Abstract
As part of the AIRC IG-13218 (NCT01913717), we analyzed data from patients with low- and intermediate-risk prostate cancer treated with extreme hypofractionated radiotherapy (RT) and simultaneous boost to the intraprostatic lesion. The aim of the study is to identify clinically meaningful information through the analysis of validated questionnaires testing gastrointestinal (GI) and genitourinary (GU) RT-related toxicity and their impact on quality of life (QoL). At the end of RT treatment, clinical assessment and prostate-specific antigen (PSA) measurements were performed every 3 months for at least 2 years and GI and GU toxicities were evaluated contextually. QoL of enrolled patients was assessed by International Prostate Symptoms score (IPSS), European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire—Core 30 (EORTC QLQ-C30), EORTC QLQ prostate specific (QLQ-PR25), and sexual activity by International Index of Erectile Function (IIEF-5). Patients’ score changes were calculated at the end of RT, at one month after RT and at 12 and 24 months. Sixty-five prospectively enrolled patients were analyzed. Extensive analysis of different QoL assessments showed that patients’ tolerance was satisfactory across all the considered time points, with no statistically significant change of QoL from baseline compared to that before RT. Overall survival and biochemical progression-free survival at 2-years were of 98% and 97%, respectively. Despite the toxicity of extreme hypofractionation was low and tumor control was encouraging, a longer follow-up is necessary to confirm our findings. The increasing dose to the dominant intraprostatic lesion does not worsen the RT toxicity and consequently does not affect patients’ QoL, thus questioning the possibility of an even more escalated treatment.





Similar content being viewed by others
Abbreviations
- AIRC:
-
Associazione Italiana per la Ricerca sul Cancro
- b-PFS:
-
Biochemical progression-free survival
- CT:
-
Computed tomography
- CTV:
-
Clinical target volume
- DIL:
-
Dominant intraprostatic lesion
- EORTC:
-
European Organization for Research and Treatment of Cancer
- G:
-
Grade
- GEE:
-
Generalized estimation method
- GI:
-
Gastrointestinal
- GU:
-
Genitourinary
- IEO:
-
European Institute of Oncology IRCCS
- IGRT:
-
Image-guided radiation therapy
- IIEF-5:
-
International index of erectile function
- IMRT:
-
Intensity-modulated radiotherapy
- IPSS:
-
International prostatic symptoms score
- IQR:
-
Interquartile range
- MAR:
-
Missing at random
- mpMRI:
-
Multiparametric resonance imaging
- NCCN:
-
National comprehensive cancer network
- OAR:
-
Organ at risk
- OS:
-
Overall survival
- PCa:
-
Prostate cancer
- PET:
-
Positron emission tomography
- PRO:
-
Patient-reported outcome
- PSA:
-
Prostate-specific antigen
- PTV:
-
Planning target volume
- QLQ-C30:
-
Quality life questionnaire-core 30
- QLQ-PR25:
-
Quality life questionnaire prostate specific
- QoL:
-
Quality of life
- RT:
-
Radiotherapy
- RTOG:
-
Radiation Therapy Oncology Group
- SBRT:
-
Stereotactic body radiotherapy
- SIB:
-
Simultaneous integrated boost
References
Hamdy FC, Donovan JL, Lane JA, et al. 10-year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N Engl J Med. 2016;375:1415–24. https://doi.org/10.1056/NEJMoa1606220.
Lane JA, Donovan JL, Davis M, et al. Active monitoring, radical prostatectomy, or radiotherapy for localised prostate cancer: study design and diagnostic and baseline results of the ProtecT randomised phase 3 trial. Lancet Oncol. 2014;15:1109–18. https://doi.org/10.1016/S1470-2045(14)70361-4.
Miralbell R, Roberts SA, Zubizarreta E, Hendry JH. Dose-fractionation sensitivity of prostate cancer deduced from radiotherapy outcomes of 5,969 patients in seven international institutional datasets: α/β = 1.4 (0.9–2.2) Gy. Int J Radiat Oncol Biol Phys. 2012;82:e17–24. https://doi.org/10.1016/j.ijrobp.2010.10.075.
Catton CN, Lukka H, Gu C-S, et al. Randomized trial of a hypofractionated radiation regimen for the treatment of localized prostate cancer. J Clin Oncol Off J Am Soc Clin Oncol. 2017;35:1884–900. https://doi.org/10.1200/JCO.2016.71.7397.
Dearnaley D, Syndikus I, Mossop H, et al. Conventional versus hypofractionated high-dose intensity-modulated radiotherapy for prostate cancer: 5-year outcomes of the randomised, non-inferiority, phase 3 CHHiP trial. Lancet Oncol. 2016;17:1047–60. https://doi.org/10.1016/S1470-2045(16)30102-4.
Lee WR, Dignam JJ, Amin MB, et al. Randomized phase III noninferiority study comparing two radiotherapy fractionation schedules in patients with low-risk prostate cancer. J Clin Oncol. 2016;34:2325–32. https://doi.org/10.1200/JCO.2016.67.0448.
Boike TP, Lotan Y, Cho LC, et al. Phase I dose-escalation study of stereotactic body radiation therapy for low- and intermediate-risk prostate cancer. J Clin Oncol Off J Am Soc Clin Oncol. 2011;29:2020–6. https://doi.org/10.1200/JCO.2010.31.4377.
Hannan R, Tumati V, Xie X-J, et al. Stereotactic body radiation therapy for low and intermediate risk prostate cancer-results from a multi-institutional clinical trial. Eur J Cancer Oxf Engl. 1990;2016(59):142–51. https://doi.org/10.1016/j.ejca.2016.02.014.
King CR, Brooks JD, Gill H, Presti JC. Long-term outcomes from a prospective trial of stereotactic body radiotherapy for low-risk prostate cancer. Int J Radiat Oncol Biol Phys. 2012;82:877–82. https://doi.org/10.1016/j.ijrobp.2010.11.054.
Fonteyne V, Soete G, Arcangeli S, et al. Hypofractionated high-dose radiation therapy for prostate cancer: long-term results of a multi-institutional phase II trial. Int J Radiat Oncol. 2012;84:e483–e490490. https://doi.org/10.1016/j.ijrobp.2012.04.012.
Jackson WC, Silva J, Hartman HE, et al. Stereotactic body radiotherapy for localized prostate cancer: a systematic review and meta-analysis of over 6,000 patients treated on prospective studies. Int J Radiat Oncol Biol Phys. 2019;104(4):778–89. https://doi.org/10.1016/j.ijrobp.2019.03.051.
Royce TJ, Lee DH, Keum N, et al. Conventional versus hypofractionated radiation therapy for localized prostate cancer: a meta-analysis of randomized noninferiority trials. Eur Urol Focus. 2019;5(4):577–84. https://doi.org/10.1016/j.euf.2017.10.011.
Incrocci L, Wortel RC, Alemayehu WG, et al. Hypofractionated versus conventionally fractionated radiotherapy for patients with localised prostate cancer (HYPRO): final efficacy results from a randomised, multicentre, open-label, phase 3 trial. Lancet Oncol. 2016;17:1061–9. https://doi.org/10.1016/S1470-2045(16)30070-5.
Arcangeli G, Saracino B, Arcangeli S, et al. Moderate hypofractionation in high-risk, organ-confined prostate cancer: final results of a phase III randomized trial. J Clin Oncol Off J Am Soc Clin Oncol. 2017;35:1891–7. https://doi.org/10.1200/JCO.2016.70.4189.
Wilkins A, Mossop H, Syndikus I, et al. Hypofractionated radiotherapy versus conventionally fractionated radiotherapy for patients with intermediate-risk localised prostate cancer: 2-year patient-reported outcomes of the randomised, non-inferiority, phase 3 CHHiP trial. Lancet Oncol. 2015;16:1605–16. https://doi.org/10.1016/S1470-2045(15)00280-6.
Widmark A, Gunnlaugsson A, Beckman L, et al. Extreme hypofractionation versus conventionally fractionated radiotherapy for intermediate risk prostate cancer: early toxicity results from the scandinavian randomized phase III trial “HYPO-RT-PC”. Int J Radiat Oncol. 2016;96:938–9. https://doi.org/10.1016/j.ijrobp.2016.09.049.
De Bari B, Arcangeli S, Ciardo D, et al. Extreme hypofractionation for early prostate cancer: Biology meets technology. Cancer Treat Rev. 2016;50:48–60. https://doi.org/10.1016/j.ctrv.2016.08.005.
Tambas M, Agaoglu F, Iribas A, et al. Conventionally Fractionationed volumetric arc therapy versus hypofractionated stereotactic body radiotherapy: quality of life, side effects, and prostate-specific antigen kinetics in localized prostate cancer. Value Health Reg Issues. 2016;10:91–9. https://doi.org/10.1016/j.vhri.2016.08.001.
Lukka HR, Pugh SL, Bruner DW, et al. Patient reported outcomes in NRG oncology RTOG 0938, evaluating two ultrahypofractionated regimens for prostate cancer. Int J Radiat Oncol Biol Phys. 2018;102:287–95. https://doi.org/10.1016/j.ijrobp.2018.06.008.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)- Prostate Cancer. Version 2.2019-April 17, 2019 n.d.
Feutren T, Herrera FG. Prostate irradiation with focal dose escalation to the intraprostatic dominant nodule: a systematic review. Prostate Int. 2018;6(3):75–877. https://doi.org/10.1016/j.prnil.2018.03.005.
Lips IM, van der Heide UA, Haustermans K, et al. Single blind randomized phase III trial to investigate the benefit of a focal lesion ablative microboost in prostate cancer (FLAME-trial): study protocol for a randomized controlled trial. Trials. 2011;12(1):255.
Basch E, Deal AM, Dueck AC, et al. Overall survival results of a trial assessing patient-reported outcomes for symptom. JAMA. 2017;318:197–8.
Forgione M, Sara S, Vincent AD, Borg M, Moretti K, O’Callaghan ME. Satisfaction with care in men with prostate cancer. Eur J Cancer Care. 2019. https://doi.org/10.1111/ecc.13028.
Diefenbach MA, Mohamed NE. Regret of treatment decision and its association with disease-specific quality of life following prostate cancer treatment. Cancer Invest. 2007;25:449–57. https://doi.org/10.1080/07357900701359460.
Fervaha G, Izard JP, Tripp DA, Rajan S, Leong DP, Siemens DR. Depression and prostate cancer: a focused review for the clinician. Urol Oncol. 2019;37:282–8. https://doi.org/10.1016/j.urolonc.2018.12.020.
Rammant E, Ost P, Swimberghe M, et al. Patient- versus physician-reported outcomes in prostate cancer patients receiving hypofractionated radiotherapy within a randomized controlled trial. Strahlenther Onkol Organ Dtsch Rontgengesellschaft Al. 2019;195:393–401. https://doi.org/10.1007/s00066-018-1395-y.
Di Maio M, Gallo C, Leighl NB, et al. Symptomatic toxicities experienced during anticancer treatment: agreement between patient and physician reporting in three randomized trials. J Clin Oncol Off J Am Soc Clin Oncol. 2015;33:910–5. https://doi.org/10.1200/JCO.2014.57.9334.
Timon G, Ciardo D, Bazani A, et al. Rationale and protocol of AIRC IG-13218, short-term radiotherapy for early prostate cancer with concomitant boost to the dominant lesion. Tumori. 2016;102(5):536–40.
Timon G, Ciardo D, Bazani A, et al. Short-term high precision radiotherapy for early prostate cancer with concomitant boost to the dominant lesion: ad interim analysis and preliminary results of phase II trial AIRC-IG-13218. Br J Radiol. 2018;91(1089):20160725.
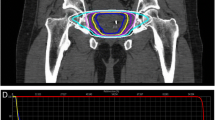
Mambretti M, Romanò C, Marvaso G, et al. A global Unified Dosimetry Index (gUDI) to evaluate simultaneous integrated boost radiotherapy plans in prostate cancer. Radiother Oncol. 2018;128(2):315–20.
Ciardo D, Jereczek-Fossa BA, Petralia G, et al. Multimodal image registration for the identification of dominant intraprostatic lesion in high-precision radiotherapy treatments. Br J Radiol. 2017;90:20170021.
Cox JD, Stetz J, Pajak TF. Toxicity criteria of the radiation therapy oncology group (RTOG) and the European organization for research and treatment of cancer (EORTC). Int J Radiat Oncol. 1995;31(5):1341–6.
Monninkhof EM, van Loon JWL, van Vulpen M, et al. Standard whole prostate gland radiotherapy with and without lesion boost in prostate cancer: toxicity in the FLAME randomized controlled trial. Radiother Oncol. 2018;127(1):74–80. https://doi.org/10.1016/j.radonc.2017.12.022.
Brand DH, Tree AC, Ostler P, et al. Intensity-modulated fractionated radiotherapy versus stereotactic body radiotherapy for prostate cancer (PACE-B): acute toxicity findings from an international, randomised, open-label, phase 3, non-inferiority trial. Lancet Oncol. 2019;20:1531–43.
Widmark A, Gunnlaugsson A, Beckman L, et al. Ultra-hypofractionated versus conventionally fractionated radiotherapy for prostate cancer: 5-year outcomes of the HYPO-RT-PC randomised, non-inferiority, phase 3 trial. Lancet. 2019;394(10196):385–95. https://doi.org/10.1016/S0140-6736(19)31131-6.
Broughman JR, Basak R, Nielsen ME, et al. Prostate cancer patient characteristics associated with a strong preference to preserve sexual function and receipt of active surveillance. JNCI. 2017;110(4):420–5.
Carroll PR, Hoffman RM, Hunt WC, Gilliland FD, Stephenson RA, Potosky AL. Patient satisfaction with treatment decisions for clinically localized prostate carcinoma. Results from the Prostate Cancer Outcomes Study. Cancer. 2003;97:1653–62.
Hyun JS. Prostate cancer and sexual function. World J Men's Health. 2012;30(2):99–107.
Pasquier D, Peiffert D, Nickers P, et al. A multicentre phase II study of hypofractionated stereostatic boost in intermediate risk prostate carcinoma: a 5-year analysis of the CKNO-PRO trial. PLoS ONE. 2017;12(11):e0187794. https://doi.org/10.1371/journal.pone.0187794.
Wortel RC, Oomen-de Hoop E, Heemsbergen WD, Pos FJ, Incrocci L. Moderate hypofractionation in intermediate-and high-risk, localized prostate cancer: health-related quality of life from the randomized, phase 3 HYPRO trial. Int J Radiat Oncol. 2019;103(4):823–33.
Alongi F, Mazzola R, Fiorentino A, et al. Phase II study of accelerated Linac-based SBRT in five consecutive fractions for localized prostate cancer. Phase-II-Studie zur Linac-basierten akzelerierten SBRT in fünf konsekutiven Fraktionen bei lokal begrenztem Prostatakarzinom. Strahlenther Onkol. 2019;195(2):113–20. https://doi.org/10.1007/s00066-018-1338-7.
van Stam MA, Aaronson NK, Bosch JR, et al. Patient-reported outcomes following treatment of localised prostate cancer and their association with regret about treatment choices. Eur Urol Oncol. 2020;3(1):21–31. https://doi.org/10.1016/j.euo.2018.12.004.
Adam S, Koch-Gallenkamp L, Bertram H, et al. Health-related quality of life in long-term survivors with localised prostate cancer by therapy—results from a population-based study. Eur J Cancer Care. 2019;28(5):e13076. https://doi.org/10.1111/ecc.13076.
Alongi F, Rigo M, Figlia V, et al. 1.5 T MR-guided and daily adapted SBRT for prostate cancer: feasibility, preliminary clinical tolerability, quality of life and patient-reported outcomes during treatment. Radiat Oncol. 2020;15(1):69.
Katz AJ, Kang J. Quality of life and toxicity after SBRT for organ-confined prostate cancer, a 7-year study. Front Oncol. 2014;4:301.
Acknowledgements
SGG was partially Supported by Associazione Italiana per la Ricerca sul Cancro (AIRC), by Project IG-14300 “Carbon ions boost followed by pelvic photon intensity-modulated radiotherapy for high-risk prostate cancer,” registered at ClinicalTrials.gov (NCT02672449). The study was also supported by Project IG-13218 “Short-term High Precision Radiotherapy for Early Prostate Cancer With Concomitant Boost on the Dominant Lesion,” registered at ClinicalTrials.gov (NCT01913717). The sponsors did not play any role in the study design, collection, analysis, and interpretation of data, nor in the writing of the manuscript, nor in the decision to submit the manuscript for publication.
Funding
None.
Author information
Authors and Affiliations
Contributions
GM and BAJF were responsible for the study conception and design and had final responsibility for the decision to submit the manuscript for publication. GM, SGG, FB, and SG drafted the manuscript. GM, GC, SV, DPR, GR, DZ, CIF, ELR, PP, SA, GP, FAM, RC, and FC were responsible for acquisition and analysis of data. GM, SGG, FB, SG, and BAJF were responsible for interpretation of data. MP, ODC, RO, and BAJF substantially revised the work. All authors have read and approved the final version of the manuscript and have agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they do not have any conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. In this research, no animals were involved.
Informed consent
All patients signed a written informed consent for radiation therapy and written informed consent for the use of the anonymized data for research or educational purpose. The present study has been reviewed and approved by the Internal Review Board of the Division of Radiotherapy, IEO, European Institute of Oncology IRCCS, Via Ripamonti 435, 20141, Milan, Italy.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Marvaso, G., Gugliandolo, S.G., Bellerba, F. et al. Phase II prospective trial “Give Me Five” short-term high precision radiotherapy for early prostate cancer with simultaneous boost to the dominant intraprostatic lesion: the impact of toxicity on quality of life (AIRC IG-13218). Med Oncol 37, 74 (2020). https://doi.org/10.1007/s12032-020-01397-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-020-01397-3