Abstract
Background
Although different techniques for sperm immobilization have been described, their value has not been assessed in an adequately powered randomized study. The aim of this study was to compare two types of sperm immobilization methods prior to ICSI and to test the hypothesis that triple touch immobilization (TTIm) would lead to a higher (5% -65% up to 70%) fertilization rate (FR) than single touch immobilization (STIm).
Methods
A total of 3056 metaphase II (MII) oocytes, from 290 patients, were randomly assigned to the STIm group (n = 1528 oocytes; 145 cycles) or to the TTIm group (n = 1528 oocytes; 138 cycles). A total of 1478 oocytes (STIm group) and 1476 oocytes (TTIm group) were used in the statistical analysis. The primary outcome variable was FR. Secondary outcome variables included: number of good quality embryos (GQE) on day 2 and day 3, implantation rate (IR) and implantation with foetal heart beat rate (FHB). Statistical analysis was done using the Fisher Exact test with a significance level of 0.05.
Results
The results showed no differences in FR between both groups. The proportion of good quality embryos on day 3, was significantly higher in the STIm group (37.5%) compared to the TTIm group (31.8%; p = 0.02).
Conclusions
In this RCT, the hypothesis that the post-ICSI FR would be higher after TTIm than after STIm was not confirmed and the number of good quality embryos on day 3 was significantly lower in the TTIm group than in the STIm group. These data suggest that more ‘aggressive’ TTIm technique has no advantages compared to the STIm technique.
Similar content being viewed by others
Background
Sperm plasma membrane damage has been described as a necessary process prior to intracytoplasmic sperm injection (ICSI) [1–4], as it plays a key role in the oocyte activation caused by the spermatozoon [3, 4]. However, it is not fully understood to which extent sperm plasma membrane damage [3] is needed for adequate oocyte activation in the context of Assisted Reproductive Technology (ART) treatments.
Since the introduction of ICSI a number of studies have been conducted to evaluate the immobilization of spermatozoa prior to ICSI as a method to induce sperm plasma membrane damage before ICSI. Immobilization induces permeabilization of the sperm membrane and enhances subsequent nuclear decondensation [3]. Although the use of motile sperm cells instead of immobilized sperm has been promoted in the past [5], most studies agree that the use of immobilized sperm is necessary to provoke the processes needed prior to fertilization [1–4, 6].
Different immobilization techniques can be used to induce sperm membrane permeabilization. The conventional method for immobilization consists of compressing the tail of the spermatozoon against the bottom of a dish with a micro injection pipette until a clear bend is visible [4]. More aggressive mechanical techniques include: permanently crimping the tail in the mid-piece region [4], cutting the tail below the mid-piece region [7], cutting halfway between the head and the tip of the tail [1] and dissecting the tail at the tip [8]. Finally, the application of lasers [9–11] or piezo-pulses [12] to sperm tails can induce sperm immobilization prior to ICSI.
When compared to the standard method, higher post ICSI fertilization rates for ejaculated spermatozoa have been reported after more aggressive mechanical [1, 2, 4, 7] or piezo-pulse induced [12] sperm immobilization, but not after cutting the tail of the spermatozoon at different places [6] or applying laser-induced (non-contact 1.48-μm diode laser) sperm immobilization [10, 11] techniques for sperm immobilization.
Although different techniques for sperm immobilization before ICSI have been described, their value has not been assessed in an adequately powered randomized study. The majority of studies mentioned above were published more than 10 years ago in selected groups, i.e. men with oligoterato- or oligoasthenozoospermia [1, 7] and using a low number of oocytes (about 500 oocytes) except for 1 study (6419 oocytes) [4]. No subsequent study has been conducted recently, including a large number of oocytes in a patient population representative for routine clinical practice. As biological plausibility [3] and observational literature data support the possibility that more sperm plasma membrane damage may lead to higher fertilization rate after ICSI, the aim of our study was to test the hypothesis that triple touch sperm immobilization (TTIm) would lead to a higher fertilization rate (FR) after ICSI than single touch sperm immobilization (STIm). The hypothesis is that the damage induced to the mid-piece region would imply a more successful outcome in ICSI, due to the fact that the mitochondria are tightly packed and located only in the mid-piece region [13].
Methods
Patients
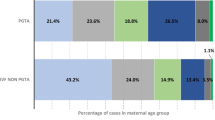
All ART ICSI cycles between April 2009 and January 2010 were eligible for our randomized study, except ICSI cycles combined with pre-implantation genetic diagnosis (PGD), or ICSI cycles using either immotile sperm from fresh ejaculate, or sperm from testicular biopsies. Patients received treatment with ICSI mostly for the indication of severe male factor infertility (87%) (See Table 1). The ovarian stimulation and egg retrieval protocols have been described in detail before [14].
Semen collection and preparation
Briefly, semen samples were processed following the SOPs (Standard Operating Procedures) of the Leuven University Fertility Centre (LUFC).
Semen samples were collected by masturbation and prepared after liquefaction (20 minutes at 37°C) [15, 16]. The samples were prepared on a three layer Isolate gradient (100%, 70%, and 50%) (IsolateTM, Irvine Scientific, Santa Ana, USA) and washed with HEPES-buffered culture medium (Gynemed, Lensahn, Germany).
ICSI procedure
The micromanipulation procedure was performed on the lid of a Petri dish (Nunc, Thermo Scientific, Roskilde, Denmark) using droplets (20 μl) of HEPES-buffered culture medium (Gynemed, Lensahn, Germany), incubated at 37°C in 5% CO2 in air. To avoid evaporation, droplets were covered with mineral oil (GM, Gynemed, Lensahn, Germany). Prior to ICSI, a small amount of spermatozoa (± 5 μl) was placed in a polyvinylpyrrolidone droplet (GM PVP, Gynemed, Lensahn, Germany). Injection pipettes (COOK Cook, Brisbane, Australia/Humagen Origio, Malov, Denmark) and holding pipettes (COOK Cook, Brisbane, Australia) were used for micromanipulation. Micromanipulation (at 37°C on a heating plate) was performed using an inverted microscope with modulation contrast using a 200x magnification.
Sperm immobilization and randomization
Randomization was performed at the time of oocyte denudation. In case of an odd number of MII oocytes, the last oocyte was randomized using a blinded envelope system. Sibling MII oocytes were randomly assigned to the STIm or TTIm technique. In the STIm group, immobilization was performed by pressing the tail of the spermatozoon to the bottom of the dish with the injection pipette and then quickly withdrawing this pipette until a clear bent in the middle of the flagellum was observed [2, 17, 18] (see Figure 1). In the TTIm group the spermatozoon was immobilized three times: twice on the tail (STIm technique applied twice) and once by compressing the mid-piece [8, 19] (see Figure 1). In case of not performing the STIm or TTIm technique in a correct manner (further kinetic movement of the sperm tail), another spermatozoa was selected and permanently immobilized for the injection in “either” groups.
Sperm immobilization. (a) Standard procedure STIm : pressing the tip of the tail against the lid of the dish with a microinjection pipette until a clear small bend in the middle of the flagellum is visible (b) More aggressive procedure TTIm: based on application of the standard procedure twice and compression of the sperm mid-piece once.
Fertilization control and embryo evaluation, embryo transfer
After injection the oocytes were washed in droplets of culture medium and placed into a new culture dish with culture medium, divided into two groups (co-cultured) and incubated overnight.
For both the STIm and TTIm group, fertilization control was performed 16 to 20 hours later on a stereomicroscope on 37°C. Oocytes showing 2 pronuclei (2PN) were identified as normally fertilized and were cultured individually, the presence of 1 (PN) or 3 (3PN) pronuclei was considered as abnormally fertilized.
On day 2 and day 3, embryo quality was assessed using embryo development and morphology. The number and size of blastomeres and the percentage of fragmentation was evaluated. A good quality embryo (GQE) on day 2 was defined as a 4- cell stage embryos with less than 25% fragmentation and equally or slightly unequally sized blastomeres and on day 3 (7-, 8-, or 9- cell stage embryo with less than 25% fragmentation and equally or slightly unequally sized blastomeres). On day 5 the blastocyst stage was evaluated based on the presence of the inner cell mass, the trophectoderm layer, the blastocoel and the degree of expansion as described before [20]. A blastocyst with a blastocoel completely filling the embryo, a tightly packed inner cell mass and a trophectoderm with many cells forming a cohesive epithelium was defined as a good quality blastocyst at day 5.
A single (SET) or double (DET) embryo transfer was performed, independent from the immobilization technique, on day 2 (N = 47), day 3 (N = 404) or day 5 (N = 8) according to the transfer policy decided by the gynaecologist (based on the Belgian law of July 2003) at the start of the cycle and the number of fertilized oocytes on day 1.
Clinical implantation and pregnancy results were obtained for the STIm versus TTIm method and also for mixed embryo transfers.
Outcome variable and power calculation
This study was performed on sibling oocytes to test the hypothesis that the fertilization rate (FR) per oocyte would be higher in the TTIm group (70%) than in the STIm group (65%) based on the average FR in our fertility centre during 2008.
The primary outcome variable was the FR, defined as the number of normally fertilized oocytes over the total number of MII oocytes and over the total number of successfully injected MII oocytes. Therefore a total of 1528 mature oocytes were required in each group assuming a power of 0.80, α = 0.05, resulting in a total of 3056 MII oocytes in the whole study.
Secondary outcome variables included: number of good quality embryos (GQE) on day 2 and day 3, utilisation rate (number of embryos available for embryo transfer and cryopreservation over the total number of normally fertilized oocytes) (UR), implantation rate per embryo transferred (IR) [21] and implantation rate with foetal heart beat per embryo transferred (FHB). Statistical analyses were done using the Fisher Exact test with a significance level of 0.05.
Results
This randomised study, performed between April 2009 and January 2010 in 290 ICSI cycles, was done with a total number of 3532 oocytes and after removal of the cumulus cells, 3056 MII oocytes were available for ICSI. After randomisation, 1528 MII oocytes (145 cycles) were assigned to the STIm group and 1528 MII oocytes (138 cycles) to the TTIm group. Oocytes (102MII) were excluded from the analysis due to missing data on day 2 or day 1, if they were excluded for analysis for day 2, than they were automatically excluded for day 1. Respectively 50 oocytes (STIm group) and 52 oocytes (TTIm group) were excluded from the analysis (see Figure 2). Consequently, 1478 MII for the STIm group and 1476 MII for the TTIm group were available for analysis. Mean age (±SD) was 31.7 (±4.5) and 34.6 (±6.0) for female and male partner respectively.
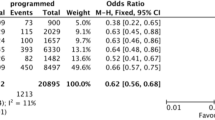
Both groups were comparable with respect to the fertilization rate per injected MII oocyte (STIm: 67.1% vs TTIm: 66.7%), fertilization rate per successfully injected MII oocyte (STIm: 74.8% vs 75.8%), percentage of abnormally fertilized oocytes (STIm: 6.7% vs TTIm: 6.1%) and the embryo utilisation rate (STIm: 51.7% vs TTIm: 47.2%) (UR) (Table 2). The number of good quality embryos on day 3 was significantly higher in the STIm group compared to the TTIm group (STIm: 37.5% vs TTIm: 32.2%; p 0.02). The embryo quality on day 2 (STIm: 33.0% vs TTIm: 31.8%) and day 5 (STIm: 17.2% vs TTIm: 20.7%) was comparable in both groups, although only a small number of day 5 blastocysts were included (Table 2). The pregnancy outcome as measured by IR per embryo transferred (STIm: 31.0% vs TTIm: 23.9%) and IR with foetal heart beat per embryo transferred (STIm: 27.6% vs TTIm: 23.2%) was comparable in the STIm group and the TTIm group (see Table 3).
Discussion
In this RCT, the hypothesis that the post-ICSI FR would be higher after TTIm than after STIm was not confirmed. Furthermore, the proportion of good quality embryos on day 3 (secondary outcome variable) was significantly lower in the TTIm group than in the STIm group. Collectively, these data suggest that more ‘aggressive’ TTIm technique has no advantages compared to the STIm technique before ICSI. To the best of our knowledge, our study represents the first randomized study in a large patient population, with FR as primary outcome variable, based on a priori power calculation and a sufficiently high number (n = 2954) sibling MII oocytes available for analysis.
The results of our study confirm the data (similar FR and embryo quality on day 2) from another RCT [8], but including only 205 MII oocytes to compare 3 different immobilization techniques: compressing the mid-piece (comparable to the TTIm technique used in our study), cutting the tail at the mid-portion and dissecting the tail of the spermatozoon at the tip. However, the results of our study are in disagreement with the increased FR after ICSI reported in non-randomized retrospective case control studies [1, 2, 4, 7] using other mechanical, aggressive sperm immobilization techniques in different types of spermatozoa (immotile, thawed, epididymal), when compared to the standard immobilization method. Furthermore, when compared to STIm, we did not confirm improved outcome after TTIm for previously reported secondary outcome variables like: a significant decline in degenerated oocytes [7] or a decrease of the number of 1PN oocytes [1].
The results of our study don’t allow us to draw conclusions on the underlying mechanisms. A possible consideration could be that the amount of damage needed to immobilize a motile spermatozoa is not depending on the number of strokes (STIm vs TTIm) but rather on the region (mid-piece) where we immobilized the sperm tail. We have to keep in mind that other reactions such as hyperactivity due to the mitochondria at the site of fertilization might have an influence on the fertilization rate [13]. In addition, we cannot exclude, based on our results, that no additional damage occurs to the centrosomes of the spermatozoa after both immobilization techniques. The importance of centrosomes has been studied in the last few years, however the exact comprehension of the mechanisms remains unclear [22].
Conclusions
In conclusion, this randomized trial showed that, when compared to STIm, TTIm did not result in a higher post-ICSI fertilization rate (primary outcome) and was associated with a lower number of good quality embryos on day 3 and with similar pregnancy rates (secondary outcomes), suggesting that the more ‘aggressive’ TTIm technique has no advantages compared to the STIm technique before ICSI.
References
Gerris J, Mangelschots K, Van Royen E, Joostens M, Eestermans W, Ryckaert G: ICSI and severe male factor infertility: breaking the sperm tail prior to injection. Hum Reprod. 1995, 10: 484-504.
Van den Bergh M, Bertrand E, Biramane J, Englert Y: Importance of breaking a spermatozoon’s tail before intracytoplasmic injection: a prospective randomized trial. Hum Reprod. 1995, 10: 2819-2820.
Dozortsev D, Rybouchkin A, De Sutter P, Dhont M: Sperm plasma membrane damage prior to intracytoplamsic sperm injection: a necessary condition for sperm nucleus decondensation. Hum Reprod. 1995, 10: 2960-2964.
Palermo G, Schlegel P, Colombero L, Zaninovic N, Moy F: Rosenwaks: aggressive sperm immobilization prior to intracytoplasmic sperm injection with immature spermatozoa improves fertilization and pregnancy rates. Hum Reprod. 1996, 11: 1023-1029. 10.1093/oxfordjournals.humrep.a019290.
Hoshi K, Yanagida K, Yazawa H, Katayose H, Sato A: Intracytoplasmic sperm injection using immobilized or motile human spermatozoon. Fertil. Steril. 1995, 63: 1241-1245.
Takeuchi T, Colombero LT, Nerii QV, Rosenwaks Z, Palermo G: Does ICSI require acrosomal disruption? An ultrastructural study. Hum Reprod. 2011, 19: 114-117.
Fishel S, Lisi F, Rinaldi L, Green S, Hunter A, Dowell K, Thornton S: Systematic examination of immobilizing spermatozoa before intracytoplasmic sperm injection in the human. Hum Reprod. 1995, 10: 497-500.
Chen SU, Ho HN, Chen HF, Huang SC, Lee TT, Yang YS: Intracytoplasmic sperm injection (ICSI) for severe semen abnormalities: dissecting the tail of spermatozoa at the tip. Hum Reprod. 1996, 11: 2640-2644. 10.1093/oxfordjournals.humrep.a019185.
Montag M, Rink K, Delacrétez G, van der Ven H: Laser induced immobilization and plasma membrane permeabilization in human spermatozoa. Hum Reprod. 2000, 15: 846-852. 10.1093/humrep/15.4.846.
Ebner T, Yaman C, Moser M, Sommergruber M, Hart J, Tews G: Laser assisted immobilization of spermatozoa prior to intracytoplasmic sperm injection in humans. Hum Reprod. 2001, 16: 2628-2631. 10.1093/humrep/16.12.2628.
Debrock S, Spiessens C, Afschrift H, Van der Auwere I, D’Hooghe TM: Application of the Fertilase laser system versus the conventional mechanical method to immobilize spermatozoa for intracytoplasmic sperm injection A randomized controlled trail. Gynecol Obstet Invest. 2003, 56: 102-105. 10.1159/000072995.
Yanagida K, Katayose H, Yazawa H, Kimura Y, Konnai K, Sato A: The usefulness of a piezo-micromanipulator in intracytoplasmic sperm injection in humans. Hum Reprod. 1999, 14: 448-453. 10.1093/humrep/14.2.448.
Piomboni P, Focarelli R, Stendardi A, Ferramosca A, Zara V: The role of mitochondria in energy production for human sperm motility. Int J Androl. 2012, 35: 109-124. 10.1111/j.1365-2605.2011.01218.x.
Debrock S, Melotte C, Spiessens C, Peeraer K, Vanneste E, Meeuwis L, Meuleman C, Frijns JP, Vermeersch JR, D’Hooghe TM: Pre-implantation genetic screening for aneuploidy of embryo’s after in vitro fertilization in women aged at least 35 years: a prospective randomized trial. Ferti Steril. 2010, 93: 364-373. 10.1016/j.fertnstert.2008.10.072.
Palermo G, Joris H, Derde MP: Sperm characteristics and outcome of human assisted fertilization by subzonal insemination and intracytoplasmic sperm injection. Fertil Steril. 1993, 59: 826-835.
Palermo G, Cohen J, Alikani M, Adler A, Rosenwaks: Intracytoplasmic sperm injection: a novel treatment for all forms of male factor infertility. Fertil Steril. 1995, 63: 1231-1240.
Van Steirteghem AC, Liu J, Joris H, Nagy Z, Staessen C, Smitz J, Wisanto A, Devroey P: High fertilization and implantation rates after intracytoplasmic sperm injection. Hum Reprod. 1993, 8: 1061-1066.
Van Steirteghem AC, Liu J, Joris H, Nagy Z, Janssenswillen C, Tournaye H, Derde MP, Van Assche E, Devroey P: Higher success rate by intracytoplasmic sperm injection than by subzonal insemination. Report of a second series of 300 consecutive treatment cycles. Hum Reprod. 1993, 8: 1055-1060.
Tucker MJ, Morton PC, Witt MA, Wright G: Intracytoplasmic injection of testicular and epididymal spermatozoa for treatment of obstructive azoospermia. Hum Reprod. 1995, 10: 486-489.
Gardner DK, Schoolcraft WB: Towards Reproductive Certainty: infertility and Genetics beyond 1999. In vitro culture of the human blastocyst. 1999, Edited by: Jansen R, Mortimer D, Carnforth, UK. Parthenon publishing, 378-388.
Zegers-Hochshild F, Adamson GD, de Mouzon J, Ishihara O, Mansour R, Nygren K, Sullivan E, Vanderpoel S: International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology. Fertil Steril. 2009, 92: 1520-1524. 10.1016/j.fertnstert.2009.09.009.
Bo Yon L, Sang Woo S, Young Sun K, Seung Bo K: The presence of centrioles and centrosomes in ovarian mature cystic teratoma cells suggest human parthenotes developed in vitro can differentiate into mature cells without a sperm centriole. BBRC. 2011, 415: 401-404.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
VA and SC designed the study. VA and PG analysed and interpreted the data. These authors draft the paper and approved the final version. DS, D’HT and CS interpreted the data and revised the paper critically for intellectual content and approved the final version. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Velaers, A., Paternot, G., Debrock, S. et al. Triple touch sperm immobilization vs. single touch sperm immobilization in ICSI - a randomised trial. Reprod Biol Endocrinol 10, 65 (2012). https://doi.org/10.1186/1477-7827-10-65
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1477-7827-10-65