Abstract
Background
The most common bariatric surgery, Roux-en-Y gastric bypass, leads to glycemia normalization in most patients long before there is any appreciable weight loss. This effect is too large to be attributed purely to caloric restriction, so a number of other mechanisms have been proposed. The most popular hypothesis is enhanced production of an incretin, active glucagon-like peptide-1 (GLP-1), in the lower intestine. We therefore set out to test this hypothesis with a model which is simple enough to be robust and credible.
Method
Our method involves (1) setting up a set of time-dependent equations for the concentrations of the most relevant species, (2) considering an “adiabatic” (or quasi-equilibrium) state in which the concentrations are slowly varying compared to reaction rates (and which in the present case is a postprandial state), and (3) solving for the dependent concentrations (of e.g. insulin and glucose) as an independent concentration (of e.g. GLP-1) is varied.
Results
Even in the most favorable scenario, with maximal values for (i) the increase in active GLP-1 concentration and (ii) the effect of GLP-1 on insulin production, enhancement of GLP-1 alone cannot account for the observations. I.e., the largest possible decrease in glucose predicted by the model is smaller than reported decreases, and the model predicts no decrease whatsoever in glucose ×insulin, in contrast to large observed decreases in homeostatic model assessment insulin resistance (HOMA-IR). On the other hand, both effects can be accounted for if the surgery leads to a substantial increase in some substance that opens an alternative insulin-independent pathway for glucose transport into muscle cells, which perhaps uses the same intracellular pool of GLUT-4 that is employed in an established insulin-independent pathway stimulated by muscle contraction during exercise.
Conclusions
Glycemia normalization following Roux-en-Y gastric bypass is undoubtedly caused by a variety of mechanisms, which may include caloric restriction, enhanced GLP-1, and perhaps others proposed in earlier papers on this subject. However, the present results suggest that another possible mechanism should be added to the list of candidates: enhanced production in the lower intestine of a substance which opens an alternative insulin-independent pathway for glucose transport.
Similar content being viewed by others
Background
Type 2 diabetes
Type 2 diabetes (T2D) has reached epidemic proportions worldwide. In 2011, an estimated 366 million people had diabetes, and this number is predicted to rise to 522 million by 2030[1]. The medical and socioeconomic burdens of the disease and the strains imposed on health-care systems arise from the devastating associated macro- and micro-vascular complications such as nephropathy, hypertension, retinopathy, cardiovascular diseases, and amputations, which make diabetes a major cause of both morbidity and mortality. Cardiovascular morbidity, for example, is 2 to 4 times greater in patients with T2D than in non-diabetic people[2].
T2D develops in adulthood and is generally considered to be a condition marked by insulin resistance and loss of function of insulin-secreting pancreatic beta cells. The exact etiology of T2D remains largely unknown. So far, over 60 genes have been associated with an increased risk for T2D[3]. However, even when pooled, these genes only account for 5-10% of disease risk[4]. Currently, it is widely recognized that obesity is the major independent risk factor for the development of T2D, and that the rise in T2D prevalence worldwide is driven by an increasing frequency of obesity, which, in turn, is driven by a combination of genetic predisposition and interactions with obesogenic environments including high intake of energy-dense food and physical inactivity[5]. Obesity-associated T2D development (diabesity) is due to the excess fat that affects many organs that are involved in glucose homeostasis, including liver and pancreas.
There is a general consensus today that T2D is a lifetime disease and that a medical cure for patients suffering from T2D does not exist. Current medical management of T2D leaves much to be desired, requiring constant vigilance from both patients and physicians. At best, the available medications, when combined with diet and physical activity, are targeted to lower blood glucose and decrease the peripheral insulin resistance associated with T2D. However, medical treatment has had limited success maintaining safe blood glucose levels in patients, as evidenced, for example, by high numbers of diabetic amputations and new onset blindness[6, 7]. With minimal success of medical treatment, there is an urgent need for a more permanent cure for the disease that has debilitated so many patients. Currently the only hope for a T2D “cure” (or at least long term remission) is bariatric surgery in very obese patients, which has opened new horizons for understanding the pathophysiology of T2D, and perhaps also hope for new therapies.
Bariatric surgery
Also called metabolic surgery, this is a form of gastrointestinal surgery that aims at reducing the amount of food intake and/or the absorption of nutrients at the intestinal level. It is, to date, the most successful intervention for the treatment of obesity. In most cases, bariatric surgery achieves a significant and sustained weight loss ranging from 12% to 39% of presurgical body weight or 40-71% excess weight loss (EWL)[8, 9].
There exist a dozen bariatric surgery procedures, which fall into the following categories: (i) Restrictive procedure: the aim is to limit the amount of food intake by reducing the size of the stomach. (ii) Malabsorptive procedure: the aim is to limit the absorption of food in the intestinal tract by bypassing a portion of the small intestine to varying degrees. (iii) Combination of both restriction and malabsorption. The four standard bariatric surgery procedures that are currently accepted for weight loss in obese patients are: (1) adjustable gastric banding (AGB), which is solely restrictive; (2) Roux-en-Y gastric bypass (RYGB), which has both restrictive and malabsorptive components; (3) sleeve gastrectomy, which is another solely restrictive procedure used for treatment of morbid obesity; (4) biliopancreatic diversion with duodenal switch (BPDDS), which is a more radical restrictive and malabsorptive procedure[10, 11]. Among the four currently accepted procedures, Roux-en-Y gastric bypass (RYGB), where the majority of the stomach and duodenum are bypassed because the stomach is reduced to a small proximal pouch and is then anastomosed to the jejunum[12], and laparoscopic adjustable gastric banding (LAGB), where the stomach is reduced to a small pouch by encircling the upper part of the stomach with a band-like fluid-filled tube, are the most frequently performed worldwide. Sleeve gastrectomy, where the stomach is reduced by 85% by excising the greater curvature and reconstructing a tubularized stomach conduit, is gaining popularity and is widely used for severely obese patients who are high-risk surgery candidates[13].
Bariatric surgery was initially used to induce weight loss in morbidly obese patients. However, it turned out that it also results in an improvement in many obesity related comorbidities including T2D[14]. Today, although curing diabetes cannot yet be considered a goal of bariatric surgery, it may be considered a serendipitous benefit.
Bariatric surgery induces long-term remission of type 2 diabetes
The last two decades have witnessed the emergence of bariatric surgery as a powerful intervention that, in addition to inducing the drastic and sustained weight loss for which it was initially designed, leads to long-term remission of T2D, decreasing the progression and potentially reversing the effects of diabetes in 40-80% of morbidly obese patients (BMI > 40 kg/m2, or BMI > 35 kg/m2 with comorbidities)[15–20]. The first report showing a serendipitous improvement or remission of hyperglycemia after gastrectomy was published in the 1950s[21]. However, it was in 1995 that Walter Pories and his colleagues described in a seminal paper a sustained improvement in glycemia control for up to 14 years after gastric bypass surgery in morbidly obese patients with T2D[22]. This astonishingly beneficial effect of bariatric surgery on glucose homeostasis was confirmed by numerous subsequent studies in both humans and animal models[16, 18].
It is well documented that weight loss, whatever the means used, improves glycemic control in obese or overweight diabetics, and it is therefore easy to attribute the remarkable return to euglycemia after bariatric surgery to weight loss. However, while weight loss certainly plays a major role in inducing improved glucose homeostasis after metabolic surgery, the striking glycemia normalization after bariatric surgery, as reported by many investigators, is achieved within a few days post-operation, long before any significant weight loss has taken place[22], and many obese diabetic patients are able to decrease, or discontinue, insulin and oral hypoglycemics just days after undergoing surgery[23]. Moreover, there is evidence that even non-obese patients with T2D[24–27] and animal models[28] experience similar anti-diabetic effects without significant weight loss.
This rapid time course and disproportional degree of T2D cure, or at least long-term remission, strongly suggests that resolution of T2D is driven by mechanisms that are surgery-specific and independent of weight loss. Given the immense positive consequences that resolution of T2D will have on the patients’ quality of life and on the diabetes-related expenditure for the patients and for the health-care systems[29], interest in the mechanisms that underlie the remission of T2D has spurred huge interest from the scientific community during the last decade. In fact, understanding the effects of bariatric surgery on T2D would provide important insights into the pathogenesis of type 2 diabetes and allow the development of new procedures, devices, and drugs both for obese and non-obese patients. It is hoped that pharmaceutical mimetics of the underlying mechanisms would potentially offer powerful new medicines for the treatment of T2D without invasive and risky surgery.
Mechanisms underlying immediate and long-term remission
Despite immense efforts worldwide, the mechanisms behind the glycemic normalization after metabolic surgery remain elusive. It was initially thought that the observed remission of T2D is the obvious result of weight loss, as significant weight loss improves insulin resistance and contributes to diabetes management. However, this hypothesis is challenged by the very rapid adjustment of glycemia reported in many studies, long before any significant weight loss is achieved. Moreover, the positive effect of surgery on glucose tolerance exceeds that achieved after equivalent weight loss via diet and exercise[30] or after conventional medical therapy[18]. Several plausible hypotheses can be articulated to explain the rapid, weight-independent glycemic effects of bariatric surgery, and none of them necessarily precludes the others. In fact, it is likely that the beneficial effect is the result of the involvement of multiple pathways that involve signals to and from different metabolism-related organs including the brain, adipose tissue, pancreas, gastrointestinal tract, liver, kidney, skeletal muscle, and perhaps others. The main suggested hypotheses are listed below. Since there is a vast literature on the effects of bariatric surgery, it should be emphasized that the papers cited here are primarily a representative sample from published work that features the very short-term effects of one specific procedure, namely RYGB.
Caloric restriction hypothesis
According to this hypothesis, the remission of T2D after metabolic surgery is due to postoperative caloric restriction. The ability of acute caloric restriction to transiently improve T2D is well known[31, 32]. (See, e.g., Figure three of Ref.[32] for 3-7 days of very low calorie dieting.) According to this model, by the time the patients are allowed ad libitum eating, they begin to experience the insulin-sensitizing effects of dynamic weight loss from the surgery. Though prima facie reasonable, this hypothesis fails to explain why the remission of T2D is far faster after RYGB than AGB, while they both involve perioperative food restriction followed by progressive weight loss[33, 34]. This hypothesis also does not explain the superiority of the glycemic control achieved after RYGB versus equivalent weight loss from dieting[10, 35].
In general, it appears that extreme caloric restriction (complete fasting or ≤300 kcal per day) can result in strong short-term decreases in plasma glucose and insulin, but that the typical dietary restrictions following RYGB surgery are not sufficient to explain the remarkable improvements that are widely observed.
Malabsorption hypothesis
As mentioned above, RYGB has both restrictive and malabsorptive effects, both of which are thought to be significant in achieving long-term weight loss. However, a recent study[36] of patients undergoing long-limb RYGB found that “malabsorption accounted for ≈6% and 11% of the total reduction in combustible energy absorption at 5 and 14 mo, respectively, after this gastric bypass procedure.” In other words, malabsorptive effects are much smaller than caloric restriction effects, and are again insufficent to account for the immediate improvement in glucose levels and insulin sensitivity.
Ghrelin hypothesis
Ghrelin is a circulating hormone produced predominantly (90%) by P/D1 cells lining the fundus of the human stomach. It is also produced in small amounts from the pancreas, the intestine, the placenta, the kidney, the pituitary gland, and the hypothalamus. It is an orexigenic hormone that stimulates appetite and food intake. Thus, ghrelin levels increase before meals to signal hunger to the brain, specifically areas of the hypothalamic feeding centers, which express the ghrelin receptors. The latter are also expressed by the insulin-secreting pancreatic beta cells, a key player in glucose metabolism[37]. In addition to its effects on feeding behavior, ghrelin has been implicated in the regulation of glucose homeostasis[38, 39]. Thus, the increase of circulating levels of ghrelin by exogenous infusion of the hormone in humans results in a reduction of glucose-induced insulin secretion and therefore glucose disposal[37]. Though the molecular mechanisms by which ghrelin suppresses insulin secretion are not yet well understood, this observation suggests that lower levels of ghrelin may improve the beta cell function.
According to the ghrelin hypothesis, the regulation of ghrelin may be altered by bariatric surgery, and there are indeed studies showing that preprandial ghrelin levels are very low after bariatric surgery. Cummings et al. were the first to report reduced levels of ghrelin post-RYGB compared to pre-RYGB[40], and many subsequent studies have confirmed this observation[41–43]. However, this hypothesis is still very equivocal, as other studies have reported an increase of postprandial ghrelin levels after RYGB, while yet others have reported no change between pre- and post-RYGB[13, 19, 44]. Different methodologies and study designs might explain these discrepancies, and more investigations are required to fully understand the role of ghrelin in T2D remission after bariatric surgery. Diminished ghrelin secretion would also decrease appetite and food intake, leading to weight loss on a longer time scale than that which is relevant in the present context.
Lower intestinal hypothesis
This hypothesis, also called the hindgut hypothesis, is proposed to explain the rapid T2D remission after RYGB and BPD via effects that result from the expedited delivery of nutrients to the lower bowel after an intestinal bypass. It has attracted huge interest because it involves active glucagon-like peptide-1 (GLP-1), an incretin which potentiates insulin secretion and has been shown to increase proliferation and decrease apoptosis of the pancreatic beta cells[45], and which presents great therapeutic potential for the treatment of T2D[46]. According to this hypothesis, the delivery of ingested nutrients to the lower bowel increases GLP-1 release from entero-endocrine L-cells, which are found throughout the small intestine and in high density in the ileum. In fact, a several-fold increase of postprandial active GLP-1 secretion has been reported in a number of studies on patients after RYGB[12, 47]. The reported increases range from none to more than 5-fold in the peak value, or more than 10-fold in the area-under-curve value, for the increase in postprandial GLP-1 one week after RYGB, with large error bars (up to about 70%)[48]. There appears to be a clustering of the increases reviewed in Ref.[47] between roughly none and 2-fold or 3-fold, but it is natural that the results will vary with different groups of patients and details of the procedures. We make no attempt in this paper to exclude any published results, or to weight some results more heavily than others. However, it does appear that the case for an increase in GLP-1 levels after RYGB is rather strong. Consistent with elevated postprandial GLP-1 secretion, post-RYGB patients display an increased incretin effect[35].
Upper intestinal hypothesis
According to this hypothesis, also called the foregut hypothesis, exclusion of a short segment of proximal small intestine (primarily the duodenum) from contact with ingested nutrients produces direct antidiabetes effects, probably via one or more unidentified duodenal factors that influence glucose homoeostasis. This suggestion is supported by the results for the duodenal-jejunal bypass (DJB) procedure, which maintains the gastric volume intact while bypassing the entire duodenum and the proximal jejunum, and which was tested in several studies that showed an improvement in T2D with no reduction in body weight in animals[49–52] and in obese and non-obese human patients[53, 54]. Additional support for this hypothesis comes from the endoluminal duodenal sleeve procedure, where a flexible plastic sleeve is implanted in the upper intestine, causing food to move from the stomach to the beginning of the jejunum without coming in contact with duodenal mucosa. This technique markedly improves glucose tolerance independently of weight loss in rats[55], pigs[56], and humans[57]. This hypothesis is, however, challenged by vertical sleeve gastrectomy, a procedure that does not result in shunting of the duodenum and induces diabetes remission similar to gastric bypass[58–60]. It was also shown very recently that a duodenal bypass procedure without gastric restriction did not resolve T2D[61], in conflict with the foregut hypothesis.
Gut microbiota hypothesis
The gut microbiota refers to the billions of microorganisms inhabiting the mammalian gastrointestinal tract. It performs a large number of important roles that define the physiology of the host, such as immune system maturation, the intestinal response to epithelial cell injury, and xenobiotic and energy metabolism. On the other side, it has been directly implicated in the etiopathogenesis of a number of pathological states as diverse as obesity, autism, circulatory disease, inflammatory bowel diseases, and type 1 diabetes[62, 63]. The mechanisms through which the microbiota exerts its beneficial or detrimental influences remain largely undefined, but include elaboration of signaling molecules and recognition of bacterial epitopes by both intestinal epithelial and mucosal immune cells[62, 63]. Recently, a change in the composition of the gut microbiota after gastric bypass has been reported[64–66], which led some scientists to suggested that the rapid T2D remission after gastric bypass may be partly due to a profound influence of the surgery on the composition of the gut microflora. Mechanisms that may underlie such an effect are, however, poorly known and in need of further exploration.
Branched-chain amino acids (BCAAs) hypothesis
The concentrations of branched-chain amino acids (leucine, isoleucine, and valine) were long known to be increased in obese individuals, compared with normal weight-, age-, and sex-matched controls, and the increase was directly correlated with the fasting insulin concentration, a marker of insulin resistance[67]. In a recent prospective study involving individuals followed for 12 years, it has been shown that individuals who had high baseline levels of BCAAs are more prone to develop T2D, which suggests that high concentrations of the BCAAs might be used as a biomarker to aid in diabetes risk assessment[68]. Furthermore, Laferrère et al.[69] reported a significant reduction in circulating total amino acids, especially BCAAs, after bariatric-surgery-induced weight loss, but not after dietary intervention, suggesting that reduction in BCAAs, rather than simply weight loss, may contribute to the rapid improvement in glucose homeostasis and the resolution of T2D seen with gastric bypass surgery. However, a very recent study by Lindqvist and coworkers[70] showed an acute elevation of BCAAs (leucine and valine) after a meal in gastric bypass patients. More work is clearly needed to clarify the role of BCAAs.
Method
Perhaps the most common starting point in systems biology is a set of first-order ordinary differential equations for the concentrations of biochemical constitutents in various specific regions of an organism. The technique that we introduce here is meant to be applicable to an arbitrarily large set of such equations, but is limited to “adiabatic” (or quasi-equilibrium) states, as defined below.
Let us begin with the general set of equations

where F i is a function of the molecular concentrations x k , their derivatives dnx k /d tn, the time t, and some set of parameters r m . (Ordinarly n = 1, but the elimination of some variables may lead to higher derivatives, as when d x/d t = a y and d y/d t = b x leads to d2x/d t2 = a b x after y is eliminated). Let F i → f i when all the dnx k /d tn → 0 can be neglected:

in an “adiabatic” state, where the concentrations are changing slowly in comparison to the reaction rates. The knowns in this set of equations are some concentrations (measured or estimated) and some parameters (again measured or estimated – for example, decay rates from half-lifes). The unknowns are the remaining parameters and concentrations. The number of unknowns must be properly matched to the number of equations.
Let us now consider shifts in the concentrations x k resulting from shifts in the parameters r m . Preservation of the condition f i = 0 requires that (see below)

Eq. (3) has the form

and this set of linear inhomogeneous algebraic equations can be numerically solved to obtain ∂ x k /∂ r m . Then we can numerically integrate using

where r stands for the set of r m .
Eq. (3) follows from f i = 0 and f i +d f i = 0, with

Here the r m are varied independently and the x k vary in response to maintain the steady state, with

Eq. (3) follows because the d r m are independent. More generally, we can replace the r m by other relevant variables, such as fluxes, changes in environment, or independently-varied concentrations.
The ∂ x k /∂ r m are obtained at each step in the numerical integration from a numerical solution of Eq. (3). In order for this set of algebraic equations to have a unique solution, we need one equation (labeled by i) for each species (labeled by k). But this is the natural way to formulate the problem from the beginning.
This paper involved no experimental research or research on humans.
Results and discussion
Specific model for immediate effect of bariatric surgery on type 2 diabetes
In constructing a model for the effects of bariatric surgery, with an emphasis on the particularly successful technique of Roux-en-Y gastric bypass, it is important to be aware of the enormous complexity of the biochemical and neural pathways that are affected. However, it is also important to emphasize simplicity, because currently the details of most effects are poorly characterized, and in many cases the reported results are even controversial or contradictory. We are aware of only one previous model[71], which uses 10 equations but focuses on the effect of two incretins, GLP-1 and glucose insulinotropic polypeptide (GIP), since these two constituents are relatively well characterized. Our model is based on a slightly less conservative approach, because it appears that the main relevant effect of GLP-1 in the present context is increased insulin production (with the effects of GIP being smaller and somewhat ambiguous), and that the observed declines in homeostatic model assessment insulin resistance (HOMA-IR) following surgery[72–75] require an additional mechanism. So, in addition to (i) the incretin effect emphasized in Ref.[71], which corresponds to the usual version of the lower intestinal hypothesis, we add the two basic ways in which insulin resistance might be immediately ameliorated: (ii) Some set of substances b that induce insulin resistance might have their production diminished when the upper part of the digestive tract is bypassed. For example, as mentioned above, there appears to be evidence that insulin resistance may result from branched-chain amino acids[68, 69, 76, 77], as well as from free fatty acids. (Alternative possibilities may include anti-incretins, ghrelin, GIP, and glucagon, which might have a roughly similar effect.) The generic version of this mechanism was also considered in Ref.[71]. (iii) A different version of the lower intestinal hypothesis, in which a postulated substance a provides an additional insulin-independent pathway for glucose transport into skeletal muscle cells, and its production is enhanced when digestion is diverted to the lower part of the digestive tract. It has been established that muscle contraction due to exercise opens such an insulin-independent pathway[78–81], and evidence has even been reported for insulin-independent pathways involving nitric oxide[82], some amino acids[83], and bradykinin[84–86]. Of course, in addressing immediate effects of the surgery, we do not include the many other substances that affect appetite etc. but do not appear to be of major importance for remission after only a few days. For simplicity, we are regarding caloric restriction, ghrelin effects, and improvements in beta cell function as primarily longer-term than a few days, although one should bear in mind that these effects can be added to those explicitly included in the model. Finally, we mention that the gut microbiota hypothesis may be consistent with any of the effects in the model.
To summarize the above paragraph, we include three mechanisms for producing a decrease in glucose levels and also insulin resistance: The first is an increase in the production of incretins (primarily GLP-1). The second is a decrease in the production of substances, labeled b, which contribute to insulin resistance. The third is an increase in a substance a which provides an additional pathway for glucose to enter cells through the plasma membrane.
Time-dependent equations
Now let us write down the equations describing the time evolution of the five molecular concentrations x k which are regarded as most central in the regulation of the plasma glucose level, with x G representing glucose, x I insulin, x I incretins (with emphasis on GLP-1), x b substances which increase insulin resistance, and x a a substance which opens an insulin-independent pathway for glucose transport. The model is defined by





In Eq. (8), R
G
is the rate at which glucose is received by the plasma from digestion; r
GI
gives the rate at which insulin stimulates glucose transport in the absence of the “bad” substances b; is a factor representing the contribution of b to insulin resistance; and r
Ga
determines the rate at which the postulated “good” substance a stimulates glucose transport via an alternative pathway. (R
G
is actually the rate at which glucose is made available to the cells which normally absorb glucose via an insulin-dependent pathway, and which are therefore relevant in the present context – e.g., skeletal muscle cells.) In Eqs. (8)-(12), the final terms represent “natural disappearance”. (The degradation of incretins by dipeptidyl-peptidase 4 (DPP4) is thus not explicitly exhibited.) In Eq. (9), r
IG
gives the rate at which glucose stimulates insulin production (in the pancreas), and r
Ii
represents the enhancement by incretins. In Eq. (10), the production of incretins (stimulated by glucose in the intestine) is increased by a factor r, with a pre-surgery value r = 1 and a post-surgery value r = rmax. Finally, in Eqs. (11) and (12), r R
a
and (rmax−r)R
b
are respectively the input of substances a and b from digestion, with the same scaling assumed as for the incretins.
is a factor representing the contribution of b to insulin resistance; and r
Ga
determines the rate at which the postulated “good” substance a stimulates glucose transport via an alternative pathway. (R
G
is actually the rate at which glucose is made available to the cells which normally absorb glucose via an insulin-dependent pathway, and which are therefore relevant in the present context – e.g., skeletal muscle cells.) In Eqs. (8)-(12), the final terms represent “natural disappearance”. (The degradation of incretins by dipeptidyl-peptidase 4 (DPP4) is thus not explicitly exhibited.) In Eq. (9), r
IG
gives the rate at which glucose stimulates insulin production (in the pancreas), and r
Ii
represents the enhancement by incretins. In Eq. (10), the production of incretins (stimulated by glucose in the intestine) is increased by a factor r, with a pre-surgery value r = 1 and a post-surgery value r = rmax. Finally, in Eqs. (11) and (12), r R
a
and (rmax−r)R
b
are respectively the input of substances a and b from digestion, with the same scaling assumed as for the incretins.
Equations in an “adiabatic” postprandial state
Let us now consider an “adiabatic” state in which the concentrations are slowly varying (e.g. on a time scale ∼ hours, with a time scale for relevant reactions typically ∼ minutes). In the present context, we are concerned with postprandial states, since these are the most important in relation to glucose homeostasis. (In the fasting state, with glucose secreted from the liver rather than intestine, there would be essentially no production of incretins, and Eqs. (10)-(12) would be invalid.) There is, of course, a continuous evolution up to and down from the peak concentrations of glucose, insulin, GLP-1, etc. following ingestion, but in the model these concentrations are taken to evolve together. The scaled values which are used here may therefore apply at any point (over a period of several hours), and when integrated over time they also apply to the “area under curve” or average values of the concentrations.
With time derivatives neglected, the linear equations are trivially solved:




Substitution into the equation for x G then results in a quadratic equation. One can easily obtain the explicit solution for x G in the present case, but it is clear that this approach does not readily generalize to problems where one can have a very large number of coupled equations. This fact is what motivates the general method described in the preceding section, in which the parameters r m are treated mathematically as continuous variables. According to Eq. (3), the solution for the derivatives ∂ x k /∂ r m is a linear algebraic problem. This problem, and the subsequent integration with respect to the r m , can then be solved with standard numerical methods. An additional advantage is that some parameters may disappear when the derivatives are taken – for example, R G in Eq. (8).
Effect of surgery treated as a continuous variable
Using this approach (with r regarded as a continuous variable) one obtains




These are mathematical equations, but one can imagine a thought experiment in which these equations, and those below for x G , describe the rates at which concentrations of chemical species change as more and more of the upper digestive tract is bypassed. Applying d/d r to the condition (from Eq. (8))

then leads finally to the following equation for glucose alone:

where


Here a I , a I , α, and a1 respectively represent the strengths of the glucose-insulin-glucose interaction (i.e., insulin-stimulated glucose transport into cells), glucose-insulin-incretin-glucose interaction (i.e., the enhancement by incretins), insulin resistance due to substances b, and direct glucose transport due to substance a. We can scale these strengths by dividing numerator and denominator by the strength a I of the usual insulin mechanism:

with

We also scale the glucose concentration (along with the parameters) so that x G = 1 for r = 1.
Test of incretin hypothesis
The most common hypothesis to explain type 2 diabetes remission immediately after surgery is that it is due solely to a large enhancement of (active) GLP-1 production in the lower intestine, with a nice review of the many studies in this area by Rhee et al.[47].
We now set out to test this hypothesis. The measured enhancements of active GLP-1 range from none (or a slight decrease) to more than 10-fold[47, 48], with the majority of reported values being well below 10, and in fact ≲ 2 or 3[47], so we will show the results for

Of course, one expects variations among different groups of patients, and with different postoperative restrictions. It should also be mentioned that there are different forms of GLP-1, and that the half-life of active GLP-1 in circulation is less than 2 minutes.
The normal contribution of incretins (mainly GLP-1) to insulin secretion is usually considered to be of the order of 50−70%[87, 88]. As can be seen from Eqs. (9), (13) (with r = 1), (23), and (26),

corresponds to the incretin contribution to insulin secretion lying between 50% and 67%. But we will also include the case of 100% (implying that there would be no insulin production whatsoever without the assistance of incretins), which is given by a I = 0 in Eq. (22), or

in Eq. (25).
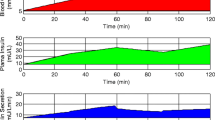
In Figure1, results are shown for the above hypothesis, that the immediate effects of surgery are due entirely to increased incretin production, and for essentially the full range of values consistent with experiment. The three lower curves in Figure1 show the decline in glucose concentration for up to a 10-fold increase in incretin production, and the horizontal line at the top shows the corresponding result for glucose × insulin, or x G × x I , which is a measure of insulin resistance analogous to homeostatic model assessment insulin resistance (HOMA-IR) measured in the fasting state. The higher two of the descending curves correspond to c i = 1 and 2 in Eq. (25), with no contribution from substances other than incretins:

Effect of incretin concentration alone. Two tests of the hypothesis that an increase in incretin concentration alone can explain the fall in glucose level and homeostatic model assessment insulin resistance (HOMA-IR) immediately after surgery. The three lower curves show the scaled glucose concentration x G as a function of the factor r by which active incretins are increased. (Reported values of r range from 1 to more than 10, with most ≲ 2 or 3.) These curves correspond to three assumptions regarding the incretin contribution to insulin production: 50% for the top curve, 67% for the middle curve, and 100% for the bottom curve. Even in the most favorable scenarios, the decrease is insufficient to explain all the observations. The horizontal line at the top is the scaled product glucose × insulin, or x G × x I , which is a measure of insulin resistance analogous to HOMA-IR. As found in Eq. (33), it is constant for all scenarios – i.e., for all values of r and all percentages for the incretin contribution. In other words, the incretin mechanism alone predicts no decrease whatsoever in this quantity. Many observations, on the other hand, show a very substantial drop in HOMA-IR immediately or very soon after surgery.
The lowest curve corresponds to the upper bound that 100% of insulin secretion is due to incretins, and it will also be discussed below.
Here we have omitted the term c G in the denominator, which correponds to the “natural disappearance” of glucose through excretion. This means that we are overestimating the decline in glucose as a function of r, since omission of c G in the denominator increases the magnitude of the negative derivative. The lowest curve in the figures are therefore extreme lower bounds on how much the glucose level and the glucose ×insulin can decline if only incretins are involved, and if 10 is taken to be the upper bound on r.
The solution to Eq. (30) is

It can be substituted into Eq. (16), which becomes

after the insulin concentration (along with the parameters) is scaled to make x I = 1 for r = 1. It follows that

Therefore, in every scenario for glucose reduction being produced entirely by incretins, there is no drop whatsoever in glucose × insulin, a quantity which is the analog in a postprandial state of HOMA-IR. The observations show, on the other hand, that HOMA-IR typically drops immediately after surgery[72–75], e.g. by 50% after one week in both obese subjects with T2D and matched subjects with normal glucose tolerance[48].
Again, the lowest curve in Figure1 corresponds to the upper bound that incretins account for 100% of insulin secretion. In this case, according to Eq. (29), Eq. (31) reduces to

The most extreme limit of possible scenarios thus gives a drop in glucose concentration of about , but more commonly reported values of r and c
i
give drops of about 0.7−1.0, as can be seen in Figure1. On the other hand, some observations show much stronger decreases soon after surgery – e.g., a drop by a factor of 0.31 (from 495 mg/dL to 153 mg/dL) in 14 days[10]. The expected long-term recovery of β-cells seems unlikely to produce such a large decrease so quickly, and in other cases there are large drops in as little as 3 days.
, but more commonly reported values of r and c
i
give drops of about 0.7−1.0, as can be seen in Figure1. On the other hand, some observations show much stronger decreases soon after surgery – e.g., a drop by a factor of 0.31 (from 495 mg/dL to 153 mg/dL) in 14 days[10]. The expected long-term recovery of β-cells seems unlikely to produce such a large decrease so quickly, and in other cases there are large drops in as little as 3 days.
There are two qualitative reasons for the above results: (i) The incretins are effective in increasing the insulin concentration, but not the insulin sensitivity of the cells. (ii) The effect of the incretins is second-order in the glucose concentration, as can be seen in Eq. (25). In other words, as the glucose concentration falls, the insulin concentration also falls, with the rate of glucose absorption being proportional to the product of these concentrations. On the other hand, the postulated substance a would have an effect that is first-order, because it directly stimulates glucose transport without insulin as an intermediary.
In summary, our results indicate that the most plausible values for an increase in GLP-1 can largely, but not completely, explain the observed beneficial changes immediately after surgery. Let us now turn to the other possibilities, considering each separately.
Test of branched-chain amino acids hypothesis (and other foregut hypotheses)
First consider the effect of only relieving the extra insulin resistance due to substances b, by setting c i = c a = 0 (and c G = 0) in Eq. (25), so that d x G /d r = −α x G /2 and

If α rmax/2 is substantial, then the glucose concentration will undergo a substantial drop. This fact lends some credibility to the branched-chain amino acids hypothesis discussed above[68, 69, 76, 77], even though insulin resistance is more commonly attributed to the release of lipids from adipose tissue.
These results actually have more general validity, since this same model can be applied to any factor from the stomach or upper intestine (duodenum and jejunum) that induces insulin resistance.
Possibility of alternative insulin-independent pathway for transport of glucose into muscle cells
Finally consider the effect of increasing only the influence of the postulated substance a, which opens an alternative pathway, by setting c i = α = 0 (and again c G = 0). Eq. (25) becomes

The results are shown in Figure2. Since the insulin level does not change in this case, the same curve describes glucose × insulin. In the limiting case of extreme insulin resistance, with a I = 0 in Eq. (22), Eq. (25) reduces to

so

Effect of alternative insulin-independent pathway. Glucose concentration x G as a function of the increase r in a substance a which opens an alternative insulin-independent pathway for glucose absorption (by the cells which are relevant in the present context). The top and middle curves are respectively for c a = 1 and 2, where c a is the strength of this alternative pathway relative to the normal insulin-dependent pathway in a patient with strong insulin resistance. The bottom curve represents the limit of extreme insulin resistance. The scaled product glucose × insulin is given by exactly these same curves, since the insulin level is constant in this case. If the present mechanism and that of Figure1 are both operative, there is, of course, an even larger drop in glucose level, and also a substantial drop in glucose × insulin. This product, in a postprandial state, is a measure of insulin resistance analogous to HOMA-IR – which is the same product measured in the fasting state.
A substance opening a new pathway could thus have a strong effect if it were produced in appreciable abundance.
In the limiting cases, the 1/r decrease of Eq. (38), in both glucose level and glucose × insulin, represents a first-order effect. On the other hand, the 1/r1/2 decrease of Eq. (34) in glucose level, with no drop of glucose × insulin in Eq. (33), represents a second-order effect, as defined below Eq. (34). This is a simple way of understanding why an insulin-independent pathway would be so effective in reducing both glucose and glucose × insulin.
Conclusions
Our general method was employed in a simple model of the response of plasma glucose concentration to bariatric surgery (with the paradigm being Roux-en-Y gastric bypass). This model includes three mechanisms that might be responsible for the remarkable positive effect observed for most patients immediately following surgery, before any appreciable weight loss. The first mechanism is the one which is currently the most widely embraced: increased production of incretins (mainly GLP-1). We performed calculations up to and including the most favorable scenario, in which there is about a 10-fold increase in the incretins and the incretins account for 100% of insulin secretion. The results, shown in Figure1, indicate that the most plausible values for an increase in GLP-1 alone cannot fully account for the decreases in glucose level which have been reported, or the large and rapid observed decreases in HOMA-IR.
In other words, we find that GLP-1 can largely, but not completely, explain the observed beneficial changes immediately after surgery.
Another possible mechanism, involving insulin resistance which is diminished when the stomach and upper intestine are bypassed, could be effective if this were indeed the main cause of type 2 diabetes in the present context. However, for obese patients undergoing bariatric surgery, the cause of insulin resistance is more commonly thought to be the release of fatty acids from fatty tissue, which will decrease only after appreciable weight loss.
This leaves the possibility that diversion of food to the lower intestine results in the production of a substance which opens an alternative insulin-independent pathway for transport of glucose into cells. As mentioned above, it has been established that exercise opens an insulin-independent pathway[78–81], involving an alternative pool of intracellular GLUT-4 which activates glucose transport through the cell membrane, and it has been argued that there are additional insulin-independent pathways involving nitric oxide[82], some amino acids[83], and bradykinin[84–86], so there are precedents for such a mechanism.
The results of Figure2 demonstrate that this would be a quite robust mechanism, which would produce large decreases in both plasma glucose and the product glucose × insulin, which provides a measure of insulin resistance analogous to HOMA-IR. If such a substance could be detected, it might, of course, be relevant to pharmaceutical approaches.
In summary, the present results suggest that another possible mechanism should be added to the current list of potential explanations for immediate glycemia normalization following Roux-en-Y gastric bypass surgery: enhanced production in the lower intestine of a substance which opens an alternative insulin-independent pathway for glucose transport.
References
Whiting DR, Guarixguata L, Weil C, Shaw J: IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011, 94: 311-321. 10.1016/j.diabres.2011.10.029.
Zimmet P, Alberti KG, Shaw J: Global and societal implications of the diabetes epidemic. Nature. 2001, 414: 782-787. 10.1038/414782a.
Pal A, McCarthy M: The genetics of type 2 diabetes and its clinical relevance. Clin Genet. 2013, 83: 297-306. 10.1111/cge.12055.
Morris AP, Voight BF, Teslovich TM, Ferreira T, Segre AV, Steinthorsdottir V, Strawbridge RJ, Khan H, Grallert H, Mahajan A, Prokopenko I, Kang HM, Dina C, Esko T, Fraser RM, Kanoni S, Kumar A, Lagou V, Langenberg C, Luan J, Lindgren CM, Muller-Nurasyid M, Pechlivanis S, Rayner NW, Scott LJ, Wiltshire S, Yengo L, Kinnuen L, Rossin EJ, Raychaudhuri S: Large-scale association analysis provides insights into the genetic architecture and pathophysiology of type 2 diabetes. Nat Genet. 2012, 44: 981-990. 10.1038/ng.2383.
Unwin N, Gan D, Whiting D: The IDF Diabetes Atlas: providing evidence, raising awareness and promoting action. Diabetes Res Clin Pract. 2010, 87: 2-3. 10.1016/j.diabres.2009.11.006.
Apelqvist J, Larsson J: What is the most effective way to reduce incidence of amputation in the diabetic foot?. Diabetes Metab Res Rev. 2000, 16 (Suppl 3): S75—S83-
American Diabetes Association, Diabetes Statistics. [http://www.diabetes.org/diabetes-basics/diabetes-statistics/], []
Butner KL, Nickols-Richardson SM, Clark SF, Ramp WK, Herbert WG: A review of weight loss following Roux-en-Y gastric bypass vs restrictive bariatric surgery: impact on adiponectin and insulin. Obes Surg. 2010, 20: 559-568. 10.1007/s11695-010-0089-z.
Garb J, Welch G, Zagarins S, Kuhn J, Romanelli J: Bariatric surgery for the treatment of morbid obesity: a meta-analysis of weight loss outcomes for laparoscopic adjustable gastric banding and laparoscopic gastric bypass. Obes Surg. 2009, 19: 1447-1455. 10.1007/s11695-009-9927-2.
Pories WJ, Mehaffey JH, Staton KM: The surgical treatment of type two diabetes mellitus. Surg Clin North Am. 2011, 91: 821-836. 10.1016/j.suc.2011.04.008.
Scalea JR, Cooper M: Surgical strategies for type II diabetes. Transplant Rev (Orlando). 2012, 26: 177-182. 10.1016/j.trre.2011.07.002.
Dirksen C, Jorgensen NB, Bojsen-Moller KN, Jacobsen SH, Hansen DL, Worm D, Holst JJ, Madsbad S: Mechanisms of improved glycaemic control after Roux-en-Y gastric bypass. Diabetologia. 2012, 55: 1890-1901. 10.1007/s00125-012-2556-7.
Franco JV, Ruiz PA, Palermo M, Gagner M: A review of studies comparing three laparoscopic procedures in bariatric surgery: sleeve gastrectomy, Roux-en-Y gastric bypass and adjustable gastric banding. Obes Surg. 2011, 21: 1458-1468. 10.1007/s11695-011-0390-5.
Heneghan HM, Nissen S, Schauer PR: Gastrointestinal surgery for obesity and diabetes: weight loss and control of hyperglycemia. Curr Atheroscler Rep. 2012, 14: 579-587. 10.1007/s11883-012-0285-5.
Buchwald H, Estok R, Fahrbach K, Banel D, Jensen MD, Pories WJ, Bantle JP, Sledge I: Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009, 122: 248-256. 10.1016/j.amjmed.2008.09.041.
Dixon JB, le Roux CW, Rubino F, Zimmet P: Bariatric surgery for type 2 diabetes. Lancet. 2012, 379: 2300-2311. 10.1016/S0140-6736(12)60401-2.
Ferchak CV, Meneghini LF: Obesity, bariatric surgery and type 2 diabetes–a systematic review. Diabetes Metab Res Rev. 2004, 20: 438-445. 10.1002/dmrr.507.
Mingrone G, Panunzi S, De GA, Guidone C, Iaconelli A, Nanni G, Pomp A, Castagneto M, Ghirlanda G, Rubino F: Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012, 366: 1577-1585. 10.1056/NEJMoa1200111.
Pournaras DJ, le Roux CW: Ghrelin and metabolic surgery. Int J Pept. 2010, 2010: 217267-
Rubino F, Gagner M, Gentileschi P, Kini S, Fukuyama S, Feng J, Diamond E: The early effect of the Roux-en-Y gastric bypass on hormones involved in body weight regulation and glucose metabolism. Ann Surg. 2004, 240: 236-242. 10.1097/01.sla.0000133117.12646.48.
Friedman MN, Sancetta AJ, Magovern GJ: The amelioration of diabetes mellitus following subtotal gastrectomy. Surg Gynecol Obstet. 1955, 100: 201-204.
Pories WJ, Swanson MS, MacDonald KG, Long SB, Morris PG, Brown BM, Barakat HA, deRamon RA, Israel G, Dolezal JM, Dohm L: Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg. 1995, 222: 339-350. 10.1097/00000658-199509000-00011.
Schauer PR, Burguera B, Ikramuddin S, Cottam D, Gourash W, Hamad G, Eid GM, Mattar S, Ramanathan R, Barinas-Mitchel E, Rao RH, Kuller L, Kelley D: Effect of laparoscopic Roux-en Y gastric bypass on type 2 diabetes mellitus. Ann Surg. 2003, 238: 467-484.
DePaula AL, Macedo AL, Mota BR, Schraibman V: Laparoscopic ileal interposition associated to a diverted sleeve gastrectomy is an effective operation for the treatment of type 2 diabetes mellitus patients with BMI 21–29. Surg Endosc. 2009, 23: 1313-1320. 10.1007/s00464-008-0156-x.
Ferzli GS, Dominique E, Ciaglia M, Bluth MH, Gonzalez A, Fingerhut A: Clinical improvement after duodenojejunal bypass for nonobese type 2 diabetes despite minimal improvement in glycemic homeostasis. World J Surg. 2009, 33: 972-979. 10.1007/s00268-009-9968-7.
Geloneze B, Geloneze SR, Fiori C, Stabe C, Tambascia MA, Chaim EA, Astiarraga BD, Pareja JC: Surgery for nonobese type 2 diabetic patients: an interventional study with duodenal-jejunal exclusion. Obes Surg. 2009, 19: 1077-1083. 10.1007/s11695-009-9844-4.
Navarrete SA, Leyba JL, Llopis SN: Laparoscopic sleeve gastrectomy with duodenojejunal bypass for the treatment of type 2 diabetes in non-obese patients: technique and preliminary results. Obes Surg. 2011, 21: 663-667. 10.1007/s11695-011-0371-8.
Rubino F, Forgione A, Cummings DE, Vix M, Gnuli D, Mingrone G, Castagneto M, Marescaux J: The mechanism of diabetes control after gastrointestinal bypass surgery reveals a role of the proximal small intestine in the pathophysiology of type 2 diabetes. Ann Surg. 2006, 244: 741-749. 10.1097/01.sla.0000224726.61448.1b.
Klein S, Ghosh A, Cremieux PY, Eapen S, McGavock TJ: Economic impact of the clinical benefits of bariatric surgery in diabetes patients with BMI ≥ 35 kg/m2. Obesity (Silver Spring). 2011, 19: 581-587. 10.1038/oby.2010.199.
Thaler JP, Cummings DE: Minireview: Hormonal and metabolic mechanisms of diabetes remission after gastrointestinal surgery. Endocrinology. 2009, 150: 2518-2525. 10.1210/en.2009-0367.
Henry RR, Wiest-Kent TA, Scheaffer L, Kolterman OG, Olefsky JM: Metabolic consequences of very-low-calorie diet therapy in obese non-insulin-dependent diabetic and nondiabetic subjects. Diabetes. 1986, 35: 155-164. 10.2337/diabetes.35.2.155.
Henry RR, Gumbiner B: Benefits and limitations of very-low-calorie diet therapy in obese NIDDM. Diabetes Care. 1991, 14: 802-823. 10.2337/diacare.14.9.802.
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, Schoelles K: Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004, 292: 1724-1737. 10.1001/jama.292.14.1724.
Karra E, Yousseif A, Batterham RL: Mechanisms facilitating weight loss and resolution of type 2 diabetes following bariatric surgery. Trends in Endocrinology and Metabolism. 2010, 21: 337-344. 10.1016/j.tem.2010.01.006.
Laferrère B, Teixeira J, McGinty J, Tran H, Egger JR, Colarusso A, Kovack B, Bawa B, Koshy N, Lee H, Yapp K, Olivan B: Effect of weight loss by gastric bypass surgery versus hypocaloric diet on glucose and incretin levels in patients with type 2 diabetes. J Clin Endocrinol Metab. 2008, 93: 2479-2485. 10.1210/jc.2007-2851.
Odstrcil EA, Martinez JG, Santa Ana CA, Xue B, Schneider RE, Steffer KJ, Porter JL, Asplin J, Kuhn JA, Fordtran JS: The contribution of malabsorption to the reduction in net energy absorption after long-limb Roux-en-Y gastric bypass. Am J Clin Nutr. 2010, 92: 704-713. 10.3945/ajcn.2010.29870.
Tong J, Prigeon RL, Davis HW, Bidlingmaier M, Kahn SE, Cummings DE, Tschop MH, D’Alessio D: Ghrelin suppresses glucose-stimulated insulin secretion and deteriorates glucose tolerance in healthy humans. Diabetes. 2010, 59: 2145-2151. 10.2337/db10-0504.
Sun Y, Asnicar M, Smith RG: Central and peripheral roles of ghrelin on glucose homeostasis. Neuroendocrinol. 2007, 86: 215-228. 10.1159/000109094.
Broglio F, Arvat E, Benso A, Gottero C, Muccioli G, Papotti M, van der Lely AJ, Deghenghi R, Ghigo E: Ghrelin, a natural GH secretagogue produced by the stomach, induces hyperglycemia and reduces insulin secretion in humans. The J Clin Endocrinol and Metab. 2001, 86: 5083-5086. 10.1210/jc.86.10.5083.
Cummings DE, Weigle DS, Frayo RS, Breen PA, Ma MK, Dellinger EP, Purnell JQ: Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N Engl J Med. 2002, 346: 1623-1630. 10.1056/NEJMoa012908.
Stoeckli R, Chanda R, Langer I, Keller U: Changes of body weight and plasma ghrelin levels after gastric banding and gastric bypass. Obes Res. 2004, 12: 346-350. 10.1038/oby.2004.43.
Chronaiou A, Tsoli M, Kehagias I, Leotsinidis M, Kalfarentzos F, Alexandrides TK: Lower ghrelin levels and exaggerated postprandial peptide-YY, glucagon-like peptide-1, and insulin responses, after gastric fundus resection, in patients undergoing Roux-en-Y gastric bypass: a randomized clinical trial. Obes Surg. 2012, 22: 1761-1770. 10.1007/s11695-012-0738-5.
Morinigo R, Casamitjana R, Moize V, Lacy AM, Delgado S, Gomis R, Vidal J: Short-term effects of gastric bypass surgery on circulating ghrelin levels. Obes Res. 2004, 12: 1108-1116. 10.1038/oby.2004.139.
Beckman LM, Beckman TR, Earthman CP: Changes in gastrointestinal hormones and leptin after Roux-en-Y gastric bypass procedure: a review. J Am Diet Assoc. 2010, 110: 571-584. 10.1016/j.jada.2009.12.023.
Drucker DJ: The role of gut hormones in glucose homeostasis. J Clin Invest. 2007, 117: 24-32. 10.1172/JCI30076.
Butler PC, Dry S, Elashoff R: GLP-1-based therapy for diabetes: what you do not know can hurt you. Diabetes Care. 2010, 33: 453-455. 10.2337/dc09-1902.
Rhee NA, Vilsbøll T, Knop FK: Current evidence for a role of GLP-1 in Roux-en-Y gastric bypass-induced remission of type 2 diabetes. Diabetes, Obes and Metab. 2012, 14: 291-298. 10.1111/j.1463-1326.2011.01505.x.
Jorgensen NB, Jacobsen SH, Dirksen C, Bojsen-Moller KN, Naver L, Hvolris L, Clausen TR, Wulff BS, Worm D, Lindqvist Hansen, Madsbad S, Holst JJ: Acute and long-term effects of Roux-en-Y gastric bypass on glucose metabolism in subjects with Type 2 diabetes and normal glucose tolerance. Am J Physiol- Endocrinol and Metabol. 2012, 303: E122-E131. 10.1152/ajpendo.00073.2012.
Cummings DE, Overduin J, Foster-Schubert KE, Carlson MJ: Role of the bypassed proximal intestine in the anti-diabetic effects of bariatric surgery. Surg Obes Relat Dis. 2007, 3: 109-115. 10.1016/j.soard.2007.02.003.
Rubino F, Marescaux J: Effect of duodenal-jejunal exclusion in a non-obese animal model of type 2 diabetes: a new perspective for an old disease. Ann Surg. 2004, 239: 1-11. 10.1097/01.sla.0000102989.54824.fc.
Wang TT, Hu SY, Gao HD, Zhang GY, Liu CZ, Feng JB, Frezza EE: Ileal transposition controls diabetes as well as modified duodenal jejunal bypass with better lipid lowering in a nonobese rat model of type II diabetes by increasing GLP-1. Ann Surg. 2008, 247: 968-975. 10.1097/SLA.0b013e318172504d.
Pacheco D, de Luis DA, Romero A, Gonzalez Sagrado M, Conde R, Izaola O, Aller R, Delgado A: The effects of duodenal-jejunal exclusion on hormonal regulation of glucose metabolism in Goto-Kakizaki rats. Am J Surg. 2007, 194: 221-224. 10.1016/j.amjsurg.2006.11.015.
Cohen RV, Schiavon CA, Pinheiro JS, Correa JL, Rubino F: Duodenal-jejunal bypass for the treatment of type 2 diabetes in patients with body mass index of 22–34 kg/m2: a report of 2 cases. Surg Obes Relat Dis. 2007, 3: 195-197. 10.1016/j.soard.2007.01.009.
Ramos AC, Galvao Neto MP, de Souza YM, Galvao M, Murakami AH, Silva AC, Canseco EG, Santamaria R, Zambrano TA: Laparoscopic duodenal-jejunal exclusion in the treatment of type 2 diabetes mellitus in patients with BMI < 30 kg/m2 (LBMI). Obes Surg. 2009, 19: 307-312. 10.1007/s11695-008-9759-5.
Aguirre V, Stylopoulos N, Grinbaum R, Kaplan LM: An endoluminal sleeve induces substantial weight loss and normalizes glucose homeostasis in rats with diet-induced obesity. Obesity (Silver Spring). 2008, 16: 2585-2592. 10.1038/oby.2008.502.
Tarnoff M, Shikora S, Lembo A, Gersin K: Chronic in-vivo experience with an endoscopically delivered and retrieved duodenal-jejunal bypass sleeve in a porcine model. Surg Endosc. 2008, 22: 1023-1028. 10.1007/s00464-007-9652-7.
Rodriguez-Grunert L, Galvao Neto MP, Alamo M, Ramos AC, Baez PB, Tarnoff M: First human experience with endoscopically delivered and retrieved duodenal-jejunal bypass sleeve. Surg Obes Relat Dis. 2008, 4: 55-59. 10.1016/j.soard.2007.07.012.
Gill RS, Birch W, Shi X, Sharma AM, Karmali S: Sleeve gastrectomy and type 2 diabetes mellitus: a systematic review. Surg Obes Relat Dis. 2010, 6: 707-713. 10.1016/j.soard.2010.07.011.
Chambers AP, Jessen L, Ryan KK, Sisley S, Wilson-Perez HE, Stefater MA, Gaitonde SG, Sorrell JE, Toure M, Berger J, D’Alessio DA, Woods SC, Seeley RJ, Sandoval DA: Weight-independent changes in blood glucose homeostasis after gastric bypass or vertical sleeve gastrectomy in rats. Gastroenterol. 2011, 141: 950-958. 10.1053/j.gastro.2011.05.050.
Chambers AP, Stefater MA, Wilson-Perez HE, Jessen L, Sisley S, Ryan KK, Gaitonde S, Sorrell JE, Toure M, Berger J, D’Alessio DA, Sandoval DA, Seeley RJ, Woods SC: Similar effects of roux-en-Y gastric bypass and vertical sleeve gastrectomy on glucose regulation in rats. Physiol Behav. 2011, 105: 120-123. 10.1016/j.physbeh.2011.05.026.
Geloneze B, Geloneze SR, Chaim E, Hirsch FF, Felici AC, Lambert G, Tambascia MA, Pareja JC: Metabolic surgery for non-obese type 2 diabetes: incretins, adipocytokines, and insulin secretion/resistance changes in a 1-year interventional clinical controlled study. Ann Surg. 2012, 256: 72-78. 10.1097/SLA.0b013e3182592c62.
Sekirov I, Russell SL, Antunes LC, Finlay BB: Gut microbiota in health and disease. Physiol Rev. 2010, 90: 859-904. 10.1152/physrev.00045.2009.
Kinross JM, Darzi AW, Nicholson JK: Gut microbiome-host interactions in health and disease. Genome Med. 2011, 3: 14-10.1186/gm228.
Furet JP, Kong LC, Tap J, Poitou C, Basdevant A, Bouillot JL, Mariat D, Corthier G, Dore J, Henegar C, Rizkalla S, Clement K: Differential adaptation of human gut microbiota to bariatric surgery-induced weight loss: links with metabolic and low-grade inflammation markers. Diabetes. 2010, 59: 3049-3057. 10.2337/db10-0253.
Li JV, Ashrafian H, Bueter M, Kinross J, Sands C, le Roux CW, Bloom SR, Darzi A, Athanasiou T, Marchesi JR, Nicholson JK, Holmes E: Metabolic surgery profoundly influences gut microbial-host metabolic cross-talk. Gut. 2011, 60: 1214-1223. 10.1136/gut.2010.234708.
Zhang H, DiBaise JK, Zuccolo A, Kudrna D, Braidotti M, Yu Y, Parameswaran P, Crowell MD, Wing R, Rittmann BE, Krajmalnik-Brown R: Human gut microbiota in obesity and after gastric bypass. Proc Natl Acad Sci U S A. 2009, 106: 2365-2370. 10.1073/pnas.0812600106.
Felig P, Marliss E: Cahill GF Jr, Plasma amino acid levels and insulin secretion in obesity. N Engl J Med. 1969, 281: 811-816. 10.1056/NEJM196910092811503.
Wang TJ, Larson MG, Vasan RS, Cheng S, Rhee EP, McCabe E, Lewis GD, Fox CS, Jacques PF, Fernandez C, O’Donnell CJ, Carr SA, Mootha VK, Florez JC, Souza A, Melander O, Clish CB, Gerszten RE: Metabolite profiles and the risk of developing diabetes. Nat Med. 2011, 17: 448-453. 10.1038/nm.2307.
Laferrère B, Reilly D, Arias S, Swerdlow N, Gorroochurn P, Bawa B, Bose M, Teixeira J, Stevens RD, Wenner BR, Bain JR, Muehlbauer MJ, Haqq A, Lien L, Shah SH, Svetkey LP, Newgard CB: Differential metabolic impact of gastric bypass surgery versus dietary intervention in obese diabetic subjects despite identical weight loss. Sci Transl Med. 2011, 3: 80re2-10.1126/scitranslmed.3002043.
Lindqvist A, Spegel P, Ekelund M, Mulder H, Groop L, Hedenbro J, Wierup N: Effects of ingestion routes on hormonal and metabolic profiles in gastric-bypassed humans. The J Clin Endocrinol and Metabol. 2013, 98: E856-E861. 10.1210/jc.2012-3996.
Toghaw P, Matone A, Lenbury Y, De Gaetano A: Bariatric surgery and T2DM improvement mechanisms: a mathematical model. Theo Biol and Med Modell. 2012, 9: 16-10.1186/1742-4682-9-16.
Wickremesekera K, Miller G, DeSilva Naotunne T, Knowles G, Stubbs RS: Loss of insulin resistance after Roux-en-Y gastric bypass surgery: a time course study. Obes Surg. 2005, 15: 474-481. 10.1381/0960892053723402.
Garrido-Sanchez L, Murri M, Rivas-Becerra J, Ocaña-Wilhelmi L, Cohen RV, Garcia-Fuentes E, Tinahones FJ: Bypass of the duodenum improves insulin resistance much more rapidly than sleeve gastrectomy. Surg for Obes and Related Dis. 2012, 8: 145-150. 10.1016/j.soard.2011.03.010.
Rao RS, Yanagisawa R, Kini S: Insulin resistance and bariatric surgery. Obes Rev. 2012, 13: 316-328. 10.1111/j.1467-789X.2011.00955.x.
Ferrannini E, Mingrone G: Impact of different bariatric surgical procedures on insulin action and β-cell function in type 2 diabetes. Diabetes Care. 2009, 32: 514-520. 10.2337/dc08-1762.
Terruzzi I, Allibardi S, Bendinelli P, Maroni P, Piccoletti R, Vesco F, Samaja M, Luzi L: Amino acid- and lipid-induced insulin resistance in rat heart: molecular mechanisms. Mol and Cell Endocrinol. 2002, 190: 135-145. 10.1016/S0303-7207(02)00005-9.
Newgard CB: Interplay between lipids and branched-chain amino acids in development of insulin resistance. Cell Metabol. 2012, 15: 606-614. 10.1016/j.cmet.2012.01.024.
Goodyear LJ, Kahn BB: Exercise, glucose transport, and insulin sensitivity. Annu Rev Med. 1998, 49: 235-261. 10.1146/annurev.med.49.1.235.
Dohm GL: Regulation of skeletal muscle GLUT-4 expression by exercise. J Appl Physiol. 2002, 93: 782-787.
Rose AJ, Richter EA: Skeletal muscle glucose uptake during exercise: how is it regulated?. Physiol. 2005, 20: 260-270. 10.1152/physiol.00012.2005.
Röckl KSC, Witczak CA, Goodyear LJ: Signaling mechanisms in skeletal muscle: acute responses and chronic adaptations to exercise. IUBMB Life. 2008, 60: 145-153. 10.1002/iub.21.
Higaki Y, Hirshman MF, Fujii N, Goodyear LJ: Nitric oxide increases glucose uptake through a mechanism that is distinct from the insulin and contraction pathways in rat skeletal muscle. Diabetes. 2001, 50: 241-247. 10.2337/diabetes.50.2.241.
Flati V, Pasini E, D’Antona G, Speca S, Toniato E, Martinotti S: Intracellular mechanisms of metabolism regulation: the role of signaling via the mammalian target of rapamycin pathway and other routes. Am J Cardiol. 2008, 101 (suppl): 16E-21E.
Shepherd PR, Kahn BB: Glucose transporters and insulin action – implications for insulin resistance and diabetes mellitus. N Engl J Med. 1999, 341: 248-257. 10.1056/NEJM199907223410406.
Kishi K, Muromoto N, Nakaya Y, Miyata I, Hagi A, Hayashi H, Ebina Y: Bradykinin directly triggers GLUT4 translocation via an insulin-independent pathway. Diabetes. 1998, 47: 550-558. 10.2337/diabetes.47.4.550.
Taguchi T, Kishikawa H, Motoshima H, Sakai K, Nishiyama T, Yoshizato K, Shirakami A, Toyonaga T, Shirontani T, Araki E, Shichiri M: Involvement of bradykinin in acute exercise-induced increase of glucose uptake and GLUT-4 translocation in skeletal muscle: studies in normal and diabetic humans and rats. Metabol. 2000, 49: 920-390. 10.1053/meta.2000.6755.
Fetner R, McGinty J, Russell C, Pi-Sunyer FX, Laferrère B: Incretins, diabetes, and bariatric surgery: a review. Surg for Obes and Relat Dis. 2005, 1: 589-598. 10.1016/j.soard.2005.09.001.
Baggio LL, Drucker DJ: Biology of Incretins: GLP-1 and GIP. Gastroenterol. 2007, 132: 2131-2157. 10.1053/j.gastro.2007.03.054.
Acknowledgements
This work was supported by the Qatar Foundation through the Qatar Biomedical Research Institute, and by the Science Program at Texas A&M University at Qatar.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
AA proposed the project, surveyed the literature, and wrote the Background section. RA further surveyed the literature, devised the method, formulated the model, solved the equations, and wrote the remainder of the paper. TH, JLN, and RO participated in regular discussions and provided input for formulation of the model and the biomedical context. MAG and OB verified all the mathematics. MAG additionally created the figures and made suggestions regarding the biomedical context. PF contributed to discussion and revision of the paper. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Allen, R.E., Hughes, T.D., Ng, J.L. et al. Mechanisms behind the immediate effects of Roux-en-Y gastric bypass surgery on type 2 diabetes. Theor Biol Med Model 10, 45 (2013). https://doi.org/10.1186/1742-4682-10-45
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1742-4682-10-45