011, 29: 707-735. 10.1146/annurev-immunol-031210-101405.
Choi KS, Scorpio DG, Dumler JS: Anaplasma phagocytophilum ligation to toll-like receptor (TLR) 2, but not to TLR4, activates macrophages for nuclear factor-κB nuclear translocation. J Infect Dis. 2004, 189 (10): 1921-1925. 10.1086/386284.
Schroder K, Tschopp J: The inflammasomes. Cell. 2010, 140 (6): 821-832. 10.1016/j.cell.2010.01.040.
Sukumaran B, Ogura Y, Pedra JH, Kobayashi KS, Flavell RA, Fikrig E: Receptor interacting protein-2 contributes to host defense against Anaplasma phagocytophilum infection. FEMS Immunol Med M. 2012, 10.1111/j.1574-695X.2012.01001.x..
Sorbara MT, Philpott DJ: Peptidoglycan: a critical activator of the mammalian immune system during infection and homeostasis. Immunol Rev. 2011, 243 (1): 40-60. 10.1111/j.1600-065X.2011.01047.x.
Mastronunzio JE, Kurscheid S, Fikrig E: Post-genomic analyses reveal development of infectious Anaplasma phagocytophilum during transmission from ticks to mice. J Bacteriol. 2012, 194 (9): 2238-2247. 10.1128/JB.06791-11.
Munderloh UG, Jauron SD, Fingerle V, Leitritz L, Hayes SF, Hautman JM, Nelson CM, Huberty BW, Kurtti TJ, Ahlstrand GG: Invasion and intracellular development of the human granulocytic ehrlichiosis agent in tick cell culture. J Clin Microbiol. 1999, 37 (8): 2518-2524.
Liu L, Narasimhan S, Dai J, Zhang L, Cheng G, Fikrig E: Ixodes scapularis salivary gland protein P11 facilitates migration of Anaplasma phagocytophilum from the tick gut to salivary glands. EMBO Rep. 2011, 12: 1196-1203. 10.1038/embor.2011.177.
Sukumaran B, Narasimhan S, Anderson J, DePont K, Marcantonio N, Krishnan M, Fish D, Telford S, Kantor F, Fikrig E: An Ixodes scapularis protein required for survival of Anaplasma phagocytophilum in tick salivary glands. J Exp Med. 2006, 203: 1507-1517. 10.1084/jem.20060208.
Sultana H, Neelakanta G, Kantor F, Malawista S, Fish D, Montgomery R, Fikrig E: Anaplasma phagocytophilum induces actin phosphorylation to selectively regulate gene transcription in Ixodes scapularis ticks. J Exp Med. 2010, 207: 1727-1743. 10.1084/jem.20100276.
Neelakanta G, Sultana H, Fish D, Anderson J, Fikrig E: Anaplasma phagocytophilum induces Ixodes scapularis ticks to express an antifreeze glycoprotein gene that enhances their survival in the cold. J Clin Invest. 2010, 120: 3179-3190. 10.1172/JCI42868.
Pedra J, Narasimhan S, Rendić D, DePonte K, Bell-Sakyi L, Wilson I, Fikrig E: Fucosylation enhances colonization of ticks by Anaplasma phagocytophilum. Cell Microbiol. 2010, 12: 1222-1234. 10.1111/j.1462-5822.2010.01464.x.
Lew-Tabor AE, Kurscheid S, Barrero R, Gondro C, Moolhuijzen PM, Rodriguez-Valle M, Morgan JA, Covacin C, Bellgard MI: Gene expression evidence for off-target effects caused by RNA interference-mediated gene silencing of ubiquitin-63E in the cattle tick Rhipicephalus microplus. Int J Parasitol. 2011, 41 (9): 1001-1014. 10.1016/j.ijpara.2011.05.003.
Acknowledgements
We acknowledge Sukanya Narasimhan and Kathy DePonte for providing tick saliva. This work was supported by a cooperative agreement K01 CK000101 from the Centers for Disease Control and Prevention, the initial complement provided by the University of California (to JHFP), public health service grant R01 AI093653 (to JHFP), an International Graduate Student Fellowship awarded by the American Association of University Women (to MSS), a Jan Evangelista Purkyne fellowship of the National Academy of Sciences of the Czech Republic and a Marie Curie Reintegration grant of the EU-FP7 (PIRG07-GA-2010-268177) (to MK).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
GC, MSS, MS and OSS carried out the experimental work. SKW and MK analyzed the data and provided intellectual support. JHFP directed the project and wrote the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Chen, G., Severo, M.S., Sohail, M. et al. Ixodes scapularis saliva mitigates inflammatory cytokine secretion during Anaplasma phagocytophilum stimulation of immune cells. Parasites Vectors 5, 229 (2012). https://doi.org/10.1186/1756-3305-5-229
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1756-3305-5-229