Abstract
Background
Merkel cell carcinoma (MCC) is an unusual primary neuroendocrine carcinoma of the skin. MCC is a fatal disease, and patients have a poor chance of survival. Moreover, MCC lacks distinguishing clinical features, and thus by the time the diagnosis is made, the tumour usually have metastasized. MCC mainly affects sun-exposed areas of elderly persons. Half of the tumours are located in the head and neck region.
Methods
MCC was first described in 1972. Since then, most of the cases reported, have been in small series of patients. Most of the reports concern single cases or epidemiological studies. The present study reviews the world literature on MCC. The purpose of this article is to shed light on this unknown neuroendocrine carcinoma and provide the latest information on prognostic markers and treatment options.
Results
The epidemiological studies have revealed that large tumour size, male sex, truncal site, nodal/distant disease at presentation, and duration of disease before presentation, are poor prognostic factors. The recommended initial treatment is extensive local excision. Adjuvant radiation therapy has recently been shown to improve survival. Thus far, no chemotherapy protocol have achieved the same objective.
Conclusion
Although rare, the fatality of this malignancy makes is important to understand the etiology and pathophysiology. During the last few years, the research on MCC has produced prognostic markers, which can be translated into clinical patient care.
Similar content being viewed by others
Background
The Merkel cell
The Merkel cell (MC) was first described by the German histopathologist Friedrich Sigmund Merkel in his classic article published in 1875: Merkel F: "Tastzellen und Tastkörperchen bei den Haustieren und beim Menschen" [1]. He demonstrated the existence of touch cells in the snout skin of pigs, calling them "Tastzellen" because of their putative function in the touch sensation. Merkel postulated that the cells acted as mechanoreceptors in all animals.
Distribution of Merkel cells
MCs are normal constituents of the basal layer of the epidermis and the follicular epithelium [2] (Figure 1). They are scarce in normal skin, but are present in high numbers and form clusters in areas of sensory perception. In close association with primary nerve endings in the skin, they form the MC-axon complex.
On light microscopy, MCs are large, oval, amphophilic, clear cells situated in the basal or suprabasal layer of the epidermis. They are not easily distinguished from other nonkeratinocytic epidermal cells, e.g. melanocytes and Langerhans cells, by light microscopic immunohistochemistry. Special techniques such as immunohistochemistry, electron microscopy or transmission electron microscopy are therefore required for their identification.
Function in developing embryo and adult
In human development, MCs can be detected in the epidermis in the 8th gestational week [3]. In the developing embryo, MCs are thought to be involved in the formation of the subepidermal nerve plexus [4, 5], and in the formation and proliferation of eccrine sweat glands and hair follicles [6]. In the adult MCs are thought to act as slow acting type-I mechanoreceptors. Together with sensory nerve endings, they form MC-axon complexes that are activated by steady skin indentation [7]. The function of MCs in this complex is, however, enigmatic. Two possible functions have been proposed: either they may act as attracters of developing or regenerating type I nerve fibres [8] or they may have neuromodulatory or neuroregulatory functions in the basal epidermis, such as keratinocyte proliferation stimulation, maintenance of the differentiation of keratinocytes, or the release of bioactive substances to subepidermal structures [9].
Origin of the Merkel cell
The origin of the MC is still controversial. The cell may derive either from the epithelial cells of the epidermis or from the neural crest migrating to the epidermis during embryogenesis. In the 1980s and 1990s, the epidermal origin from keratinocytes with an aberrant differentiation [10] was the prevailing hypothesis [3, 11–13], as suggested by the epidermal location of the MC, the expression of cytokeratins and the results of skin transplantation experiments [14, 15]. Recent studies, however, have provided strong evidence in support of the neural crest origin [16, 17].
Merkel cell carcinoma
The Merkel cell carcinoma (MCC) was first described in 1972, when Toker presented the first five cases under the name "trabecular carcinoma of the skin", assuming them to represent an eccrine, sweat gland-derived carcinoma [18]. In electron microscopic (EM) studies, Tang and Toker later identified dense-core neuroendocrine granules within the tumour cells, thus demonstrating their origin from MCs [19].
The "cell of origin" of MCC is, however, still speculative. There are morphological and biological similarities between the MC and MCC. The common presence of neuroendocrine granules [20] and the positive immunostaining for cytokeratin-20 (CK-20), for instance, provide evidence for MC origin [21], although this may indicate differentiation rather than origin. However, certain differences also exist between the MC and MCC, such as the fibrous whorls and neurofilaments that are seen in MCC but not in normal MCs. Another argument against the MC as the cell of origin for MCC is that mitoses have not been detected in human MCs [3, 22]. There is a contradiction between the location of the cell in the skin in MCs and in MCC, the tumour practically always involves the dermis, sparing the epidermal structures.
Toker called the first five cases of MCC "trabecular carcinoma of the skin." This name derived from the trabecular architecture of the tumour, which is the most characteristic, but the uncommon, configuration of three histological patterns. Over the years, the name of this tumour has been the subject of lively discussion. Several names and synonyms have been proposed; either based on histological features or derived from the term "Merkel cell". These include derivatives such as "Malignant Merkel-cell tumour" [23], "Merkel cell tumour" [24] or "Merkel cell tumour of the skin" [25]. It was not until the mid 1980s that the term "Merkel cell carcinoma" was established. In the year 1980, Johannessen and co-workers seem to have used this term for the first time [26]. The term "Primary neuroendocrine carcinoma of the skin" was coined to reflect the pathophysiology of the disease.
Histology
The histology of MCC is typical of small round blue cell tumours, an entity that includes a wide variety of highly malignant tumours: the Ewing family of tumours, olfactory neuroblastoma (esthesioblastoma), rhabdomyosarcoma, neuroblastoma, lymphoma, desmoplastic small cell tumour, osteosarcoma, small cell lung carcinoma (SCLC), small cell melanoma and mesenchymal chondrosarcoma [27, 28].
Histologically, MCC can be classified into three distinct subtypes [29–31]. In haematoxylin-eosin staining, typical histology of the MCC is small blue cells with sparse cytoplasm. Nuclei are medium-sized. Mitoses are abundantly and the tumour expands frequently to subcutaneous tissue. Chromatin is displayed in typical salt and pepper pattern.
The classification to the subtypes is usually reserved for the anatomical studies. The first of these is the trabecular subtype, described originally by Toker[18]. This is the least frequent histological pattern. Cells are arranged in distinctly organoid clusters and trabeculae with occasional ribbons. This type of tumour usually occurs adjacent to adnexal structures, particularly hair follicles.
The intermediate subtype is the most frequent histological subtype [32]. It exhibits a solid and diffuse growth pattern. Cells are less compactly arranged, and the cytoplasm is less abundant than in the trabecular type. Mitoses and focal areas of necrosis are frequent. These tumours usually arise adjacent to adnexa, but may invade the epidermis. The clinical behaviour is more aggressive than that of tumours of the trabecular type. The small cell type mimics small cell tumours of other sites, e.g. SCLC [33]. The tumours arise in the dermis and appear as solid sheets and clusters of cells. The clinical behaviour of this subtype appears to be as similar as the small cell tumours of other origins.
Diagnosis
Diagnosis is based on typical histology representation on haematoxylin-eosin -stained slides together with the results of immunohistochemistry [32]. A typical histological finding in MCC is the presence of tumour tissue within the dermis with repeated extensions to underlying subcutaneous tissue (Figure 2). The epidermis, papillary dermis and adnexal structures are not usually involved. Cytological features include sparse cytoplasm with uniform, monotonous medium-sized nuclei and abundant mitoses [34]. All these cytomorphological features can be present as well in fine needle aspirates [35]. EM studies show that the ultrastructure of neuroendocrine granules of the tumour is similar to that of normal MCs. The most consistent findings are the aggregation of intermediate filaments in a paranuclear location and the existence of membrane-bound dense core granules. Only 10 % of all MCC tumours are intraepidermal [36].
Immunohistochemical staining of primary Merkel cell carcinoma for differential diagnosis and neuroendocrine differentiation. A. Hematoxylin-eosin staining, the tumour cells have round nuclei, original magnification 200×. B. Positive cytokeratin-20 staining, showing typical punctate pattern of immunostaining, original magnification 400×. C. Negative staining for Thyroid-transcriptor factor-1, original magnification 400×. D. chromogranin -A staining, original magnification 400× and E. synaptophysin staining, original magnification 400×.
Immunohistochemistry – differentiation
The tumour expresses both epithelial and neuroendocrine markers, and thus exhibits both epithelial and neuroendocrine differentiation.
Epithelial differentiation
Of the intermediate filaments, MCC expresses low-molecular-weight cytokeratins (keratins 8,18,19 and 20), the simple epithelial type being the most marked [20, 37]. The most important keratin in differential diagnostics is cytokeratin-20 (CK-20). CK-20 is a low-molecular-weight cytokeratin, in normal tissues it is only expressed in the gastrointestinal epithelium, urothelium, and MCs [38]. It has been shown that CK-20-positivity in MCC serves to distinguish it from pulmonary small cell carcinoma. Considered a sensitive and specific marker for MCC, CK-20 is helpful in efforts to distinguish between MCC and other malignant neoplasms, since it is not usually expressed in neuroendocrine carcinomas of other sites, such as SCLC [39, 40] (Figure 2). Although up to 30 % of metastatic neuroendocrine carcinoma from lung might stain for CK-20, but they always stain for TTF-1, which is negative in MCC [41]. In some 5 – 25% of MCC cases, CK-20 is negative [42, 43].
Tissue-specific transcription factors control cell determination and differentiation. Thyroid transcription factor 1 (TTF-1) is a tissue specific transcription factor expressed in epithelial cells of the thyroid and lung, as well as in certain areas of the brain [44]. TTF-1 is employed to differentiate between MCC and small-cell tumours [45, 46], MCC is negative for TTF-1 [47] (Figure 2).
Combining TTF-1 with CK-20 provides a sound basis for diagnosis. Most adenocarcinomas from other sites (breast, lung, endometrium) and neuroendocrine carcinomas such as SCLC are essentially negative for CK-20 [40] while most are negative for CK-20, those from the lung are postitive for TTF-1. Table 1 presents the immunohistochemistry for the differentiation diagnosis of MCC.
Neuroendocrine differentiation
Due to neuroendocrine differentiation, MCC always stains positively for neuron-specific enolase (NSE), which is a general marker of neuroendocrine tumours [48–50]. CD56, or neural cell adhesion molecule (NCAM), has recently been demonstrated to be a neuroendocrine marker of the pulmonary neuroendocrine cell system as well as MCC [51, 52]. Although, McNiff and co-workers recently reminded of the pitfalls in using CD56 marker for MCC diagnosis [53] Chromogranin A (CrA), a member of the chromogranin family, is a major protein that accounts for a large amount of the soluble matrix of neurosecretory granules. First isolated from chromaffin cells of the adrenal medulla, CrA is the most widely distributed marker of endocrine tumours [54]. MCC shows a focal, positive immunoreaction to CrA [55, 56] (Figure 2). Synaptophysin is a transmembrane channel protein of small presynaptic vesicles. It is expressed in neuroendocrine and neural cells and diffusely in neuroendocrine system cells [57, 58]. Both primary and metastatic neuroendocrine carcinomas are habitually synaptophysin positive [59, 60]. MCC consistently shows positive immunoreactions to synaptophysin [56, 61] (Figure 2).
Newer markers of neuroendocrine differentiation introduced for MCC are the microtubule-associated proteins (MAPs). These are the major component of the cytoskeleton family of proteins associated with the microtubule assembly of the central and peripheral nervous system [62, 63]. Specific MAPs have been identified in specific cell types. MAP-2, for instance, is a highly sensitive and specific marker of neuroendocrine differentiation [62–64]. Liu et al, demonstrated MAP-2 expression in all MCC samples, even though CK-20 staining was negative [65]. In general, MCC shows a high degree of neuroendocrine differentiation. A higher expression of CrA and synaptophysin associated with more indolent behaviour [56].
DNA copy number changes
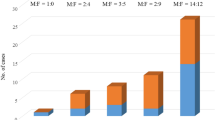
Different types of chromosomal irregularities have been documented in MCC tumours and cell lines [66–68]. The most common aberrations engage chromosomes 1, 6, 11 and 13. Trisomy of chromosome 6 is a widely considered as recurrent aberration [69, 70]. Trisomy of chromosome 1 appears to be typical of MCC [71]. In the chromosome 11 a partial trisomy has been documented [72] as well as complete trisomy [73]. In chromosome 13 loss was recognizable [72] in addition to LOH [74]. So far it seems that high-copy number amplifications for chromosomal subregions are a rare event in MCC [75]. Although DNA copy number changes have not been established as prognostic factor for MCC, primary tumours expressing DNA alterations were predominantly distinguished in large sized tumours, and risk of metastatic dissemination was three-fold compared to tumours with no DNA alterations [76].
Clinical presentation and staging
The clinical presentation of this tumour is rather non-specific. MCC is usually, at least at early stages of the disease, defined as a small painless erythematous intradermal mass, usually with no ulceration [77, 78]. Especially small tumours in particular can appear somewhat benign, whereas large tumours have an unquestionably malignant appearance. Because of the rare nature of this neoplasm, it is often mistaken for more common skin tumours of epithelial origin. Most common presumptive clinical diagnosis is cyst.
There is no classification scheme for MCC such as there is for most carcinomas or sarcomas. At present, staging of most malignant tumours is based on the T(umour) N(odes) M(etastasis) classification (TNM classification of malignant tumours – 6th edition, 2002). Concerning the skin malignancies the TNM classification applies to carcinomas of the skin in general and malignant melanoma. In most published series MCC is not classified according to the TNM system.
Yiengpruksawan has, however, proposed a staging system that has been widely recognised in the treatment of MCC [77], which is presented in Table 2.
Incidence and clinical behaviour of MCC
The reported annual incidence of MCC ranges from 0.2 to 0.45 per 100 000 [79, 80]. Incidence has tripled since 1986:1986 0.15 per 100,000 and 2001 0.44 per 100,000 [81]. It is 100 times as rare as melanoma [82]. MCC is principally a disease of the Caucasian race. The annual age-adjusted incidence of MCC is 0.23 per 100,000 for whites and 0.01 for blacks [83]. The literature contains only single case reports of black Africans or African-Americans with MCC [84–86]. Both sexes are affected, though earlier studies showed a slight male predominance [87–89]. The number of reported patient series is, however growing, and recent investigations have shown an equal distribution of the sexes or even a minor female prevalence [90–92]. MCC mainly affects the elderly, the mean age at presentation being about 75 years [93, 94]. Age-specific incidence was highest in the elderly, 4.28 per 100,000 in the 85+ age group [81] Only a few cases occur before the age of 50, and is usually related to immunosuppression [95].
MCC usually occurs in sun-damaged skin. The tumours are often found in close proximity to other lesions of actinically damaged skin, for instance, in cases of Bowen disease, squamous cell carcinoma, basal cell carcinoma, solar keratosis and lentigo maligna. The most common site is the head and neck region [96]. Pathogenetic factors such as UV irradiation may contribute to tumour development [68, 97]. Miller and Rabkin have calculated that the incidence of MCC rises along with an increase in potential exposure to solar UVB. They found statistical significance between the incidence of MCC and UVB exposure [83].
The natural history of MCC is variable and dependent on the stage of disease at presentation [98]. Typically MCC has a tendency to progress rapidly, and in just a few months, the tumour may attain a large diameter. Therefore, early diagnosis and surgery are strongly advocated. Several studies established a close correlation between overall survival and tumour size. The overall survival rate is largely influenced by tumour size (≥ 2 cm) [99, 100]. In some studies dense lymphocytic infiltrates have been associated with poor prognosis [101].
The typical clinical course of the disease is rapid progression of the primary tumour with early and frequent metastasis to the regional lymph nodes. The sentinel lymph node biopsy (SLNB) technique has provided information on the metastatic dissemination at the presentation. In a meta-analysis of 60 MCC patients, Mehrany and co-workers detected 33% of the patients having metastatic dissemination in the sentinel lymph node at the presentation [102]. Then again, Hohaus and co-workers in their 17 patients retrospective analysis reported only 3 (18%) of the patients at stage II at the presentation [103]. Allen and co-workers detected 5/26 (19%) of the patients having positive lymph nodes at the presentation [104].
Recurrences are frequent. Allen et al, at the Memorial Sloan-Kettering Cancer Center's identified 251 patients who had been treated between 1970 and 2002. The median time to recurrence was 9 months, and 102 patients (43%) recurred [98]. Primary site on the lower limb had an adverse effect on locoregional recurrencies [105].
Although the natural course of MCC is usually defined with metastatic spread, there are some reports in the literature (10 cases) of spontaneous regression [106, 107]. Mori and co-workers have studied the apoptosis in eight cases of MCC [108] and found high apoptotic rate in MCC samples. Inoue et al have examined the mechanisms behind the spontaneous regression in seven MCC samples [109]. The TUNEL index and number of lymphocytes around the tumour nests was increased in the samples with spontaneous regression, furthermore the majority of the infiltrating lymphocytes were T-cells [109]. They concluded that apoptosis and local T-cell mediated immune response might be involved in spontaneous regression of MCC.
Co-existing malignancies
MCC has been associated with other skin tumours (squamous cell carcinoma, basal cell carcinoma) and haematological (B-cell) malignancies [110–112]. In addition, adenocarcinomas of the breast and ovaries have been shown to have an association with MCC. Co-malignancies, whether they appear before, after or simultaneously with MCC, are associated with higher MCC-specific mortality [113, 114].
Immunosuppression: therapeutic and acquired
The incidence of MCC is abnormally high (8%) among immunosuppressed patients. Such patients are moreover younger, 49% being under the age of 50 [115, 116]. Weakened immunity increases the risk of MCC; HIV patients, for example, have a 13.4 times increased risk of acquiring MCC [117].
Prognosis
The prognosis is rather poor. The 2-year survival rate is 30 – 50% [118, 119], Kokoska included 35 and Linjawi 10 patients in his study. Agelli and Clegg have studied the epidemiology of MCC in the United States in a patient population of 1034 by using Surveillance, Epidemiology, and End Results Program. The 5-year survival rate in their study was 75%, 59% and 25% for localised, regional and distant MCC, respectively [120]. Overall survival (OS) is associated with the stage of disease at presentation. Female sex, localized disease, and younger age were positive predictors of survival [78, 120, 121]. The risk of recurrence or metastasis was 19 times as great in sentinel node biopsy-positive patients as in biopsy-negative patients (p = 0.005) [102].
Local recurrences are frequent, occurring in up to 44% of patients [30, 88, 93]. There have been some reports of lymph node metastasis alone, with no detectable primary tumour [122, 123]. Depending on the length of the follow-up period up to 36% of the patients develop regional lymph node metastasis [124]. Distant dissemination is not infrequent, up to 40–50% of patients developing visceral metastasis [125–127], particularly to the lungs, liver and bone [128, 129].
Surgical treatment
Because of the rarity of the tumour, there is multitude of treatment protocols. However, the surgical treatment seems to be the corner stone of the different treatment protocols.
Early, radical surgery is the recommended procedure for the treatment of primary MCC [92, 130]. Margins of 2 – 5 cm are recommended for better local control. Nevertheless, consensus on the width of margins has not yet been reached. Yiengpruksawan and co-workers, O'Connor and Brodland reported better local control with margins of > 3 cm [77, 131]. Then again, there have been reports that larger free margins confer no advantage on survival [124]. Gillenwater and co-workers had sixty-six head and neck MCC cases included in their study, but only eighteen patient's data was sufficient for the statistical analysis. They state themselves that the small patient population in their study might explain this result. Because lymph node metastases develop in approximately 50% of patients in the course of the disease, some authors recommend prophylactic lymphadenectomy in all patients [97, 118]. Then again, the patient materials are small: Lawenda had nine patient study population and Kokoska 35. Silva and co-workers recommend lymphadenectomy for tumours with 10 or more mitoses per high-power field, in cases of lymphatic invasion, or when tumours are composed of small cells, that is, the small-cell subtype [132].
According to the literature on MCC, the sentinel lymphnode biopsy (SLNB) technique was used in approximately 100 cases between 1976 and 2002. Most reports advocate SLNB because morbidity is low, and because it provides an easy and reliable way of locating occult metastasis [102, 133, 134]. Recent studies have investigated the efficacy of SLNB in helping to determine whether lymph basin evacuation is necessary. These studies have been conducted on only a small series of patients, but even so, the results suggest that a negative sentinel node may obviate the need for neck dissection. SLNB is strongly advocated in the treatment and staging of individual tumours. Its use will improve the accrual of patients to adjuvant and further surgical treatment protocols [102, 135]. Especially for the MCC cases occurring in the head and neck region the SLNB seems to be a safe and reliable technique for regional staging [136].
It is widely accepted that patients with regional node metastases or local or regional recurrence should undergo excision of the primary lesion and lymph node dissection [130]. Adjuvant radiation therapy to the primary site and regional nodes is generally recommended in addition to lymph node dissection. Tumours arising in the head and neck region with parotid gland metastasis seem to have even poorer prognosis [137]. As a result elective lymph node dissection has been recommended for younger patients with large tumours or tumours of the head and neck region [138–140].
Mohs micrographic surgery is a surgical technique developed by Frederick Mohs in the 1930s at the university of Wisconsin [141]. Briefly, the technique consists of debulking the tumour with a semisharp curette, in order to outline the skin tumour. Subsequently, a scalpel is used to remove the tissue in a horizontal fashion with 2 mm clinical margins. The tissue sample is taken to the laboratory for the processing. The patient is bandaged and waiting for the microscopic results. The horizontal frozen sections are cut from the undersurface of the tissue parallel to the skin surface, rather than vertically. This method allows for microscopic examination of the entire deep and peripheral margins of the surgical specimen. The surgeon does the microscopic examination. These steps are then repeated until the margins are free from the tumour, and the defect is closed.
Mohs micrographic surgery has been recommended as an advanced technique for local control, especially in areas calling for excellent cosmetic results (i.e. head and neck region) without compromising the principles of cancer surgery [142, 143]. Then again, Brissett and co-workers reported inferior 2-year survival with patients undergoing Mohs micrographic surgery compared to patients who had wide local excision alone or wide local excision and lymphnode basin evacuation, 33%, 68% and 100% respectively [130].
Oncological treatment
Chemotherapy is generally reserved for stage III (distant metastasis) cases of MCC. The carcinoma has often been shown to respond to chemotherapy but, as in SCLC, remission is brief. Recently, Waldman and co-workers reported a complete remission that lasted for 6 months. The remission was achieved through the use of high-dose polychemotherapy following autologous blood stem cell transplantation [144]. Some months previously, Voog et al reported similar results, the rates of response to second-line (n = 33) and third-line (n = 10) chemotherapy being 45% and 20%, respectively [145]. No chemotherapeutic protocol has, however, been able to achieve a significant increase in survival rate [105].
No standard chemotherapy protocol has yet been established for the treatment of MCC. Because of the morphological and immunohistochemical similarity of MCC to SCLC, chemotherapy has been performed with protocols based largely on agents active in SCLC. A wide variety of chemotherapeutic agents, including the cytostatic drugs cyclophosphamide, doxorubicin, epirubicin, vincristine, etoposide, cisplatine, carboplastin, 5-fluorouracil, dacarbazine, mitoxantrone, bleomycine and iphosphamide, have been discussed [87, 96, 145–147]. Unfortunately, reports to date consist of only small studies and anecdotal evidence. A few reports have shown markedly high mortality among MCC patients receiving chemotherapy for metastatic disease. Tai and co-workers reported seven (3.4%) toxic deaths among 204 cases [96]. Voog and co-workers gave even higher mortality, the rate of toxic death during first-line treatment being 7.7% in 101 patients [145].
MCC is a highly radiosensitive tumour, which has been demonstrated in in vitro studies [148]. Many authors have recommended post-operative radiotherapy based on the retrospective comparison of patients treated with surgery alone with patients treated with surgery and post-operative radiotherapy [149, 150]. In a recent series of 37 MCC patients Veness et al. reported a significantly longer median disease free survival with patients treated with surgery and adjuvant radiotherapy and than those undergoing surgery alone (23 months vs. 6 months) [151]. Moreover, outcome improved markedly in patients receiving adjuvant radiotherapy after surgery [152]. Radiation is most commonly used as an adjuvant therapy after surgery but it may be used to as the only treatment especially in patients who are too weak to undergo surgical treatments [153, 154]
Conclusion
Recent advances in the research of MCC have revealed features in the natural biology of this malignancy. However, several questions regarding the biology and pathology of the tumour remain to be addressed. The molecular events leading to oncogenic alterations must be identified. Mechanisms of metastasis are still largely concealed. Revealing these biological properties, hopefully, will lead to discovery of new treatments, e.g. the role of anti-angiogenic medication is still uncertain. Of the surgical treatments, the sentinel lymph node biopsy has proven its efficacy in finding the clinically occult metastasis and accrual of patients to adjuvant and further surgical and oncological treatment protocols.
Several markers for prognosis have been studied, but none have proven its value like large, ≥ 2 cm, primary tumour size. The wide range of the factors associated to survival may reflect the absence of large institutional studies.
References
Merkel F: Tastzellen und Tastkörperchen bei den Haustieren und beim Menschen. Arkiv für Mikroskopische Anatomie und Entwicklungsmechanik. 1875, 11: 636-652.
Briggaman RA, Wheeler CEJ: The epidermal-dermal junction. J Invest Dermatol. 1975, 65: 71-84. 10.1111/1523-1747.ep12598050.
Moll I, Zieger W, Schmelz M: Proliferative Merkel cells were not detected in human skin. Arch Dermatol Res. 1996, 288: 184-187. 10.1007/s004030050044.
Narisawa Y, Hashimoto K, Nihei Y, Pietruk T: Biological significanse of dermal Merkel cells in development of cutaneus nerves in the human fetal skin. Journal of Histochemistry & Cutochemistry. 1992, 40: 65-71.
Vos P, Starck F, Pittman RN: Merkel cells in vitro: production of nerve growht factor and selective interactions with sensory neuros. Developmental Biology. 1991, 144: 281-300. 10.1016/0012-1606(91)90422-Y.
Kim DK, Holbrook KA: The appearance, density, and distributin of Merkel cells in human embryonic and fetal skin: their relation to sweat gland and hair follicle development. The Journal of Investigative Dermatology. 1995, 104: 411-416. 10.1111/1523-1747.ep12665903.
Ogawa H: The Merkel cell as a possible mechanoreceptor cell. Prog Neurobiol. 1996, 49: 317-334.
He L, Tuckett RP, English KB: Chemosensitivity of the rat type I slowly adapting mechanoreceptor. Biol Signals Receptors. 1999, 8: 382-389. 10.1159/000014612.
Tachibana T: The Merkel cell: recent findings and unresolved problems. Arch Histol Cytol. 1995, 58: 379-396.
Heim S, Mitelman F: Cancer Cytogenetics. 1995, New York, Wiley-Liss, 2nd:
Compton CC, Regauer S, Seiler GR, Landry DB: Human Merkel cell regeneration in skin derived from cultured keratinocyte grafts. Laboratory Investigation. 1990, 63: 233-241.
Moll I, Moll R, Franke WW: Formation of epidermal and dermal Merkel cells during human fetal skin development. The Journal of Investigative Dermatology. 1986, 87: 779-789. 10.1111/1523-1747.ep12458993.
Frigerio B, Capella C, Eusebi V, Tenti P, Azzobardi JG: Merkel cell carcinoma of the skin: the structure and origin of normal Merkel cells. Histopathology. 1983, 7: 229-240.
English KB, Burgess PR, Kavka-Van Norman D: Development of rat Merkel cells. J Comp Neurol. 1980, 194: 475-496. 10.1002/cne.901940212.
Lyne AG, Hollis DE: Merkel cells in sheep epidermis during fetal development. J Ultrastruct Res. 1971, 34: 464-472. 10.1016/S0022-5320(71)80059-X.
Grim M, Halata Z: Developmental origin of avian Merkel cells. Anatomy and Embryology. 2000, 202: 410-410. 10.1007/s004290000121.
Szeder V, Grim M, Halata Z, Sieber-Blum M: Neural crest origin of mammalian Merkel cells. Dev Biol. 2003, 253: 258-263. 10.1016/S0012-1606(02)00015-5.
Toker C: Trabecular Carcinoma of the Skin. Arch Derm. 1972, 105: 107 -1110. 10.1001/archderm.105.1.107.
Tang CK, Toker C: Trabecular Carcinoma of the SkinAn Ultrastructural Study. Cancer. 1978, 42: 2311 -22321.
Miettinen M, Lehto VP, Virtanen I, Asko-Seljavaara S, Pitkanen J, Dahl D: Neuroendocrine carcinoma of the skin (Merkel cell carcinoma): ultrastructural and immunohistochemical demonstration of neurofilaments. Ultrastruct Pathol. 1983, 4: 219-225.
Sadahira Y, Nakamoto S, Mori M, Hsueh CL, Awai M: Merkel cell tumor coexpressing cytokeratin and neurofilament proteins. Acta Pathol Jpn. 1987, 37: 331-337.
Vaigot P, Pisani A, Darmon YM, Ortonne JP: The majority of epidermal Merkel cells are non-proliferative: a quantitative immunofluorescence analysis. Acta Derm Venereol. 1987, 67: 517-520.
Rywlin AM: Malignant Merkel-cell tumor is a more accurate description than trabecular carcinoma. Am J Dermatopathol. 1982, 4: 513-515.
Fetissof F, Arbeille-Brassart B, Colombat P, Lorette G, Monegier du Sorbier C, Jobard P: [Merkel cell tumor]. Ann Pathol. 1983, 3: 285-291.
Cremer H, Totovic V: [Merkel cell tumor of the skin. Light and electron microscopic study of 5 cases]. Pathologe. 1983, 4: 287-293.
Johannessen JV, Gould VE: Neuroendocrine skin carcinoma associated with calcitonin production: a Merkel cell carcinoma?. Hum Pathol. 1980, 11: 586-588.
Tarkkanen M, Knuutila S: The diagnostic use of cytogenetic and molecular genetic techniques in the assessment of small round cell tumours. Current Diagnostic Pathology. 2002, 8: 338-348. 10.1016/S0968-6053(02)90135-3.
Pisick E, Skarin AT, Salgia R: Recent advances in the molecular biology, diagnosis and novel therapies for various small blue cell tumors. Anticancer Res. 2003, 23: 3379-3396.
Ratner D, Nelson BR, Brown MD, Johnson T: Merkel Cell Carcinoma. Journal of the American Academy of Dermatology. 1993, 29: 143 -1156.
Haag ML, Glass LF, Fenske NA: Merkel cell carcinoma. Diagnosis and treatment. Dermatol Surg. 1995, 21: 669-683. 10.1016/1076-0512(95)97513-6.
Gould VE, Moll R, Moll I, Lee I, Franke WW: Neuroendocrine (Merkel) cells of the skin: hyperplasias, dysplasias, and neoplasms. Lab Invest. 1985, 52: 334-353.
Johansson L, Tennvall J, Akerman M: Immunohistochemical examination of 25 cases of Merkel cell carcinoma: a comparison with small cell carcinoma of the lung and oesophagus, and a review of the literature. Apmis. 1990, 98: 741-752.
Schmidt U, Muller U, Metz KA, Leder LD: Cytokeratin and neurofilament protein staining in Merkel cell carcinoma of the small cell type and small cell carcinoma of the lung. Am J Dermatopathol. 1998, 20: 346-351. 10.1097/00000372-199808000-00004.
Warner TF, Uno H, Hafez GR, Burgess J, Bolles C, Lloyd RV, Oka M: Merkel cells and Merkel cell tumors. Ultrastructure, immunocytochemistry and review of the literature. Cancer. 1983, 52: 238-245.
Skoog L, Schmitt FC, Tani E: Neuroendocrine (Merkel-cell) carcinoma of the skin: immunocytochemical and cytomorphologic analysis on fine-needle aspirates. Diagn Cytopathol. 1990, 6: 53-57.
Brown HA, Sawyer DM, Woo T: Intraepidermal Merkel cell carcinoma with no dermal involment. American Journal of Dermapathology. 2000, 22: 65-69. 10.1097/00000372-200002000-00013.
Moll R, Osborn M, Hartschuh W, Moll I, Mahrle G, Weber K: Variability of expression and arrangement of cytokeratin and neurofilaments in cutaneous neuroendocrine carcinomas (Merkel cell tumors): immunocytochemical and biochemical analysis of twelve cases. Ultrastruct Pathol. 1986, 10: 473-495.
Miettinen M: Keratin 20: immunohistochemical marker for gastrointestinal, urothelial, and Merkel cell carcinomas. Mod Pathol. 1995, 8: 384-388.
Scott MP, Helm KF: Cytokeratin 20: a marker for diagnosing Merkel cell carcinoma. Am J Dermatopathol. 1999, 21: 16-20. 10.1097/00000372-199902000-00003.
Moll R, Lowe A, Laufer J, Franke WW: Cytokeratin 20 in human carcinomas. A new histodiagnostic marker detected by monoclonal antibodies. Am J Pathol. 1992, 140: 427-447.
Hanly AJ, Elgart GW, Jorda M, Smith J, Nadji M: Analysis of thyroid transcription factor-1 and cytokeratin 20 separates merkel cell carcinoma from small cell carcinoma of lung. J Cutan Pathol. 2000, 27: 118-120. 10.1034/j.1600-0560.2000.027003118.x.
Chan JK, Suster S, Wenig BM, Tsang WY, Chan JB, Lau AL: Cytokeratin 20 immunoreactivity distinguishes Merkel cell (primary cutaneous neuroendocrine) carcinomas and salivary gland small cell carcinomas from small cell carcinomas of various sites. Am J Surg Pathol. 1997, 21: 226-234. 10.1097/00000478-199702000-00014.
Barrett AW, Cort EM, Patel P, Berkovitz BK: An immunohistological study of cytokeratin 20 in human and mammalian oral epithelium. Arch Oral Biol. 2000, 45: 879-887. 10.1016/S0003-9969(00)00050-9.
Lazzaro D, Price M, de Felice M, Di Lauro R: The transcription factor TTF-1 is expressed at the onset of thyroid and lung morphogenesis and in restricted regions of the foetal brain. Development. 1991, 113: 1093-1104.
Byrd-Gloster AL, Khoor A, Glass LF, Messina JL, Whitsett JA, Livingston SK, Cagle PT: Differential expression of thyroid transcription factor 1 in small cell lung carcinoma and Merkel cell tumor. Hum Pathol. 2000, 31: 58-62. 10.1016/S0046-8177(00)80199-9.
Cheuk W, Kwan MY, Suster S, Chan JK: Immunostaining for thyroid transcription factor 1 and cytokeratin 20 aids the distinction of small cell carcinoma from Merkel cell carcinoma, but not pulmonary from extrapulmonary small cell carcinomas. Arch Pathol Lab Med. 2001, 125: 228-231.
Ordonez NG: Value of thyroid transcription factor-1 immunostaining in distinguishing small cell lung carcinomas from other small cell carcinomas. Am J Surg Pathol. 2000, 24: 1217-1223.
Metz KA, Jacob M, Schmidt U, Steuhl KP, Leder LD: Merkel cell carcinoma of the eyelid: histological and immunohistochemical features with special respect to differential diagnosis. Graefes Arch Clin Exp Ophthalmol. 1998, 236: 561-566. 10.1007/s004170050121.
Leong AS, Phillips GE, Pieterse AS, Milios J: Criteria for the diagnosis of primary endocrine carcinoma of the skin (Merkel cell carcinoma). A histological, immunohistochemical and ultrastructural study of 13 cases. Pathology. 1986, 18: 393-399.
Sibley RK, Dahl D: Primary neuroendocrine (Merkel cell?) carcinoma of the skin. II. An immunocytochemical study of 21 cases. Am J Surg Pathol. 1985, 9: 109-116.
Kurokawa M, Nabeshima K, Akiyama Y, Maeda S, Nishida T, Nakayama F, Amano M, Ogata K, Setoyama M: CD56: a useful marker for diagnosing Merkel cell carcinoma. J Dermatol Sci. 2003, 31: 219-224. 10.1016/S0923-1811(03)00029-X.
Gallego R, Garcia-Caballero T, Fraga M, Beiras A, Forteza J: Neural cell adhesion molecule immunoreactivity in Merkel cells and Merkel cell tumours. Virchows Arch. 1995, 426: 317-321. 10.1007/BF00191370.
McNiff JM, Cowper SE, Lazova R, Subtil A, Glusac EJ: CD56 staining in Merkel cell carcinoma and natural killer-cell lymphoma: magic bullet, diagnostic pitfall, or both?. J Cutan Pathol. 2005, 32: 541-545. 10.1111/j.0303-6987.2005.00378.x.
Weiler R, Fischer-Colbrie R, Schmid KW, Feichtinger H, Bussolati G, Grimelius L, Krisch K, Kerl H, O'Connor D, Winkler H: Immunological studies on the occurrence and properties of chromogranin A and B and secretogranin II in endocrine tumors. Am J Surg Pathol. 1988, 12: 877-884.
Haneke E, Schulze HJ, Mahrle G: Immunohistochemical and immunoelectron microscopic demonstration of chromogranin A in formalin-fixed tissue of Merkel cell carcinoma. J Am Acad Dermatol. 1993, 28: 222-226.
Koljonen V, Haglund C, Tukiainen E, Bohling T: Neuroendocrine differentiation in primary Merkel cell carcinoma--possible prognostic significance. Anticancer Res. 2005, 25: 853-858.
Wiedenmann B, Franke WW, Kuhn C, Moll R, Gould VE: Synaptophysin: a marker protein for neuroendocrine cells and neoplasms. Proc Natl Acad Sci U S A. 1986, 83: 3500-3504.
Wiedenmann B, Huttner WB: Synaptophysin and chromogranins/secretogranins--widespread constituents of distinct types of neuroendocrine vesicles and new tools in tumor diagnosis. Virchows Arch B Cell Pathol Incl Mol Pathol. 1989, 58: 95-121.
Miettinen M: Synaptophysin and neurofilament proteins as markers for neuroendocrine tumors. Arch Pathol Lab Med. 1987, 111: 813-818.
Gould VE, Wiedenmann B, Lee I, Schwechheimer K, Dockhorn-Dworniczak B, Radosevich JA, Moll R, Franke WW: Synaptophysin expression in neuroendocrine neoplasms as determined by immunocytochemistry. Am J Pathol. 1987, 126: 243-257.
Buffa R, Rindi G, Sessa F, Gini A, Capella C, Jahn R, Navone F, De Camilli P, Solcia E: Synaptophysin immunoreactivity and small clear vesicles in neuroendocrine cells and related tumours. Mol Cell Probes. 1987, 1: 367-381. 10.1016/0890-8508(87)90018-1.
Liu Y, Sturgis CD, Grzybicki DM, Jasnosz KM, Olson PR, Tong M, Dabbs DD, Raab SS, Silverman JF: Microtubule-associated protein-2: a new sensitive and specific marker for pulmonary carcinoid tumor and small cell carcinoma. Mod Pathol. 2001, 14: 880-885. 10.1038/modpathol.3880406.
Liu Y, Saad RS, Shen SS, Silverman JF: Diagnostic Value of Microtubule-Associated Protein-2 (MAP-2) for Neuroendocrine Neoplasms. Adv Anat Pathol. 2003, 10: 101-106. 10.1097/00125480-200303000-00005.
Fang D, Hallman J, Sangha N, Kute TE, Hammarback JA, White WL, Setaluri V: Expression of microtubule-associated protein 2 in benign and malignant melanocytes: implications for differentiation and progression of cutaneous melanoma. Am J Pathol. 2001, 158: 2107-2115.
Liu Y, Mangini J, Saad R, Silverman AR, Abell E, Tung MY, Graner SR, Silverman JF: Diagnostic value of microtubule-associated protein-2 in Merkel cell carcinoma. Appl Immunohistochem Mol Morphol. 2003, 11: 326-329.
Van Gele M, Van Roy N, Ronan SG, Messiaen L, Vandesompele J, Geerts ML, Naeyaert JM, Blennow E, Bar-Am I, Das Gupta TK, van der Drift P, Versteeg R, Leonard JH, Speleman F: Molecular analysis of 1p36 breakpoints in two Merkel cell carcinomas. Genes, Chromosomes and Cancer. 1998, 23: 67-71. 10.1002/(SICI)1098-2264(199809)23:1<67::AID-GCC10>3.0.CO;2-B.
Van Gele M, Leonard JH, Van Roy N, Van Limbergen H, Van Belle S, Cocquyt V, Salwen H, De Paepe A, Speleman F: Combined karytyping, CGH and M-FISH analysis allows detailed characterization of unidnetified chromosomal rearrangements in Merkel cell carcinoma. International Journal of Cancer. 2002, 101: 137-145. 10.1002/ijc.10591.
Popp S, Waltering S, Herbst C, Moll I, Boukamp P: UV-B-type mutations and chromosomal imbalances indicate common pathways for the development of Merkel and skin squamous cell carcinomas. Int J Cancer. 2002, 99: 352-360. 10.1002/ijc.10321.
Gancberg D, Feoli F, Hamels J, de Saint-Aubain N, Andre J, Rouas G, Verhest A, Larsimont D: Trisomy 6 in Merkel cell carcinoma: a recurrent chromosomal aberration. Histopathology. 2000, 37: 445-451. 10.1046/j.1365-2559.2000.01011.x.
Larsimont D, Verhest A: Chromosome 6 trisomy as sole anomaly in a primary Merkel cell carcinoma. Virchows Arch. 1996, 428: 305-309. 10.1007/BF00196706.
Vortmeyer AO, Merino MJ, Boni R, Liotta LA, Cavazzana A, Zhuang Z: Genetic changes associated with primary Merkel cell carcinoma. Am J Clin Pathol. 1998, 109: 565-570.
Leonard JH, Leonard P, Kearsley JH: Chromosomes 1, 11, and 13 are frequently involved in karyotypic abnormalities in metastatic Merkel cell carcinoma. Cancer Genet Cytogenet. 1993, 67: 65-70. 10.1016/0165-4608(93)90046-O.
Amo-Takyi BK, Tietze L, Tory K, Guerreiro P, Gunther K, Bhardwaj RS, Mittermayer C, Handt S: Diagnostic relevance of chromosomal in-situ hybridization in Merkel cell carcinoma: targeted interphase cytogenetic tumour analyses. Histopathology. 1999, 34: 163-169. 10.1046/j.1365-2559.1999.00580.x.
Leonard JH, Hayard N: Loss of heterozygosity of chromosome 13 in Merkel cell carcinoma. Genes Chromosomes Cancer. 1997, 20: 93-97. 10.1002/(SICI)1098-2264(199709)20:1<93::AID-GCC14>3.0.CO;2-G.
Van Gele M, Speleman F, Vandesompele J, Van Roy N, Leonard JH: Characteristic pattern of chromosomal gains and losses in Merkel cell carcinoma detected by comparative genomic hybridization. Cancer Research. 1998, 58: 1503-1508.
Larramendy ML, Koljonen V, Bohling T, Tukiainen E, Knuutila S: Recurrent DNA copy number changes revealed by comparative genomic hybridization in primary Merkel cell carcinomas. Mod Pathol. 2004, 17: 561-567. 10.1038/modpathol.3800091.
Yiengpruksawan A, Coit DG, Thaler HT, Urmacher C, Knapper WK: Merkel cell carcinoma. Prognosis and management. Arch Surg. 1991, 126: 1514-1519.
Hitchcock CL, Bland KI, Laney RG, Franzini D, Harris B, Copeland EM: Neuroendocrine (Merkel cell) carcinoma of the skin. Its natural history, diagnosis, and treatment. Ann Surg. 1988, 207: 201-207.
Chuang TY, Su WP, Muller SA: Incidence of cutaneous T cell lymphoma and other rare skin cancers in a defined population. J Am Acad Dermatol. 1990, 23: 254-256.
Pan D, Naryan D, Ariyan S: Merkel Cell Carcinoma: Five Case reports Using Sentinel Lymph Node Biopsy and Review of 110 New Cases. Plastic and Reconstructive surgery. 2002, 110: 1259 -11265. 10.1097/00006534-200210000-00007.
Hodgson NC: Merkel cell carcinoma: changing incidence trends. J Surg Oncol. 2005, 89: 1-4. 10.1002/jso.20167.
Landis SH, Murray T, Bolden S, Wingo PA: Cancer statistics, 1998. CA Cancer J Clin. 1998, 48: 6-29.
Miller RW, Rabkin CS: Merkel cell carcinoma and melanoma: etiological similarities and differences. Cancer Epidemiol Biomarkers Prev. 1999, 8: 153-158.
Anderson LL, Phipps TJ, McCollough ML: Neuroendocrine carcinoma of the skin (Merkel cell carcinoma) in a black. J Dermatol Surg Oncol. 1992, 18: 375-380.
Chao TC, Park JM, Rhee H, Greager JA: Merkel cell tumor of the back detected during pregnancy. Plast Reconstr Surg. 1990, 86: 347-351.
Matichard E, Descamps V, Grossin M, Genin R, Bouvet E, Crickx B: Merkel cell carcinoma in a black human immunodeficiency virus-infected patient. Br J Dermatol. 2002, 146: 671-673. 10.1046/j.1365-2133.2002.04592.x.
Feun LG, Savaraj N, Legha SS, Silva EG, Benjamin RS, Burgess MA: Chemotherapy for metastatic Merkel cell carcinoma. Review of the M.D. Anderson Hospital's experience. Cancer. 1988, 62: 683-685.
Boyle F, Pendlebury S, Bell D: Further insights into the natural history and management of primary cutaneous neuroendocrine (Merkel cell) carcinoma. Int J Radiat Oncol Biol Phys. 1995, 31: 315-323. 10.1016/0360-3016(93)E0110-R.
Meeuwissen JA, Bourne RG, Kearsley JH: The importance of postoperative radiation therapy in the treatment of Merkel cell carcinoma. Int J Radiat Oncol Biol Phys. 1995, 31: 325-331. 10.1016/0360-3016(94)E0145-A.
Akhtar S, Oza KK, Wright J: Merkel cell carcinoma: report of 10 cases and review of the literature. J Am Acad Dermatol. 2000, 43: 755-767. 10.1067/mjd.2000.106505.
Ott MJ, Tanabe KK, Gadd MA, Stark P, Smith BL, Finkelstein DM, Souba WW: Multimodality management of Merkel cell carcinoma. Arch Surg. 1999, 134: 388-92; discussion 392-3. 10.1001/archsurg.134.4.388.
Colombo F, Holbach LM, Junemann AG, Schlotzer-Schrehardt U, Naumann GO: Merkel cell carcinoma: clinicopathologic correlation, management, and follow-up in five patients. Ophthal Plast Reconstr Surg. 2000, 16: 453-458. 10.1097/00002341-200011000-00010.
Pergolizzi JJ, Sardi A, Pelczar M, Conaway GL: Merkel cell carcinoma: an aggressive malignancy. Am Surg. 1997, 63: 450-454.
Savage P, Constenla D, Fisher C, Thomas JM, Gore ME: The natural history and management of Merkel cell carcinoma of the skin: a review of 22 patients treated at the Royal Marsden Hospital. Clin Oncol (R Coll Radiol). 1997, 9: 164-167.
Penn I, First MR: Merkel's cell carcinoma in organ recipients: report of 41 cases. Transplantation. 1999, 68: 1717-1721. 10.1097/00007890-199912150-00015.
Tai PT, Yu E, Winquist E, Hammond A, Stitt L, Tonita J, Gilchrist J: Chemotherapy in neuroendocrine/Merkel cell carcinoma of the skin: case series and review of 204 cases. J Clin Oncol. 2000, 18: 2493-2499.
Lawenda BD, Thiringer JK, Foss RD, Johnstone PA: Merkel cell carcinoma arising in the head and neck: optimizing therapy. Am J Clin Oncol. 2001, 24: 35-42. 10.1097/00000421-200102000-00006.
Allen PJ, Bowne WB, Jaques DP, Brennan MF, Busam K, Coit DG: Merkel cell carcinoma: prognosis and treatment of patients from a single institution. J Clin Oncol. 2005, 23: 2300-2309. 10.1200/JCO.2005.02.329.
Tai PT, Yu E, Tonita J, Gilchrist J: Merkel cell carcinoma of the skin. J Cutan Med Surg. 2000, 4: 186-195.
Koljonen V, Bohling T, Granhroth G, Tukiainen E: Merkel cell carcinoma: a clinicopathological study of 34 patients. Eur J Surg Oncol. 2003, 29: 607-610. 10.1016/S0748-7983(03)00110-0.
Mott RT, Smoller BR, Morgan MB: Merkel cell carcinoma: a clinicopathologic study with prognostic implications. J Cut Pathol. 2004, 31: 217-10.1111/j.0303-6987.2004.00149.x.
Mehrany K, Otley CC, Weenig RH, Phillips PK, Roenigk RK, Nguyen TH: A Meta-analysis of the Prognostic Significance of Sentinel Lymph Node Status in Merkel Cell Carcinoma. Dermatol Surg. 2002, 28: 113-117. 10.1046/j.1524-4725.2002.02901.x.
Hohaus K, Kostler E, Schonlebe J, Klemm E, Wollina U: Merkel cell carcinoma--a retrospective analysis of 17 cases. J Eur Acad Dermatol Venereol. 2003, 17: 20-24. 10.1046/j.1468-3083.2003.00592.x.
Allen PJ, Busam K, Hill AD, Stojadinovic A, Coit DG: Immunohistochemical analysis of sentinel lymph nodes from patients with Merkel cell carcinoma. Cancer. 2001, 92: 1650-1655. 10.1002/1097-0142(20010915)92:6<1650::AID-CNCR1491>3.0.CO;2-8.
Poulsen MG, Rischin D, Porter I, Walpole E, Harvey J, Hamilton C, Keller J, Tripcony L: Does chemotherapy improve survival in high-risk stage I and II merkel cell carcinoma of the skin?. Int J Radiat Oncol Biol Phys. 2005
Connelly TJ, Cribier B, Brown TJ, Yanguas I: Complete spontaneous regression of Merkel cell carcinoma: a review of the 10 reported cases. Dermatol Surg. 2000, 26: 853-856. 10.1046/j.1524-4725.2000.00054.x.
Junquera L, Torre A, Vicente JC, Garcia-Consuegra L, Fresno MF: Complete spontaneous regression of Merkel cell carcinoma. Ann Otol Rhinol Laryngol. 2005, 114: 376-380.
Mori Y, Hashimoto K, Tanaka K, Cui CY, Mehregan DR, Stiff MA: A study of apoptosis in Merkel cell carcinoma: an immunohistochemical, ultrastructural, DNA ladder, and TUNEL labeling study. Am J Dermatopathol. 2001, 23: 16-23.
Inoue T, Yoneda K, Manabe M, Demitsu T: Spontaneous regression of merkel cell carcinoma: a comparative study of TUNEL index and tumor-infiltrating lymphocytes between spontaneous regression and non-regression group. J Dermatol Sci. 2000, 24: 203-211. 10.1016/S0923-1811(00)00103-1.
Ziprin P, Smith S, Salerno G, Rosin RD: Two cases of merkel cell tumour arising in patients with chronic lymphocytic leukaemia. Br J Dermatol. 2000, 142: 525-528. 10.1046/j.1365-2133.2000.03370.x.
Sinclair N, Mireskandari K, Forbes J, Crow J: Merkel cell carcinoma of the eyelid in association with chronic lymphocytic leukaemia. Br J Ophthalmol. 2003, 87: 240-10.1136/bjo.87.2.240.
Papageorgiou KI, Kaniorou-Larai MM: A case repot of Merkel cell carcinoma on chronic lymphocytic leukemia: differential diagnosis of coexisting lymphadenopathy and indications for early aggressive treatment. BMC Cancer. 2005, 5: 106-10.1186/1471-2407-5-106.
Brenner B, Sulkes A, Rakowsky E, Feinmesser M, Yukelson A, Bar-Heim E, Katz A, Idelevich E, Neuman A, Barhana M, Fenig E: Second Neoplasms in Patients with Merkel Cell carcinoma. Cancer. 2001, 91: 1358 -11362. 10.1002/1097-0142(20010401)91:7<1358::AID-CNCR1139>3.0.CO;2-C.
Kurul S, Mudun A, Aksakal N, Aygen M: Lymphatic Mapping for Merkel Cell Carcinoma. Plastic and Reconstructive surgery. 2000, 105: 680 -6683.
Buell JF, Trofe J, Hanaway MJ, Beebe TM, Gross TG, Alloway RR, First MR, Woodle ES: Immunosuppression and Merkel cell carcinoma. Transplantation Proceedings. 2002, 34: 1780-1781. 10.1016/S0041-1345(02)03065-8.
Gooptu C, Woollons A, Ross J, Proce M, Wojnarowska F, Morris PJ, Bunker CB: Merkel cell carcinoma arising after therapeutic immusuppression. British Journal of Dermatology. 1997, 137: 637-641.
Engels EA, Frisch M, Goedert JJ, Biggar RJ, Miller RW: Merkel cell carcinoma and HIV infection. Lancet. 2002, 359: 497-498. 10.1016/S0140-6736(02)07668-7.
Kokoska ER, Kokoska MS, Collins BT, Stapleton DR, Wade TP: Early aggressive treatment for Merkel cell carcinoma improves outcome. Am J Surg. 1997, 174: 688-693. 10.1016/S0002-9610(97)00193-1.
Linjawi A, Jamison WB, Meterissian S: Merkel cell carcinoma: important aspects of diagnosis and management. Am Surg. 2001, 67: 943-947.
Agelli M, Clegg LX: Epidemiology of primary Merkel cell carcinoma in the United States. J Am Acad Dermatol. 2003, 49: 832-841. 10.1016/S0190-9622(03)02108-X.
Medina-Franco H, Urist MM, Fiveash J, Heslin MJ, Bland KI, Beenken SW: Multimodality treatment of Merkel cell carcinoma: case series and literature review of 1024 cases. Ann Surg Oncol. 2001, 8: 204-208.
Eusebi V, Capella C, Cossu A, Rosai J: Neuroendocrine carcinoma within lymph nodes in the absence of a primary tumor, with special reference to Merkel cell carcinoma. Am J Surg Pathol. 1992, 16: 658-666.
Ferrara G, Ianniello GP, Di Vizio D, Nappi O: Lymph node Merkel cell carcinoma with no evidence of cutaneous tumor--report of two cases. Tumori. 1997, 83: 868-872.
Gillenwater AM, Hessel AC, Morrison WH, Burgess M, Silva EG, Roberts D, Goepfert H: Merkel cell carcinoma of the head and neck: effect of surgical excision and radiation on recurrence and survival. Arch Otolaryngol Head Neck Surg. 2001, 127: 149-154.
Raaf JH, Urmacher C, Knapper WK, Shiu MH, Cheng EW: Trabecular (Merkel cell) carcinoma of the skin. Treatment of primary, recurrent, and metastatic disease. Cancer. 1986, 57: 178-182.
Hanke WC, Conner AC, Temofeew RK, Lingeman RE: Merkel cell carcinoma. Arch Dermatol. 1989, 125: 1096-1100. 10.1001/archderm.125.8.1096.
Sibley RK, Dehner LP, Rosai J: Primary neuroendocrine (Merkel cell?) carcinoma of the skin. I. A clinicopathologic and ultrastructural study of 43 cases. Am J Surg Pathol. 1985, 9: 95-108.
Wynne CJ, Kearsley JH: Merkel cell tumor. A chemosensitive skin cancer. Cancer. 1988, 62: 28-31.
Shack RB, Barton RM, DeLozier J, Rees RS, Lynch JB: Is aggressive surgical management justified in the treatment of Merkel cell carcinoma?. Plast Reconstr Surg. 1994, 94: 970-975.
Brissett AE, Olsen KD, Kasperbauer JL, Lewis JE, Goellner JR, Spotts BE, Weaver AL, Strome SE: Merkel cell carcinoma of the head and neck: a retrospective case series. Head Neck. 2002, 24: 982-988. 10.1002/hed.10153.
O'Connor WJ, Brodland DG: Merkel cell carcinoma. Dermatol Surg. 1996, 22: 262-267. 10.1016/1076-0512(95)00580-3.
Silva EG, Mackay B, Goepfert H, Burgess MA, Fields RS: Endocrine carcinoma of the skin (Merkel cell carcinoma). Pathol Annu. 1984, 19 Pt 2: 1-30.
Ames SE, Krag DN, Brady MS: Radiolocalization of the sentinel lymph node in Merkel cell carcinoma: a clinical analysis of seven cases. J Surg Oncol. 1998, 67: 251-254. 10.1002/(SICI)1096-9098(199804)67:4<251::AID-JSO8>3.0.CO;2-7.
Rodrigues LK, Leong SP, Kashani-Sabet M, Wong JH: Early experience with sentinel lymph node mapping for Merkel cell carcinoma. J Am Acad Dermatol. 2001, 45: 303-308. 10.1067/mjd.2001.114749.
Wasserberg N, Schachter J, Fenig E, Feinmesser M, Gutman H: Applicability of the sentinel node technique to Merkel cell carcinoma. Dermatol Surg. 2000, 26: 138-141. 10.1046/j.1524-4725.2000.99213.x.
Schmalbach CE, Lowe L, Teknos TN, Johnson TM, Bradford CR: Reliability of sentinel lymph node biopsy for regional staging of head and neck merkel cell carcinoma. Arch Otolaryngol Head Neck Surg. 2005, 131: 610-614. 10.1001/archotol.131.7.610.
de Mortillet S, Laurent B, Fassio E, Zimmann F, Bonin B, Brie J, Goga D, Ballon G: [Cervicofacial involvement of primary cutaneous neuroendocrine carcinomas or Merkel cell tumors: therapeutic considerations]. Rev Stomatol Chir Maxillofac. 1995, 96: 33-35.
Shaw JH, Rumball E: Merkel cell tumour: clinical behaviour and treatment. Br J Surg. 1991, 78: 138-142.
Victor NS, Morton B, Smith JW: Merkel cell cancer: is prophylactic lymph node dissection indicated?. Am Surg. 1996, 62: 879-882.
Allen PJ, Zhang ZF, Coit DG: Surgical management of Merkel cell carcinoma. Ann Surg. 1999, 229: 97-105. 10.1097/00000658-199901000-00013.
Cottel WI, Bailin PL, Albom MJ, Bernstein G, Braun M, Hanke CW, Sutnick TB, Swanson NA: Essentials of Mohs micrographic surgery. J Dermatol Surg Oncol. 1988, 14: 11-13.
Boyer JD, Zitelli JA, Brodland DG, D'Angelo G: Local control of primary Merkel cell carcinoma: review of 45 cases treated with Mohs micrographic surgery with and without adjuvant radiation. J Am Acad Dermatol. 2002, 47: 885-892. 10.1067/mjd.2002.125083.
O'Connor WJ, Roenigk RK, Brodland DG: Merkel cell carcinoma. Comparison of Mohs micrographic surgery and wide excision in eighty-six patients. Dermatol Surg. 1997, 23: 929-933. 10.1016/S1076-0512(97)00292-6.
Waldmann V, Goldschmidt H, Jackel A, Deichmann M, Hegenbart U, Hartschuh W, Ho A, Naher H: Transient complete remission of metastasized Merkel cell carcinoma by high-dose polychemotherapy and autologous peripheral blood stem cell transplantation. Br J Dermatol. 2000, 143: 837-839. 10.1046/j.1365-2133.2000.03852.x.
Voog E, Biron P, Martin JP, Blay JY: Chemotherapy for patients with locally advanced or metastatic Merkel cell carcinoma. Cancer. 1999, 85: 2589-2595. 10.1002/(SICI)1097-0142(19990615)85:12<2589::AID-CNCR15>3.0.CO;2-F.
Samonis G, Mantadakis E, Kononas TC, Rigatos SK, Stathopoulos GP: Merkel cell carcinoma: a case series of twelve patients and review of the literature. Anticancer Res. 2001, 21: 4173-4177.
Fenig E, Lurie H, Sulkes A: The use of cyclophosphamide, methotrexate, and 5-fluorouracil in the treatment of Merkel cell carcinoma. Am J Clin Oncol. 1993, 16: 54-57.
Leonard JH, Ramsay JR, Kearsley JH, Birrell GW: Radiation sensitivity of Merkel cell carcinoma cell lines. Int J Radiat Oncol Biol Phys. 1995, 32: 1401-1407. 10.1016/0360-3016(94)00610-W.
Bourne RG, O'Rourke MG: Management of Merkel cell tumour. Aust N Z J Surg. 1988, 58: 971-974.
Herbst A, Haynes HA, Nghiem P: The standard of care for Merkel cell carcinoma should include adjuvant radiation and lymph node surgery. J Am Acad Dermatol. 2002, 46: 640-642. 10.1067/mjd.2002.119667.
Veness MJ, Morgan GJ, Gebski V: Adjuvant locoregional radiotherapy as best practice in patients with Merkel cell carcinoma of the head and neck. Head Neck. 2005, 27: 208-216. 10.1002/hed.20134.
Veness MJ, Perera L, McCourt J, Shannon J, Hughes TM, Morgan GJ, Gebski V: Merkel cell carcinoma: improved outcome with adjuvant radiotherapy. ANZ J Surg. 2005, 75: 275-281. 10.1111/j.1445-2197.2005.03353.x.
Mortier L, Mirabel X, Fournier C, Piette F, Lartigau E: Radiotherapy alone for primary Merkel cell carcinoma. Arch Dermatol. 2003, 139: 1587-1590. 10.1001/archderm.139.12.1587.
Pacella J, Ashby M, Ainslie J, Minty C: The role of radiotherapy in the management of primary cutaneous neuroendocrine tumors (Merkel cell or trabecular carcinoma): experience at the Peter MacCallum Cancer Institute (Melbourne, Australia). Int J Radiat Oncol Biol Phys. 1988, 14: 1077-1084.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
VK: concived the idea, did literature search, wrote the article and edited it for its final content.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Koljonen, V. Merkel cell carcinoma. World J Surg Onc 4, 7 (2006). https://doi.org/10.1186/1477-7819-4-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1477-7819-4-7