Abstract
Purpose
In this first of two companion papers, we critically review the evidence recently published in the primary literature, which addresses adverse maternal and neonatal pregnancy outcomes associated with programmed embryo transfer cycles. We next consider whether these pathological pregnancy outcomes might be attributable to traditional risk factors, unknown parental factors, embryo culture, culture duration, or cryopreservation. Finally, in the second companion article, we explore potential etiologies and suggest strategies for prevention.
Methods
Comprehensive review of primary literature.
Results
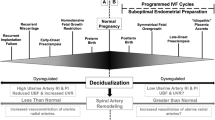
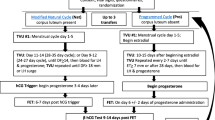
The preponderance of retrospective and prospective observational studies suggests that increased risk for hypertensive disorders of pregnancy (HDP) and preeclampsia in assisted reproduction involving autologous embryo transfer is associated with programmed cycles. For autologous frozen embryo transfer (FET) and singleton live births, the risk of developing HDP and preeclampsia, respectively, was less for true or modified natural and stimulated cycles relative to programmed cycles: OR 0.63 [95% CI (0.57–0.070)] and 0.44 [95% CI (0.40–0.50)]. Though data are limited, the classification of preeclampsia associated with programmed autologous FET was predominantly late-onset or term disease. Other adverse pregnancy outcomes associated with autologous FET, especially programmed cycles, included increased prevalence of large for gestational age infants and macrosomia, as well as higher birth weights. In one large registry study, FET was associated with fetal overgrowth of a symmetrical nature. Postterm birth and placenta accreta not associated with prior cesarean section, uterine surgery, or concurrent placenta previa were also associated with autologous FET, particularly programmed cycles. The heightened risk of these pathologic pregnancy outcomes in programmed autologous FET does not appear to be attributable to traditional risk factors, unknown parental factors, embryo culture, culture duration, or cryopreservation, although the latter may contribute a modest degree of increased risk for fetal overgrowth and perhaps HDP and preeclampsia in FET irrespective of the endometrial preparation.
Conclusions
Programmed autologous FET is associated with an increased risk of several, seemingly diverse, pathologic pregnancy outcomes including HDP, preeclampsia, fetal overgrowth, postterm birth, and placenta accreta. Though the greater risk for preeclampsia specifically associated with programmed autologous FET appears to be well established, further research is needed to substantiate the limited data currently available suggesting that the classification of preeclampsia involved is predominately late-onset or term. If substantiated, then this knowledge could provide insight into placental pathogenesis, which has been proposed to differ between early- and late-onset or term preeclampsia (see companion paper for a discussion of potential mechanisms). If a higher prevalence of preeclampsia with severe features as suggested by some studies is corroborated in future investigations, then the danger to maternal and fetal/neonatal health is considerably greater with severe disease, thus increasing the urgency to find preventative measures. Presupposing significant overlap of these diverse pathologic pregnancy outcomes within subjects who conceive by programmed embryo transfer, there may be common etiologies.


Similar content being viewed by others
Data availability
Not applicable.
Notes
Because the use of true or modified NC was not consistently specified in the literature, we combined the two approaches for discussion.
References
Mumusoglu S, Polat M, Ozbek IY, Bozdag G, Papanikolaou EG, Esteves SC, et al. Preparation of the endometrium for frozen embryo transfer: a systematic review. Front Endocrinol (Lausanne). 2021;12:688237.
Sha T, Yin X, Cheng W, Massey IY. Pregnancy-related complications and perinatal outcomes resulting from transfer of cryopreserved versus fresh embryos in vitro fertilization: a meta-analysis. Fertil Steril. 2018;109(2):330-42 e9.
Sullivan-Pyke C, Dokras A. Preimplantation genetic screening and preimplantation genetic diagnosis. Obstet Gynecol Clin North Am. 2018;45(1):113–25.
Wei D, Liu JY, Sun Y, Shi Y, Zhang B, Liu JQ, et al. Frozen versus fresh single blastocyst transfer in ovulatory women: a multicentre, randomised controlled trial. Lancet. 2019;393(10178):1310–8.
Zaat T, Zagers M, Mol F, Goddijn M, van Wely M, Mastenbroek S. Fresh versus frozen embryo transfers in assisted reproduction. The Cochrane Database Systematic Rev. 2021;2(2):CD011184.
Conrad KP, von Versen-Hoynck F, Baker VL. Potential role of the corpus luteum in maternal cardiovascular adaptation to pregnancy and preeclampsia. Am J Obstet Gynecol. 2022;226:683–99.
Petersen SH, Westvik-Johari K, Spangmose AL, Pinborg A, Romundstad LB, Bergh C, et al. Risk of hypertensive disorders in pregnancy after fresh and frozen embryo transfer in assisted reproduction: a population-based cohort study with within-sibship analysis. Hypertension. 2023;80(2):e6–16.
Li C, He YC, Xu JJ, Wang Y, Liu H, Duan CC, et al. Perinatal outcomes of neonates born from different endometrial preparation protocols after frozen embryo transfer: a retrospective cohort study. BMC Pregnancy Childbirth. 2021;21(1):341.
Pape J, Levy J, von Wolff M. Hormone replacement cycles are associated with a higher risk of hypertensive disorders: retrospective cohort study in singleton and twin pregnancies. BJOG. 2023;130(4):377–86.
Xu J, Zhou H, Zhou T, Guo Y, Liang S, Jia Y, et al. The impact of different endometrial preparation protocols on obstetric and neonatal complications in frozen-thawed embryo transfer: a retrospective cohort study of 3,458 singleton deliveries. Reprod Biol Endocrinol. 2022;20(1):141.
Opdahl S, Henningsen AA, Tiitinen A, Bergh C, Pinborg A, Romundstad PR, et al. Risk of hypertensive disorders in pregnancies following assisted reproductive technology: a cohort study from the CoNARTaS group. Hum Reprod. 2015;30(7):1724–31.
Pijnenborg R, Vercruysse L, Hanssens M. The uterine spiral arteries in human pregnancy: facts and controversies. Placenta. 2006;27(9–10):939–58.
Brosens I, Pijnenborg R, Vercruysse L, Romero R. The, “great obstetrical syndromes” are associated with disorders of deep placentation. Am J Obstet Gynecol. 2011;204(3):193–201.
Melchiorre K, Giorgione V, Thilaganathan B. The placenta and preeclampsia: villain or victim? Am J Obstet Gynecol. 2022;226(2S):S954–62.
Conrad KP, Bernstein IM, Gernand AD. Preconceptional and periconceptional pathways to preeclampsia. In: Taylor RN, Conrad KP, Davidge ST, Staff AC, Roberts JM, editors. Chesley’s hypertensive disorders of pregnancy. 5th ed. San Diego, CA: Elsevier; 2022. p. 71–94.
Burton GJ, Woods AW, Jauniaux E, Kingdom JC. Rheological and physiological consequences of conversion of the maternal spiral arteries for uteroplacental blood flow during human pregnancy. Placenta. 2009;30(6):473–82.
Redman CW, Sargent IL, Staff AC. IFPA Senior award lecture: making sense of pre-eclampsia - two placental causes of preeclampsia? Placenta. 2014;35(Suppl):S20–5.
Jones CJ, Fox H. Ultrastructure of the placenta in prolonged pregnancy. J Pathol. 1978;126(3):173–9.
Roberts JM, Rich-Edwards JW, McElrath TF, Garmire L, Myatt L, Global PC. Subtypes of preeclampsia: recognition and determining clinical usefulness. Hypertension. 2021;77(5):1430–41.
von Versen-Hoynck F, Schaub AM, Chi YY, Chiu KH, Liu J, Lingis M, et al. Increased preeclampsia risk and reduced aortic compliance with in vitro fertilization cycles in the absence of a corpus luteum. Hypertension. 2019;73(3):640–9.
Wiegel RE, Jan Danser AH, Steegers-Theunissen RPM, Laven JSE, Willemsen SP, Baker VL, et al. Determinants of maternal renin-angiotensin-aldosterone-system activation in early pregnancy: insights from 2 cohorts. J Clin Endocrinol Metab. 2020;105(11):3505–17.
Sites CK, Wilson D, Barsky M, Bernson D, Bernstein IM, Boulet S, et al. Embryo cryopreservation and preeclampsia risk. Fertil Steril. 2017;108(5):784–90.
Niu Y, Suo L, Zhao D, Wang Y, Miao R, Zou J, et al. Is artificial endometrial preparation more associated with early-onset or late-onset preeclampsia after frozen embryo transfer? J Assist Reprod Genet. 2023;40(5):1045–54.
Luke B, Brown MB, Eisenberg ML, Callan C, Botting BJ, Pacey A, et al. In vitro fertilization and risk for hypertensive disorders of pregnancy: associations with treatment parameters. Am J Obstet Gynecol. 2020;222(4):350-e1- e13.
Roelens C, Racca A, Mackens S, Van Landuyt L, Buelinckx L, Gucciardo L, et al. Artificially prepared vitrified-warmed embryo transfer cycles are associated with an increased risk of pre-eclampsia. Reprod Biomed Online. 2022;44(5):915–22.
Moreno-Sepulveda J, Espinos JJ, Checa MA. Lower risk of adverse perinatal outcomes in natural versus artificial frozen-thawed embryo transfer cycles: a systematic review and meta-analysis. Reprod Biomed Online. 2021;42(6):1131–45.
Busnelli A, Schirripa I, Fedele F, Bulfoni A, Levi-Setti PE. Obstetric and perinatal outcomes following programmed compared to natural frozen-thawed embryo transfer cycles: a systematic review and meta-analysis. Hum Reprod. 2022;37(7):1619–41.
Zaat TR, Kostova EB, Korsen P, Showell MG, Mol F, van Wely M. Obstetric and neonatal outcomes after natural versus artificial cycle frozen embryo transfer and the role of luteal phase support: a systematic review and meta-analysis. Hum Reprod Update. 2023;29(5):634–54.
Fan L, Li N, Liu X, Li X, Cai H, Pan D, et al. Hormone replacement treatment regimen is associated with a higher risk of hypertensive disorders of pregnancy in women undergoing frozen-thawed embryo transfer. Front Endocrinol (Lausanne). 2023;14:1133978.
Landsverk E, Westvik-Johari K, Romundstad LB, Opdahl S. Birth size after embryo cryopreservation: larger by all measures? Hum Reprod. 2023;38(7):1379–89.
Westvik-Johari K, Romundstad LB, Lawlor DA, Bergh C, Gissler M, Henningsen AA, et al. Separating parental and treatment contributions to perinatal health after fresh and frozen embryo transfer in assisted reproduction: a cohort study with within-sibship analysis. PLoS Med. 2021;18(6):e1003683.
Rosalik K, Carson S, Pilgrim J, Luizzi J, Levy G, Heitmann R, et al. Effects of different frozen embryo transfer regimens on abnormalities of fetal weight: a systematic review and meta-analysis. Hum Reprod Update. 2021;28(1):1–14.
Jauniaux E, Hussein AM, Elbarmelgy RM, Elbarmelgy RA, Burton GJ. Failure of placental detachment in accreta placentation is associated with excessive fibrinoid deposition at the utero-placental interface. Am J Obstet Gynecol. 2022;226(2):243-e1- e10.
Jauniaux E, Jurkovic D, Hussein AM, Burton GJ. New insights into the etiopathology of placenta accreta spectrum. Am J Obstet Gynecol. 2022;227(3):384–91.
McNally L, Zhou Y, Robinson JF, Zhao G, Chen LM, Chen H, et al. Up-regulated cytotrophoblast DOCK4 contributes to over-invasion in placenta accreta spectrum. Proc Natl Acad Sci U S A. 2020;117(27):15852–61.
Illsley NP, DaSilva-Arnold SC, Zamudio S, Alvarez M, Al-Khan A. Trophoblast invasion: lessons from abnormally invasive placenta (placenta accreta). Placenta. 2020;102:61–6.
Fitzpatrick KE, Sellers S, Spark P, Kurinczuk JJ, Brocklehurst P, Knight M. Incidence and risk factors for placenta accreta/increta/percreta in the UK: a national case-control study. PLoS ONE. 2012;7(12):e52893.
Salmanian B, Fox KA, Arian SE, Erfani H, Clark SL, Aagaard KM, et al. In vitro fertilization as an independent risk factor for placenta accreta spectrum. Am J Obstet Gynecol. 2020;223(4):568-e1- e5.
Silver RM, Landon MB, Rouse DJ, Leveno KJ, Spong CY, Thom EA, et al. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol. 2006;107(6):1226–32.
Carusi DA, Fox KA, Lyell DJ, Perlman NC, Aalipour S, Einerson BD, et al. Placenta accreta spectrum without placenta previa. Obstet Gynecol. 2020;136(3):458–65.
Larish A, Horst K, Brunton J, Schenone M, Branda M, Mehta R, et al. Focal-occult placenta accreta: a clandestine source of maternal morbidity. Am J Obstet Gynecol MFM. 2023;5(6):100924.
Ishihara O, Araki R, Kuwahara A, Itakura A, Saito H, Adamson GD. Impact of frozen-thawed single-blastocyst transfer on maternal and neonatal outcome: an analysis of 277,042 single-embryo transfer cycles from 2008 to 2010 in Japan. Fertil Steril. 2014;101(1):128–33.
Kaser DJ, Melamed A, Bormann CL, Myers DE, Missmer SA, Walsh BW, et al. Cryopreserved embryo transfer is an independent risk factor for placenta accreta. Fertil Steril. 2015;103(5):1176-1184 e2.
Carusi DA, Gopal D, Cabral HJ, Racowsky C, Stern JE. A risk factor profile for placenta accreta spectrum in pregnancies conceived with assisted reproductive technology. F S Rep. 2023;4(3):279–85.
Saito K, Kuwahara A, Ishikawa T, Morisaki N, Miyado M, Miyado K, et al. Endometrial preparation methods for frozen-thawed embryo transfer are associated with altered risks of hypertensive disorders of pregnancy, placenta accreta, and gestational diabetes mellitus. Hum Reprod. 2019;34(8):1567–75.
Sakai Y, Ono M, Iizuka T, Kagami K, Masumoto S, Nakayama M, et al. Embryo transfer associated with hormone replacement therapy cycles using assisted reproductive technology increases placenta accreta spectrum. J Obstet Gynaecol Res. 2019;45(12):2394–9.
Takeshima K, Ezoe K, Onogi S, Kawasaki N, Hayashi H, Kuroda T, et al. Endometrial preparation and maternal and obstetrical outcomes after frozen blastocyst transfer. AJOG Glob Rep. 2022;2(4):100081.
Tao Y, Kuang Y, Wang N. Risks of placenta previa and hypertensive disorders of pregnancy are associated with endometrial preparation methods in frozen-thawed embryo transfers. Front Med (Lausanne). 2021;8:646220.
Tanaka H, Tanaka K, Osato K, Kusaka H, Maegawa Y, Taniguchi H, et al. Evaluation of maternal and neonatal outcomes of assisted reproduction technology: a retrospective cohort study. Medicina (Kaunas). 2020;56(1):32.
Al-Khatib A, Sagot P, Cottenet J, Aroun M, Quantin C, Desplanches T. Major postpartum haemorrhage after frozen embryo transfer: a population-based study. BJOG. 2024;131(3):300–8
Taniguchi M, Akinaga C, Suzuki K, Tarui K, Tamura N, Shiko Y, et al. The effect of assisted reproductive technology on postpartum bleeding: hormonal cycle frozen embryo transfer might increase blood loss. J Anesth. 2024;38(1):19–28.
Sugai S, Yamawaki K, Sekizuka T, Haino K, Yoshihara K, Nishijima K. Pathologically diagnosed placenta accreta spectrum without placenta previa: a systematic review and meta-analysis. Am J Obstet Gynecol MFM. 2023;5(8):101027.
Stuart JJ, Gray KJ, Rich-Edwards JW, Roberts J. Epidemiology of hypertensive disorders of pregnancy. In: Taylor RN, Conrad KP, Davidge ST, Staff AC, Roberts JM, editors. Chesley’s hypertensive disorders of pregnancy. 5th ed. San Diego, CA: Elsevier; 2022. p. 21–44.
Moreno-Sepulveda J, Checa MA. Risk of adverse perinatal outcomes after oocyte donation: a systematic review and meta-analysis. J Assist Reprod Genet. 2019;36(10):2017–37.
Salha O, Sharma V, Dada T, Nugent D, Rutherford AJ, Tomlinson AJ, et al. The influence of donated gametes on the incidence of hypertensive disorders of pregnancy. Hum Reprod. 1999;14(9):2268–73.
Wang Z, Zhang Y, Shang X, Miao R, Yin M, Yang H, et al. The likelihood of a healthy live birth after frozen embryo transfer with endometrium prepared by natural ovulation regimen vs. programmed regimen: a propensity-score matching study. AJOG Glob Rep. 2023;3(2):100210.
Frisell T. Invited commentary: sibling-comparison designs, are they worth the effort? Am J Epidemiol. 2021;190(5):738–41.
Gu F, Wu Y, Tan M, Hu R, Chen Y, Li X, et al. Programmed frozen embryo transfer cycle increased risk of hypertensive disorders of pregnancy: a multicenter cohort study in ovulatory women. Am J Obstet Gynecol MFM. 2023;5(1):100752.
Barberet J, Romain G, Binquet C, Guilleman M, Bruno C, Ginod P, et al. Do frozen embryo transfers modify the epigenetic control of imprinted genes and transposable elements in newborns compared with fresh embryo transfers and natural conceptions? Fertil Steril. 2021;116(6):1468–80.
Velker BA, Denomme MM, Mann MR. Embryo culture and epigenetics. Methods Mol Biol. 2012;912:399–421.
Mani S, Ghosh J, Rhon-Calderon EA, Lan Y, Ord T, Kalliora C, et al. Embryo cryopreservation leads to sex-specific DNA methylation perturbations in both human and mouse placentas. Hum Mol Genet. 2022;31(22):3855–72.
Scherrer U, Rimoldi SF, Rexhaj E, Stuber T, Duplain H, Garcin S, et al. Systemic and pulmonary vascular dysfunction in children conceived by assisted reproductive technologies. Circulation. 2012;125(15):1890–6.
Meister TA, Rimoldi SF, Soria R, von Arx R, Messerli FH, Sartori C, et al. Association of assisted reproductive technologies with arterial hypertension during adolescence. J Am Coll Cardiol. 2018;72(11):1267–74.
Ginstrom Ernstad E, Wennerholm UB, Khatibi A, Petzold M, Bergh C. Neonatal and maternal outcome after frozen embryo transfer: increased risks in programmed cycles. Am J Obstet Gynecol. 2019;221(2):126 e1-e18.
Waschkies F, Kroning L, Schill T, Chandra A, Schippert C, Topfer D, et al. Pregnancy outcomes after frozen-thawed embryo transfer in the absence of a corpus luteum. Front Med (Lausanne). 2021;8:727753.
Epelboin S, Labrosse J, De Mouzon J, Devaux A, Gervoise-Boyer MJ, Hesters L, et al. Higher risk of pre-eclampsia and other vascular disorders with artificial cycle for frozen-thawed embryo transfer compared to ovulatory cycle or to fresh embryo transfer following in vitro fertilization. Front Endocrinol (Lausanne). 2023;14:1182148.
Zhou R, Zhang X, Huang L, Wang S, Li L, Dong M, et al. The impact of different cycle regimens on birth weight of singletons in frozen-thawed embryo transfer cycles of ovulatory women. Fertil Steril. 2022;117(3):573–82.
Esh-Broder E, Ariel I, Abas-Bashir N, Bdolah Y, Celnikier DH. Placenta accreta is associated with IVF pregnancies: a retrospective chart review. BJOG. 2011;118(9):1084–9.
Hayashi M, Nakai A, Satoh S, Matsuda Y. Adverse obstetric and perinatal outcomes of singleton pregnancies may be related to maternal factors associated with infertility rather than the type of assisted reproductive technology procedure used. Fertil Steril. 2012;98(4):922–8.
Zhu L, Zhang Y, Liu Y, Zhang R, Wu Y, Huang Y, et al. Maternal and live-birth outcomes of pregnancies following assisted reproductive technology: a retrospective cohort study. Sci Rep. 2016;6:35141.
Nagata C, Yang L, Yamamoto-Hanada K, Mezawa H, Ayabe T, Ishizuka K, et al. Complications and adverse outcomes in pregnancy and childbirth among women who conceived by assisted reproductive technologies: a nationwide birth cohort study of Japan environment and children’s study. BMC Pregnancy Childbirth. 2019;19(1):77.
Modest AM, Toth TL, Johnson KM, Shainker SA. Placenta accreta spectrum: in vitro fertilization and non-in vitro fertilization and placenta accreta spectrum in a Massachusetts cohort. Am J Perinatol. 2021;38(14):1533–9.
Funding
Investigations by KPC, VLB, and FVH were supported, in part, by a grant from the National Institutes of Health P01 HD065647: KPC Program Director/Principal Investigator, University of Florida; VLB Principal Investigator, Stanford University; FVH was also underwritten by a grant from the German Research Foundation DFG project number 273703678. VLB is currently supported by funding from the National Institutes of Health R01 HD100341 to study frozen embryo transfer protocols and FVH by DFG project number 507276351 to study decidualization.
Ethics declarations
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
The authors consent for publication.
Competing interests
KPC holds use patents for relaxin.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Dedication
We dedicate this work to Robert N. Taylor MD, PhD—colleague, friend and mentor. His exceptional intelligence, kindness, generosity and humility will never be forgotten.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Conrad, K.P., von Versen-Höynck, F. & Baker, V.L. Pathologic maternal and neonatal outcomes associated with programmed embryo transfer. J Assist Reprod Genet 41, 821–842 (2024). https://doi.org/10.1007/s10815-024-03041-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-024-03041-9