Abstract
Background
In comparison to the conventional whole-prostate dose escalation, an integrated boost to the macroscopic malignant lesion might potentially improve tumor control rates without increasing toxicity. Quality of life after radiotherapy (RT) with vs. without 18F-choline PET-CT detected simultaneous integrated boost (SIB) was prospectively evaluated in this study.
Methods
Whole body image acquisition in supine patient position followed 1 h after injection of 178-355MBq 18F-choline. SIB was defined by a tumor-to-background uptake value ratio > 2 (GTVPET). A dose of 76Gy was prescribed to the prostate (PTVprostate) in 2Gy fractions, with or without SIB up to 80Gy. Patients treated with (n = 46) vs. without (n = 21) SIB were surveyed prospectively before (A), at the last day of RT (B) and a median time of two (C) and 19 month (D) after RT to compare QoL changes applying a validated questionnaire (EPIC - expanded prostate cancer index composite).
Results
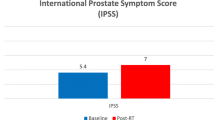
With a median cut-off standard uptake value (SUV) of 3, a median GTVPET of 4.0 cm3 and PTVboost (GTVPET with margins) of 17.3 cm3 was defined. No significant differences were found for patients treated with vs. without SIB regarding urinary and bowel QoL changes at times B, C and D (mean differences ≤3 points for all comparisons). Significantly decreasing acute urinary and bowel score changes (mean changes > 5 points in comparison to baseline level at time A) were found for patients with and without SIB. However, long-term urinary and bowel QoL (time D) did not differ relative to baseline levels - with mean urinary and bowel function score changes < 3 points in both groups (median changes = 0 points). Only sexual function scores decreased significantly (> 5 points) at time D.
Conclusions
Treatment planning with 18F-choline PET-CT allows a dose escalation to a macroscopic intraprostatic lesion without significantly increasing toxicity.
Similar content being viewed by others
Background
Increasing doses for prostate cancer have been shown to be associated with improved biochemical control rates in several prospective randomized studies [1]. However, rectal toxicity has also increased significantly. Rectal toxicity is known to be the dose-limiting toxicity in prostate cancer radiotherapy [2, 3]. Focusing the dose escalation on the actual tumour has the potential to increase tumour control without increasing toxicity.
Local prostate cancer recurrence after primary radiotherapy (RT) usually originates in the location of the primary tumor. Cellini et al. found the origin of all local recurrences within the initial tumor volume, supporting the rationale of a selective dose escalation only to the intraprostatic lesion [4]. In view of an often multifocal microscopic spread of prostate cancer [5] - not possible to delineate with the presently available imaging modalities - the whole prostate has still to be covered by an effective dose.
Treatment was based on 18F-choline PET-CT (positron emission tomography and computed tomography acquired in same patient position) for patients in focus of this study. A simultaneous integrated boost (SIB) was delivered to the GTVPET (gross target volume, as defined in PET). Quality of life (QoL) changes were evaluated prospectively and compared to a patient group treated with the same concept in the same time interval - but without a SIB - to demonstrate an acceptable treatment tolerance and a rationale to continue this innovative strategy.
In contrast to grading scales, for example the commonly applied RTOG/EORTC (Radiation Therapy Oncology Group/European Organisation of Research and Treatment of Cancer) scale, QoL questionnaires have the advantage of revealing all grades of toxicity from the patient's perspective. Baseline problems can be taken into account accurately.
Methods
Treatment planning
This prospective study was based on consecutive patients who were treated due to localized T1-3N0M0 prostatic carcinoma in the years 2008-2009. PET-CT (Philips Gemini TF 16) with 18F-choline was performed in 46 patients for treatment planning. Image acquisition in supine patient position followed 1 h after injection of 178-355MBq 18F-choline. Images were reconstructed using the iterative LOR (line of response) algorithm (pixel size: 4 mm3). CT images (from PET-CT) with a slice thickness of 3 mm were used for treatment planning.
The CTV (prostate volume ± base of seminal vesicles), bladder and rectum (region from anal canal to the rectosigmoid flexure) were delineated by identifying the external contours (Philips Pinnacle3 Version 8.0 m). GTVPET (intraprostatic lesion) was defined by a tumour-to-background choline uptake ratio > 2, based on the results of studies correlating choline PET results with histopathologic examinations [6, 7]. We have identified an area of about 1 cm2 within the prostate with the lowest activity and defined the threshold for GTVPET after multiplying the SUVmax (maximum standard uptake value) in this area by 2 [8].
For the planning target volume (PTV), 8 mm lateral and anterior, 5 mm superior and inferior and 4 mm posterior margin was added. A uniform margin of 4 mm was added to the GTVPET to account for intrafraction target motion, with the exception of the posterior direction (3 mm). Intrafraction prostate displacements have been evaluated in our department recently using ultrasound based image-guided radiotherapy (IGRT) - the required margins were calculated to be ≤4 mm in all directions, with 85% of displacements within a margin of 3 mm [9]. Ultrasound based IGRT was applied before each fraction for patient positioning for all patients using the BAT® SXi system (B-mode acquisition and targeting).
An inverse planning with a five field step-and-shoot intensity-modulated radiotherapy (IMRT) technique and 15MeV photons was used. The direct machine parameter optimization (DMPO) algorithm was applied for inverse planning with a 2 cm2 minimum segment area, 5 minimum segment monitor units and a maximum number of 70 segments. The dose to the PTV was prescribed to a reference point (outside the volume of GTVPET). Treatment planning objectives are summarised in Table 1. Examples are shown in Figure 1.
Quality of life and treatment plans for patients who were treated with SIB were compared with patients treated without SIB in the same period (n = 21) - boost volume has either have not been defined or 18F-choline PET-CT has not been performed due to logistic reasons. Tumour based criteria had no relevance for the selection to treat with or without SIB. With the exception of the SIB, the same treatment planning and treatment delivery technique was used for patients without SIB (daily IGRT and five field IMRT).
We have focused on the EUD (equivalent uniform dose) for the PTV, rectum and bladder and the NTCP (normal tissue complication probability) for the rectum and bladder.
N = voxel number; Di = dose in the i'th voxel; a = tumour or normal tissue-specific parameter that describes the dose-volume effect; with a = -10 for prostate cancer and a = 6 for bladder and rectum in this study [8].
NTCP for grade 3 or worse rectum and bladder toxicity was computed applying the Lyman-Kutcher-Burman model with Emami parameters (rectum: n = 0.12, m = 0.15, median toxicity dose = 80Gy; bladder: n = 0.5, m = 0.11; median toxicity dose = 80Gy) [10, 11].
Quality of life evaluation
Patients were surveyed prospectively before (time A), at the last day (B), and a median time of two months (range 6 weeks-6 months) after (C) and 19 months (range 14-24 months) after (D) radiotherapy using a validated questionnaire, the Expanded Prostate Cancer Index Composite (EPIC) [12, 13]. The questionnaire comprises 50 items concerning the urinary, bowel, sexual and hormonal domains for function and bothersomeness. The multi-item scale scores were transformed lineary to a 0-100 scale, with higher scores representing better QoL. According to data in the literature, mean QoL changes of below 5 points can be defined as clinically not significant, 5-10 as "little" changes, 10-20 as "moderate" changes and > 20 as "very much" changes [14]. Other authors use the "0.5 standard deviation of baseline value" to determine clinically relevant changes [14] - this is also reported in this study. A baseline questionnaire was required for inclusion in this study resulting in a total number of 46/21 (time A), 38/16 (time B), 44/21 (time C) and 44/20 (time D) questionnaires after treatment with/without SIB.
The questionnaire was handed over to the patients personally by one of the physicians at time A, B and C. Number of questionnaires was the lowest at the end of radiotherapy (time B) because this point in time was limited to a single day (last radiotherapy fraction) and there was no second opportunity to fill out a missed questionnaire. Patients presented in the department six to ten weeks after the end of treatment. Missed questionnaires in the acute phase (time C) and questionnaires one to two years after radiotherapy (time D) were sent to the patients with a return envelope. If a questionnaire was not returned within 4 weeks, patients were contacted by telephone and were urged to complete it. The median time after treatment and the respective ranges for the questionnaires C and D were the same for patients after treatment with and without SIB.
Statistical analysis
Statistical analysis was performed using the IBM SPSS 19.0 software. The Wilcoxon's matched-pairs test was applied to determine longitudinal changes in specific subgroups of patients. To explore statistical volume or dose differences in treatment plans and QoL score differences between different subgroups at a specific time, the Mann-Whitney-U-test was used. Contingency table analysis with the chi-square test was performed to compare treatment groups with respect to categorical variables. All p-values reported are two-sided, p < 0.05 is considered significant.
Results
Demographic and treatment plan-related data are presented in Table 2, showing well comparable (statistically not significantly different) distribution of prognostic factors and organ volumes for treatment planning. Median EUD values for patients treated with SIB were 2% higher in comparison to patients without SIB, with slightly higher NTCP for rectal toxicity. However, only the EUD for PTVprostate was significantly higher for patients treated with SIB (p > 0.05 for all other comparisons).
With a median cut-off standard uptake value (SUV) of 3, a median GTVPET of 4.0 cm3 and PTVboost (GTVPET with margins) of 17.3 cm3 was defined. Malignant lesions were defined as single lesions in 31%, as two bilateral lesions in 26%, as central lesions extending into both lobes in 30% and as multiple (at least three) lesions in 13%.
Baseline QoL scores have not been found to be significantly different (Table 3) for patients treated with or without SIB. No significant differences were found regarding urinary, bowel and sexual QoL changes at times B, C and D (mean differences ≤3 points for all comparisons in urinary and bowel domains). Significantly decreasing acute urinary and bowel scores changes (clinically relevant: mean changes > 5 points in comparison to baseline level at time A; > 0.5 standard deviation of baseline value) were found for patients with and without SIB. However, long-term urinary and bowel QoL (time D) did not differ relative to baseline levels - with mean urinary and bowel function score changes < 3 points in both groups (median changes = 0 points).
Only sexual scores decreased significantly (> 5 points; all mean changes < 0.5 standard deviation of baseline value) at time D. As sexual scores demonstrate the largest variability (Table 3), a possible decrease strongly depends on the baseline scores. Sexual function scores of patients with a baseline sexual function score < 25 did not change > 5 points at time D in comparison to baseline in both subgroups. However, sexual function scores of patients with a baseline sexual function scores of 25-50 and > 50 decreased 12 points in both subgroups and 11/15 points in the subgroup treated with/without SIB, respectively. Considering only patients with higher baseline scores (> 25 points), changes more than a year after the end of radiotherapy also exceeded the 0.5 of standard deviation threshold (p < 0.01 and p = 0.02 with and without SIB). At time D, 75% and 60% of patients in the prostate with SIB and prostate only groups who reported erections sufficient for sexual intercourse before treatment retained this ability.
The rates of reporting big or moderate bother with specific symptoms are shown in Table 4. In accordance with the corresponding scores, the greatest changes were reported in the acute phase at the end of treatment for irritative symptoms - or urinary and bowel function overall. Significant differences between the subgroups with or without SIB have not been found. Remarkably, not a single patient reported big or moderate bother with bloody stools at times C or D. Mean bleeding function scores were 98 points at all response intervals (times A, B, C and D) in the subgroup with SIB.
GTVPET volumes and distances to the bladder and rectum wall were evaluated in the subgroup of patients who were treated with SIB (Table 5; < or ≥median, respectively). A tendency for larger QoL changes was found for patients with larger GTVPET volumes and closer distances to the bladder and rectum wall. In contrast to a faster return to baseline levels at time C of patients with GTVPET < 4 cm3, a distance to the bladder ≥1 cm and a distance to the rectum wall ≥3 mm, scores of patients with GTVPET > 4 cm3 (bowel bother) a distance to the bladder < 1 cm (urinary bother) and a distance to the rectum wall < 3 mm (bowel bother) were still significantly higher at time C in comparison to baseline levels. The difference exceeded 5 points and the 0.5 standard deviation of baseline level threshold with the exception urinary bother scores in case of a GTVPET > 4 cm3. No statistically significant differences relative to baseline levels were found in any subgroup at time D.
Discussion
The whole prostate is the standard target volume for external beam radiotherapy and brachytherapy for localised prostate cancer, as prostate cancer is known to be a multifocal disease and diagnosis of microscopic cancer is not possible with presently available imaging modalities [5]. However, advances in imaging and radiotherapy techniques offer innovative treatment possibilities [15]. Treatment planning with 18F-choline PET-CT allows a dose escalation to a macroscopic intraprostatic lesion without increasing toxicity.
Magnetic resonance imaging (MRI), magnetic resonance spectroscopy (MRS) and choline PET/CT are suitable methods to localize intraprostatic lesions with an adequate sensitivity and specificity [6, 7, 16, 17]. Choline acts as a precursor for the biosynthesis of phospholipids, e.g. phosphatidylcholine, the major component of the plasma membrane. The uptake of choline reflects both proliferation and signaling in transformed cells [18]. Elevated choline to citrate ratios are used to discriminate prostate cancer in MRS imaging [16]. Disadvantages of MRS in comparison to PET imaging are larger voxel sizes (usually at least 1 cm3 vs. 4 mm3) and a more strenuous and subjective analysis of the data.
Image-guided radiotherapy (IGRT) and IMRT are prerequisites for applying the simultaneous integrated boost concept. IGRT techniques eliminate inaccuracies due to interfractional prostate displacement and help to minimize safety margins considerably. IMRT brings the opportunity to deliver heterogeneous dose prescriptions within the target. The simultaneous integrated boost concept has been rapidly adopted for the IMRT of head and neck cancer patients [19]. Dose escalation in the area of the primary macroscopic tumour is also applied in several other regions, probably most frequently for breast cancer - the clinical benefit on local control has been demonstrated [20].
In a recently published study, an intraprostatic lesion could be identified in 65 of 66 consecutive patients after performing 18F-choline PET-CT [21]. GTVPET and SUV levels were found to depend on prognostic risk factors, particularly a Gleason score > 7. Increasing PET-defined tumor volumes and increasing SUV levels correlated well with increasing prognostic risk. Though antiandrogen hormonal therapy is known to decrease choline uptake in prostate cancer [19], the identification of a lesion is still possible after NHT. SUV levels in intraprostatic lesions were comparable to patients without NHT. NHT or a prior radiation dose to the prostate reduces cell metabolism and absolute SUV both in the tumour and the benign prostate tissue [22]. A relative SUV threshold seems to be a more reasonable definition for these patients. The ratio between tumour and normal tissue is the key to identifying aggressive disease [23].
Treatment planning studies evaluating the impact of the simultaneous integrated boost have been already published, demonstrating the potential of a considerable dose escalation to the macroscopically defined tumor without significantly increasing the dose to the organs at risk or NTCP [8, 24]. These results are supported by the treatment plan-related data of the patients in this study. EUD and NTCP values for the rectum and bladder have not been found to differ significantly between patients treated with or without SIB.
Quality of life evaluations after radiotherapy for prostate cancer with a SIB have not been published before. The results of this clinical study well support the results of prior treatment planning studies [8, 24]. The additional SIB did not increase QoL changes in the acute phase or more than one year after radiotherapy. Generally, the treatment was very well tolerated. Even with larger SIB volumes and close distances to the bladder and/or rectum walls, mean long-term urinary and bladder QoL scores did not decrease more than 5 points (or 0.5 standard deviation) in comparison to the baseline level. Treatment tolerance did not decrease in comparison to our patients who were treated up to total doses of 70.2-72Gy using three-dimensional conformal planning without IGRT [2, 3] (data presented in prior publications). In particular, rectal bleeding - usually in focus of rectal toxicity after radiotherapy for prostate cancer [2, 3]- has not been found to be considerably relevant for the patients. A clinically relevant QoL change was only found in the sexual domain for patients with higher baseline sexual function scores, without a significant difference with vs. without SIB.
Acute toxicity results up to three months after RT with an MRI/MRS detected SIB have been published by Fonteyne et al. [16]. An intraprostatic lesion was identified in only 118 of 230 patients - a considerably lower percentage in comparison to treatment planning after 18F-choline PET-CT. The severity and incidence of acute toxicity did not increase for patients treated with SIB. However, the authors did not consider any margin around the intraprostatic lesion.
Conclusions
According to the results of this prospective non-randomized study, treatment planning with 18F-choline PET-CT allows a dose escalation to a macroscopic intraprostatic lesion without increasing toxicity. Previously found significantly decreasing long-term bowel scores (> 5 points) after conformal RT to doses of 70.2-72Gy could be avoided after IMRT without and with SIB in spite of increasingly higher total doses to the prostate and specifically the intraprostatic malignant lesion.
The results are encouraging to continue evaluating this concept in the future. Further results with longer follow-up and larger patient groups are needed.
References
Viani GA, Stefano EJ, Alfonso SL: Higher-than-conventional radiation doses in localized prostate cancer treatment: a meta-analysis of randomized, controlled trials. Int J Radiat Oncol Biol Phys. 2009, 74: 1405-1418. 10.1016/j.ijrobp.2008.10.091.
Pinkawa M, Piroth MD, Fischedick K, Nussen S, Klotz J, Holy R, Eble MJ: Self-assessed bowel toxicity after external beam radiotherapy for prostate cancer--predictive factors on irritative symptoms, incontinence and rectal bleeding. Radiat Oncol. 2009, 4: 36-10.1186/1748-717X-4-36.
Pinkawa M, Holy R, Piroth MD, Fischedick K, Schaar S, Székely-Orbànm Eble MJ: Consequential late effets after radiotherapy for prostate cancer - a prospective longitudianl quality of life study. Radiat Oncol. 2010, 5: 27-10.1186/1748-717X-5-27.
Cellini N, Morganti AG, Mattiucci GC, Valentini V, Leone M, Luzi S, Manfredi R, Dinapoli N, Digesu C, Smaniotto D: Analysis of intraprostatic failures in patients treated with hormonal therapy and radiotherapy: implications for conformal therapy planning. Int J Radiat Oncol Biol Phys. 2002, 53: 595-599. 10.1016/S0360-3016(02)02795-5.
Chen ME, Johnston DA, Tang K, Babaian RJ, Troncoso P: Detailed mapping of prostate carcinoma foci: biopsy strategy implications. Cancer. 2000, 89: 1800-1809. 10.1002/1097-0142(20001015)89:8<1800::AID-CNCR21>3.0.CO;2-D.
Farsad M, Schiavina R, Castellucci P, Nanni C, Corti B, Martorana G, Canini R, Grigioni W, Boschi S, Marengo M, Pettinato C, Salizzoni E, Monetti N, Franchi R, Fanti S: Detection and localization of prostate cancer: correlation of (11)C-choline PET/CT with histopathologic step-section analysis. J Nucl Med. 2005, 46: 1642-1649.
Kwee SA, Wei H, Sesterhenn I, Yun D, Coel MN: Localization of primary prostate cancer with dual-phase 18F-fluorocholine PET. J Nucl Med. 2006, 47: 262-269.
Pinkawa M, Attieh C, Piroth MD, Holy R, Nussen S, Klotz J, Hawickhorst R, Schäfer W, Eble MJ: Dose-escalation using intensity-modulated radiotherapy for prostate cancer--evaluation of the dose distribution with and without 18F-choline PET-CT detected simultaneous integrated boost. Radiother Oncol. 2009, 93: 213-219. 10.1016/j.radonc.2009.07.014.
Pinkawa M, Pursch-Lee M, Asadpour B, Gagel B, Piroth MD, Klotz J, Nussen S, Eble MJ: Image-guided radiotherapy for prostate cancer. Implementation of ultrasound-based prostate localization for the analysis of inter- and intrafraction motion. Strahlenther Onkol. 2008, 184: 679-685. 10.1007/s00066-008-1902-7.
Burman C, Kutcher GJ, Emami B, Goitein M: Fitting of normal tissue tolerance data to an analytic function. Int J Radiat Oncol Biol Phys. 1991, 21: 123-135.
Emami B, Lyman JT, Brown A, Coia L, Goitein M, Munzenrider JE, Shank B, Solin LJ, Wesson M: Tolerance of normal tissue to therapeutic irradiation. Int J Radiat Oncol Biol Phys. 1991, 21: 109-122.
Wei JT, Dunn RL, Litwin MS, Sandler HM, Sanda MG: Development and validation of the expanded prostate cancer index composite (epic) for comprehensive assessment of health-related quality of life in men with prostate cancer. Urology. 2000, 56: 899-905. 10.1016/S0090-4295(00)00858-X.
Volz-Sidiropoulou E, Pinkawa M, Fischedick K, Jakse G, Gauggel S, Eble MJ: Factor analysis of the Expanded Prostate Cancer Index Composite (EPIC) in a patient group after primary (external beam radiotherapy and permanent iodine-125 brachytherapy) and postoperative radiotherapy for prostate cancer. Curr Urol. 2008, 2: 122-129. 10.1159/000189652.
Pinkawa M, Holy R, Piroth DM, Klotz J, Pfister D, Heidenreich A, Eble MJ: Interpreting the clinical significance of quality of life score changes after radiotherapy for localized prostate cancer. Curr Urol. 2011, 5: 137-144. 10.1159/000327467.
Pinkawa M, Eble MJ, Mottaghy FM: PET and PET/CT in radiation treatment planning for prostate cancer. Expert Rev Anticancer Ther. 2011, 7: 1035-1041.
Fonteyne V, Villeirs G, Speleers B, De Neve W, De Wagter C, Lumen N, De Meerleer G: Intensity-modulated radiotherapy as primary therapy for prostate cancer: report on acute toxicity after dose escalation with simultaneous integrated boost to intraprostatic lesion. Int J Radiat Oncol Biol Phys. 2008, 72: 799-807. 10.1016/j.ijrobp.2008.01.040.
Rinnab L, Mottaghy FM, Blumstein NM, Resje SN, Hautmann RE, Hohl K, Möller P, Wiegel T, Kuefer R, Gschwend JE: Evaluation of [11C]-choline positron-emission/computed tomography in patients with increasing prostate-specific antigen levels after primary treatment for prostate cancer. BJU Int. 2007, 100: 786-93. 10.1111/j.1464-410X.2007.07083.x.
Emonds KM, Swinnen JV, Mortelmanns L, Mottaghy FM: Molecular imaging of prostate cancer. Methods. 2009, 48: 193-199. 10.1016/j.ymeth.2009.03.021.
Wang J, Bai S, Chen N, Xu F, Jiang X, Li Y, Xu Q, Shen Y, Zhang H, Gong Y, Zhong R, Jiang Q: The clinical feasibility of online cone beam computer tomography-guided intensity-modulated radiotherapy for nasopharyngeal cancer. Radiother Oncol. 2009, 90: 221-227. 10.1016/j.radonc.2008.08.017.
Bartelink H, Horiot JC, Poortmans PM, Struikmans H, Van den Bogaert W, Fourquet A, Jager JJ, Hoogenraad WJ, Oei SB, Wárlám-Rodenhuis CC, Pierart M, Collette L: Impact of higher radiation dose on local control and survival after breast-conserving therapy of early breast cancer: 10-year results of the randomized boost versus no boost EORTC 22881-10882 trial. J Clin Oncol. 2007, 25: 3259-3265. 10.1200/JCO.2007.11.4991.
Pinkawa M, Holy R, Piroth DM, Klotz J, Nussen S, Krohn T, Mottaghy FM, Weibrecht M, Eble MJ: Intensity-modulated radiotherapy for prostate cancer implementing molecular imaging with 18F-choline PET-CT to define a simultaneous integrated boost. Strahlenther Onkol. 2011, 186: 600-606.
Sutinen E, Nurmi M, Roivainen A, Roivainen A, Varpula M, Tolvanen T, Lehikoinen P, Minn H: Kinetics of [(11)C]choline uptake in prostate cancer: a PET study. Eur J Nucl Med Mol Imaging. 2004, 31: 317-324. 10.1007/s00259-003-1377-9.
Piert M, Park H, Khan A, Siddiqui J, Hussain H, Chenevert T, Wood D, Johnson T, Shah RB, Meyer C: Detection of aggressive primary prostate cancer with 11C-choline PET/CT using multimodality fusion techniques. J Nucl Med. 2009, 50: 1585-1593. 10.2967/jnumed.109.063396.
De Meerleer G, Villeirs G, Bral S, Paelinck L, De Gersem W, Dekuyper P, De Neve W: The magnetic resonance detected intraprostatic lesion in prostate cancer: planning and delivery of intensity-modulated radiotherapy. Radiother Oncol. 2005, 75: 325-333. 10.1016/j.radonc.2005.04.014.
Acknowledgements
The study was funded by the research resources of the Department of Radiation Oncology, RWTH Aachen University, Germany. The implementation of 18F-choline PET-CT was supported by Philips Research.
We would like to thank the staff who took care of our patients' needs, and who were involved in gathering, documenting, verifying, forwarding, and processing the clinical data.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
MP, MJE have made substantial contributions to conception and design; MP, MDP, RH, JK, VD, NEC, MC, OW, TK, FMM, MJE have made substantial contributions to acquisition of data; MP, MDP, RH, MJE to analysis and interpretation of data. MP has been involved in drafting the manuscript. MDP, RH, JK, VD, NEC, MC, OW, TK, FMM, MJE revised it critically for important intellectual content. All authors have given final approval of the version to be published.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Pinkawa, M., Piroth, M.D., Holy, R. et al. Dose-escalation using intensity-modulated radiotherapy for prostate cancer - evaluation of quality of life with and without 18F-choline PET-CT detected simultaneous integrated boost. Radiat Oncol 7, 14 (2012). https://doi.org/10.1186/1748-717X-7-14
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1748-717X-7-14