Abstract
Background
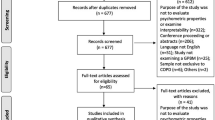
Cost utility analysis (CUA) using SF-36/SF-12 data has been facilitated by the development of several preference-based algorithms. The purpose of this study was to illustrate how decision-making could be affected by the choice of preference-based algorithms for the SF-36 and SF-12, and provide some guidance on selecting an appropriate algorithm.
Methods
Two sets of data were used: (1) a clinical trial of adult asthma patients; and (2) a longitudinal study of post-stroke patients. Incremental costs were assumed to be $2000 per year over standard treatment, and QALY gains realized over a 1-year period. Ten published algorithms were identified, denoted by first author: Brazier (SF-36), Brazier (SF-12), Shmueli, Fryback, Lundberg, Nichol, Franks (3 algorithms), and Lawrence. Incremental cost-utility ratios (ICURs) for each algorithm, stated in dollars per quality-adjusted life year ($/QALY), were ranked and compared between datasets.
Results
In the asthma patients, estimated ICURs ranged from Lawrence's SF-12 algorithm at $30,769/QALY (95% CI: 26,316 to 36,697) to Brazier's SF-36 algorithm at $63,492/QALY (95% CI: 48,780 to 83,333). ICURs for the stroke cohort varied slightly more dramatically. The MEPS-based algorithm by Franks et al. provided the lowest ICUR at $27,972/QALY (95% CI: 20,942 to 41,667). The Fryback and Shmueli algorithms provided ICURs that were greater than $50,000/QALY and did not have confidence intervals that overlapped with most of the other algorithms. The ICUR-based ranking of algorithms was strongly correlated between the asthma and stroke datasets (r = 0.60).
Conclusion
SF-36/SF-12 preference-based algorithms produced a wide range of ICURs that could potentially lead to different reimbursement decisions. Brazier's SF-36 and SF-12 algorithms have a strong methodological and theoretical basis and tended to generate relatively higher ICUR estimates, considerations that support a preference for these algorithms over the alternatives. The "second-generation" algorithms developed from scores mapped from other indirect preference-based measures tended to generate lower ICURs that would promote greater adoption of new technology. There remains a need for an SF-36/SF-12 preference-based algorithm based on the US general population that has strong theoretical and methodological foundations.
Similar content being viewed by others
Background
Health-related quality of life (HRQL) measures have many applications, including the measurement of population health status and outcomes of medical interventions that subsequently can be applied to economic evaluations of health care interventions. One such method of economic evaluation, cost utility analysis (CUA), is a special form of cost effectiveness analysis that evaluates incremental costs and effects of an intervention by assessing health effects using quality-adjusted life years (QALYs) [1]. QALYs incorporate both length of life and quality of life into a single metric, and are calculated by summing the time periods individuals spend in different health states, weighted by the qualities of the health states [2]. Because new therapies are typically more expensive than standard therapies, CUA has gained prominence as a method to inform decision makers who seek to compare the tradeoff in incremental costs and gains in health conferred by new treatment choices within and across disease states.
Optimally, CUA is used to guide the allocation of resources on a societal level. The Panel on Cost Effectiveness in Health and Medicine recommended that community preferences for health states collected from a representative sample of the US general population should be "the most appropriate ones for use in a Reference Case analysis" for US decision makers [2]. Such an approach is facilitated by indirect preference-based generic measures of health-related quality of life (HRQL) such as the Quality of Well-Being Scale [3], Health Utilities Index [4, 5], and EQ-5D [6, 7], as opposed to elicitation of preferences directly from patients using techniques such as the standard gamble, rating scale, and the time trade-off. Indirect preference-based HRQL measures typically generate index-based single summary scores for health states described by the instrument's classification system using an algorithm based on preferences of the community or general population.
An important development in health services research has been the emergence of algorithms that generate single preference-based summary scores based on items, domain scores, or summary scores from the Short Form 36 (SF-36) [8] and SF-12, a 12-item subset of the SF-36 [9]. While many SF-12 and SF-36 datasets are available due to the widespread use of this family of health assessment measures in clinical trials and population health surveys, their value for application to economic evaluations has been previously limited due to an absence of a scoring algorithm that could generate QALYs from SF-12 and SF-36 response sets. The preference-based algorithms provide an opportunity to use SF-36 and SF-12 data in CUA. As of 2004, 10 published algorithms were identified in the literature that were based on SF-36 or SF-12 items, subscale scores, or summary scores [10–18]. Each preference-based algorithm is unique, derived from different modeling approaches, items/domains, data and/or sources of preferences. Several of these algorithms have been compared in studies, and found to differ from one another and from valuations directly elicited from patients [19–22]. Studies have used some of the algorithms to conduct CUA [23–27], which may be used to inform health care resource allocation. Although the algorithms are known to produce different results, their impact on incremental cost-utility ratios (ICURs) and related decision-making in health care have not been clearly demonstrated.
The purpose of this study was to examine how choice of algorithm for the SF-36/SF-12 might affect decision-making. The specific objectives for the study were to calculate ICURs by applying each algorithm to data from 2 different studies that included longitudinal assessments of the SF-36, to compare the ranking of each algorithm-based ICUR across conditions, and finally to interpret whether differences in ICURs generated by each algorithm had the potential to affect decision making. There were two specific hypotheses. First, ICURs calculated from different algorithms were expected to differ because preferences derived from those algorithms had been found to be different [19]. Second, the rank ordering of ICURs was expected to be similar between the conditions, stroke and asthma, examined in the CUA simulations.
Methods
Data sources
To illustrate the outcomes of CUA using the different SF-36 algorithms, data with empiric responses to the SF-36 from patients were used from two different sources and conditions: (1) a clinical trial of adults with asthma [19]; and (2) a longitudinal study of health-related quality of life (HRQL) after stroke [28]. The study of asthma patients was a 12-month randomized controlled trial conducted in inhaled corticosteroid naïve adult patients with mild persistent to moderate persistent asthma that compared two inhaled corticosteroid treatments, triamcinolone acetonide hydrofluoroalkane and fluticasone propionate. Patient included in this trial were ≥ 18 years old, had had a forced expiratory volume in 1 second ≥ 60% of their predicted value after withholding inhaled β-agonists, and had had airway reversibility of ≥ 15% following the administration of an inhaled β-agonist. For the purpose of this analysis, responses to the SF-36 at baseline and 12 months were used.
The second source of data was a natural history of HRQL after stroke. Stroke patients who were hospitalized with a confirmed ischemic stroke and consented to participate were included. Patients were excluded if they were ≤ 18 years old, could not comprehend English-based questionnaire, lived > 150 kilometers from Edmonton, Alberta, had hemorrhagic or lower brain stem stroke, coma, global or Wernicke's aphasia, or life expectancy was less than 6 months for any medical reason. Patients were enrolled in the study within two weeks of stroke and no later than 3 weeks after stroke. Health status measures, including the SF-36, were self-assessed by patients. For this analysis, responses to the SF-36 at baseline and 6 months were used. Both the stroke and asthma studies used version 1 of the SF-36.
Measures
The SF-36 has been traditionally described as a psychometrically-derived generic health status profile, with 8 subscales and two summary scores, the physical component summary (PCS-36) score and the mental component summary (MCS-36) score. The eight domains include physical functioning (PF), role limitations-physical (RP), bodily pain (BP), general health (GH), mental health (MH), role limitations-emotional (RE), vitality (VT), and social functioning (SF). The SF-12 is a shorter, 12-item version of the SF-36 that does not generate domain scores but provides summary scores, the PCS-12 and MCS-12, that are highly predictive of the PCS-36 and MCS-36 [9]. Scores of the 8 subscales range from 0 to 100. The summary scores (i.e. PCS-36, MCS-36) have a mean score of 50 and a standard deviation of 10. Similarly, the PCS-12 and MCS-12 summary scores have a mean of 50 and a standard deviation of 10.
Preference-Based Algorithms for SF-36 and SF-12
Nine publications that derived 10 unique preference-based algorithms for the SF-36 or SF-12 were identified (Table 1) [10–18]. Four algorithms were identified that mapped scores for the SF-36, and 6 algorithms mapped scores for the SF-12. The mapping approach was described as 1st generation if the algorithm was derived from directly elicited preferences, and denoted as 2nd generation mapping if the SF-12/SF-36 algorithm was based upon scores from an indirect preference-based HRQL measure, such as the EQ-5D. Note that these algorithms relate to the most recently advocated algorithms, as several authors published earlier algorithms and subsequently published updates (e.g. Shmueli) [16]. For brevity, each published algorithm is identified by the name of the first author.
Brazier and colleagues constructed an econometric model for predicting health state valuations by first revising the SF-36 into a health status measure with 6 domains called the SF-6D [10]. Using a variant on the standard gamble, 249 health states defined by the SF-6D were valued by a representative sample of the UK general population. Ordinary least squares (OLS) models were estimated to predict all 18,000 SF-6D health states. The Brazier (SF-36) algorithm used for the present study was based on the parsimonious consistent model, the preferred specification for model 10. The same data and a similar approach was used to estimate an algorithm based on the SF-12 [17].
Fryback and colleagues predicted Quality of Well-being Index (QWB) scores from SF-36 domain scores using data collected from the Beaver Dam Health Outcomes Study [12]. A six-variable regression model with three main effects (PF, MH, and BP) and three interaction terms (GH*RP, PF*BP, and MH*BP) is used to estimate preferences.
Nichol and colleagues mapped the SF-36 to the preference-based Health Utility Index Mark 2 (HUI2). They estimated HUI2 scores from SF-36 domain scores and sociodemographic variables from a sample of Southern California Kaiser Permanente members [15]. The Nichol method used OLS models, retaining statistically significant parameter estimates that included all eight domains of the SF-36 and age of the respondent.
Shmueli updated an examination of the relationship between Visual Analog Scale (VAS) ratings and SF-36 domains provided in a population health survey in Israel by predicting VAS values from SF-36 domains using linear and non-linear regression models [16]. The model was anchored such that scores of 100 on all 8 SF-36 domains would result in a VAS score of 100. The present study used the anchored algorithm that included statistically significant coefficients for PF, MH, VT, and GH.
Franks and colleagues mapped the SF-12 to the EQ-5D Index and HUI3 using a convenience sample of 240 low-income, predominantly Latino and black patients visiting a community health center in New York [11]. Two equations were separately developed that mapped the PCS-12 and MCS-12 onto EQ-5D and HUI3 scores using OLS models. Described as a pilot, the authors observed that the level of explained variance was consistent with the Fryback and Nichol studies (between 50–60%). Franks led a second investigation, again mapping the SF-12 to EQ-5D scores, using data from the Medical Expenditure Panel Survey (MEPS) [18]. The algorithm based upon SF-12 responses that did not include demographic variables was utilized for the present study. In a similar analysis, Lawrence and colleagues predicted the EQ-5D scores from the SF-12 using MEPS data [13]. A series of 2-variable, 3-variable, and 6-variable models, based on functional variations on, and interactions between, the PCS-12 and MCS-12 were developed. The 2-variable model was advocated for its simplicity and predictive ability across a diverse set of subgroups in the validation set.
Finally, Lundberg and colleagues investigated the relationship of preference-based measures and the SF-12 based on self-assessed HRQL from a random sample of residents in Uppsala County of Sweden [14]. Linear regression models were used to predict valuations from 11 of the 12 items on the SF-12 (excluding the global health item), age, and gender. When using proportion explained variance as a criterion, the reduced VAS-based model that retained only significant coefficients was recommended, with 50% of variance explained by the model.
Data analysis
Empiric data for stroke and asthma were used to ensure that actual health state changes were represented. The present analysis was based on patients who completed both pre- and post- assessments and had no missing items. After the scoring algorithms were applied to SF-36 responses using the 10 algorithms [10–18], the change in utility was transformed into QALYs, with the assumption that the incremental gain/lose in health state utility was realized for a 1-year period. QALYs were calculated using the area under the curve (AUC) approach. We assumed incremental costs associated with the intervention were $2000 per year greater than standard treatment in both the stroke and asthma patients. Such costs over standard treatment were considered reasonable approximations for the costs of an innovative treatment in asthma and stroke, and although distributions of costs could have been used to further simulate a "realistic CUA", but would further complicate the paper without contributing to the main purpose of this study. The incremental cost utility ratio (ICUR) between the intervention and control groups was calculated by dividing incremental costs by gain in QALYs. The algorithms were ranked based on ICURs for each condition.
The pre/post domain and preference-based scores were described for both study groups visit using means and standard deviations. The 95% confidence intervals (CIs) for ICURs were based on the CIs for the preference scores. The pre/post change scores were evaluated with paired t-tests. The rank order of the ICURs was compared between the asthma and stroke groups using Spearman's correlation coefficient (rs). P-values < 0.05 were considered statistically significant.
Results
Of the 304 patients enrolled in the asthma study, 220 (72.4%) completed both the baseline and final SF-36 assessment. The stroke study had 81 of 124 initial respondents (65.3%) complete the SF-36 at baseline and final follow-up. In comparison to the patients in the asthma study, patients in the stroke study were older (mean age 67.4 years vs. 39.1 years) and had much lower mean average PF, RP, SF, and PCS scores (Table 2). Positive change was observed on all 8 domains of the SF-36 in the asthma patients from the baseline to the end of the study (all p-values < 0.01). Stroke patients showed trend towards improvement on all 8 domains, with significant improvement on all domains (p-values < 0.01) with the exception of GH and BP (p-values > 0.05).
According to the preference-based summary scores, all patients in both studies demonstrated statistically significant improvement from baseline to the end of the study (p-value < 0.001) (Table 3). In the asthma study, the mean (SD) change in preference scores ranged from 0.063 (0.117) to 0.130 (0.159). In the stroke study, change scores ranged between 0.055 (0.124) and 0.143 (0.215).
Table 4 shows the results from the two sets of CUA simulations, and the rank order of the algorithms. As the incremental cost of $2000 is held constant across the algorithms, the differences in QALYs are mirrored by the differences in ICURs. In the asthma patients, estimated ICURs ranged from Lawrence's SF-12 algorithm at $30,769/QALY (95% CI: 26,316 to 36,697) to Brazier's SF-36 algorithm at $63,492 (95% CI: 48,780 to 83,333). ICURs for the stroke cohort varied slightly more dramatically. The MEPS-based algorithm by Franks et al. provided the lowest ICUR at $27,972/QALY (95% CI: 20,942 to 41,667). The Fryback and Shmueli algorithms provided ICURs that were greater $50,000/QALY and did not have confidence intervals that overlapped with most of the other algorithms. The rank order of algorithms based on ICUR was similar across the two conditions, with rs = 0.60 (p-value < 0.10).
Discussion
The development of preference-based algorithms for the SF-36 and SF-12 to facilitate CUA has fostered studies that recognized these preference-based scores can differ from each other and from directly elicited valuations in patients with asthma, hypertension, lung transplantation, and osteoporosis [19, 20, 29, 30]. However, the extent to which the differences might lead to different decisions on implementing or reimbursing for a new technology has been unclear. Using actual health states self-assessed by patients and imputing what might be considered conservative costs for an innovative treatment, our analysis demonstrated that ICURs based on the derivation algorithms can vary dramatically. The 10 algorithms produced a wide range of ICURs that varied more than 2-fold in magnitude for the asthma cohort and almost 3-fold in the stroke study.
Although guidelines or thresholds for decision making based on cost per QALY are contentious, cost-effectiveness thresholds that health care decision makers are willing to accept in health care reimbursement decisions exist, if not explicitly, then implicitly. Some guidance has been published. The National Institute of Clinical Effectiveness (NICE) in the UK has indicated they do not have an explicit threshold [31], while a threshold of around £20,000 to £30,000 per QALY gained (about $37,000 to $55,000 in 2004 US dollars) [32, 33] or slightly higher [34] has been cited as the value used in making decisions. Laupacis et al (1992) suggested that a treatment costing less than $20,000/QALY could be considered very cost-effective, a treatment costing between $20,000/QALY and $100,000/QALY was judged acceptable, while a treatment costing more than $100,000/QALY was deemed not likely to be cost-effective [35]. Other studies have suggested that $50,000/QALY provides a threshold for judging cost effectiveness [36, 37]. Although arbitrary criteria, the application of any of the cited guidelines to the CUAs illustrated in the present study convey that the choice of algorithm can dictate whether the intervention is considered cost-effective or unacceptable. The choice of algorithm could determine whether a drug is considered for formulary listing, particularly if an emphasis is placed on cost-effectiveness as a criterion by the decision-making committee, as is often done by publicly funded health care systems.
The CUA simulations illustrated how selection of a specific algorithm could lead to a different interpretation of the cost-effectiveness of an intervention. In the asthma cohort, algorithms by Lawrence [13], and the three equations by Franks [11, 18] generated relatively smaller ICURs close to a level that may be considered very cost-effective, i.e. $20,000, with 95% confidence intervals that did not bound the $50,000/QALY threshold. In contrast, the Nichol, Fryback, and both Brazier methods produced ICUR point estimates above $50,000/QALYs that would be unacceptable by most guidelines. In stroke, the Lawrence and Franks methods again generated ICURs that would indicate the technology of interest was relatively cost-effective, at $30,000/QALY or less, while the algorithms by Shmueli [16] and Fryback [12] produced ICURs over $50,000/QALY. In examining the robustness of the results, all algorithms produced ICURs below $20,000/QALY when incremental costs for the hypothetical intervention are reduced to less than $500, but algorithm selection becomes critical as incremental costs increase and thresholds such as $20,000/QALYs or $50,000/QALY are crossed.
Changes in the rank order of algorithms between conditions can be explained, not only by differences in the preference-based weighting assigned to each of the domain/summary scores, but several additional factors. There are differences in the SF-36 items or subscales retained by some of the methods. For instance, Brazier's SF-6D based on the SF-36 does not include GH, while the score generated by the Shmueli algorithm is largely influenced by the GH domain. The responsiveness/sensitivity of algorithms appears to be somewhat related to the scale range. It was not surprising that Fryback's method produced relatively larger ICURs that implied the intervention was less cost effective, as Fryback's method had a much smaller range of scale relative to the other algorithms (Table 1). Algorithms that incorporate demographic characteristics, such as the Nichol and Lundberg methods, provide estimates that are influenced by age of the cohort and could contribute to changes in their rank order.
In order to provide some guidance in the selection of preference-based algorithms for the SF-36 and SF-12 the algorithms were appraised in the context of their theoretical and methodological foundations, source of community-based preferences, and their relative potential to enhance or deter the uptake of new technology. The study results clearly illustrated that choice of algorithm can affect the estimated ICUR, and that there was a tendency for the Fryback and Shmueli methods to generate higher estimates of ICURs relative to the other algorithms. From a third-party payer perspective, algorithms generating higher ICURs would appeal to third-party reimbursement decision makers with short-term budget constraints, as algorithms that generate higher ICURs provide less encouraging evidence in the adoption of new technology when considered in the context of the $/QALY benchmarks previously discussed. The Panel on Cost Effectiveness of Health and Medicine [2] recommended that preference-based measures have a theoretical basis and represent community-based preferences. The Brazier algorithms are arguably most favorable on a theoretical basis. Only the Brazier, Lundberg, and Shmueli algorithms were based on preferences directly elicited from the general populace, i.e. first generation. The Lawrence, Franks, Nichol, and Fryback methods mapped the SF-12/SF-36 onto scores obtained from indirect utility-based measures, e.g. EQ-5D, HUI2, to derive what we termed "second generation" preference-based algorithms. Such an approach is limited by differences in the descriptive systems [17]. Interestingly, algorithms derived from directly elicited valuations of health states (i.e. first-generation mapping) tended to generate smaller magnitudes of change compared to the algorithms that mapped the SF-36/12 using other indirect utility measures (i.e. second-generation mapping). One explanation for the second-generation algorithms producing larger change scores is that several of them were derived from the utility scores of the HUI3 and EQ-5D, which have broader scale ranges compared to the SF-6D [38].
A further consideration is the theoretical foundation for the elicitation technique used in the valuation study. Only Brazier employed methodology using the SG technique for first-generation mapping. The SG has the most appeal in economic theory due to its foundations in Expected Utility Theory (EUT), although it has been suggested that the axioms of EUT are empirically flawed [39], and requires the respondent possess a rudimentary understanding of probabilities. Scores generated by Lundberg, Shmueli, and Fryback methods were based on first or second generation mapping of the SF-12/SF-36 onto scores from rating scales. Rating scales have been criticized for lack of theoretical basis in economics [39, 40], as a rating scale is not a choice-based technique and its ability to represent preferences on a cardinal scale is debatable. In contrast, the TTO and SG are choice-based techniques that generate utilities [2]. Lundberg utilized a variant of the TTO in addition to the VAS, but the complexity of the TTO task does not lend itself to a mail survey design. Lundberg observed that the TTO models did not perform as well as the VAS. Most of the algorithms were developed using self-assessed preferences for health status from a general population where severe states are rare, rather increasing the representation of more severe health states by statistical design, as done by Brazier [10, 17] and by other developers of preference-based measures [4, 7].
Given that HRQL may be valued differently between countries [41], an algorithm based on the preferences of a representative sample of the general population for the country of interest would be most desirable for resource allocation decision-making on the societal level, e.g. when the payer is the national ministry of health. The algorithms for the SF-36 find their preference-based origins from a diverse range of national sources. The algorithm by Shmueli was based on valuations obtained from representative samples of the Israeli Jewish population [16], while Lundberg's algorithm was based on valuations from the Sweden populace [14]. Brazier's utilities for health states were elicited from respondents in the United Kingdom [10]. The preferences for algorithms derived by Franks (EQ-5D) [11] and Lawrence [13] were mapped from the EQ-5D scoring function derived from the general population in the United Kingdom [7]. Fryback [12] mapped scores from the QWB that were based on community-based preferences from San Diego, California, USA [3]. The Nichol [11, 15] and Franks [11] algorithms were mapped from the utility-based scores of the HUI2 and HUI3 systems, respectively, that were originally elicited from respondents in Ontario, Canada [4, 5]. Nichol and Lundberg algorithms may not be considered as representing general population values because they include demographic variables such as age and/or gender. At present, only the Fryback algorithm has preferences originating from a community in the US, albeit a second generation mapping of those preferences.
Among the algorithms presently available, Brazier's algorithms for the SF-12 and SF-36 appear to be most favorable because of their methodological and theoretical basis. From the perspective of the third party reimbursement decision maker, the Brazier algorithms are not among those that tend to encourage adoption of new technology, tending to provide relatively higher estimates of ICUR. For those decision-makers, those algorithms would appear to be more fiscally conservative in the sense that they would not promote the adoption new technology any more than the other methods according to the results of this study. Although similar estimates are obtained using the Brazier SF-36 and SF-12 algorithms [17], it would be preferable to utilize the Brazier SF-36 algorithm rather than the SF-12-based algorithm if responses to the SF-36 are available because of the richer information afforded by the descriptive system. If alternative algorithms are used for CUA, it may be suggested to test robustness of conclusions by sensitivity analysis using Brazier's SF-36 or SF-12-based algorithms. At present, no SF-36/SF-12 algorithm has been published based on the first generation preferences of the US general population. As there is evidence to support health states valuations by the general US population differ from other countries[41], this represents an opportunity for future research leading to the development of an algorithm specific to the US as well as for other countries.
Note that there are several limitations and assumptions to the CUAs simulated in this paper. The primary purpose was to determine whether choice of preference-based algorithm applied to SF-36/SF-12 data has the potential to change the conclusion of a CUA; hence, aspects of the CUA not central to the purpose were simplified. For example, incremental costs were assumed to be constant, whereas in reality, considerable cost variance would be observed across patients. CUAs were performed in two patient populations, i.e., asthma patients and stroke patients, rather than using a single data set, to enhance the generalizability of the results. The rank order of the algorithms is limited to the datasets examined in this study, however, and comparisons of the algorithms across more diseases/conditions and persons with different demographic characteristics may provide stronger evidence of the rank order "stability". Change scores and thus ICUR estimates depend on baseline health status and the impact of an intervention on the various domains of health as captured by changes in responses to the SF-12/SF-36 items. Note that baseline domain scores for asthma and stroke cohorts were lower than US-based population norms. Several algorithm developers provide caveats for the application of their algorithm, including concerns about profiles severely limited by ceiling or floor effects [12], and inconsistent estimates and overprediction of poorest health states [10]. For instance, the descriptive system of the SF-6D is more concentrated at the milder end of health problems relative to the EQ-5D [42]. These concerns may be particularly relevant to the stroke cohort, where floor effects were observed.
Conclusion
In summary, SF-36/SF-12 preference-based algorithms tend to generate a wide range of ICURs that can potentially lead to different reimbursement decisions. Brazier's algorithms for the SF-36 and SF-12 had an arguably stronger methodological and theoretical basis, and tended to produce higher ICURs. For decision-makers who consider cost-effectiveness in the decision to reimburse for a new medical technology, selection of an algorithm that generates relatively higher ICURs would provide less convincing evidence of the cost-effectiveness of a new technology and consequently, its uptake. The "second-generation" algorithms mapped from other indirect preference-based measures tended to produce lower ICURs. When an alternative algorithm is selected, sensitivity analysis is recommended using the Brazier SF-12/SF-36 algorithm in order to examine the robustness of CUA. There remains a need for an SF-36/SF-12 algorithm developed from U.S.-based general population preferences with strong methodological and theoretical foundations.
References
Drummond MF, O'Brien BJ, Stoddart GL, Torrance GW: Methods for the economic evaluation of health care programmes. 2nd edition. Oxford, NY, Oxford University Press; 1997.
Gold MR, Siegel JE, Russell LB, Weinstein MC: Cost-Effectiveness in Health and Medicine. New York, NY, Oxford University Press; 1996.
Kaplan RM, Anderson JP: A general health policy model: update and applications. Health Serv Res 1988, 23: 203–235.
Feeny D, Furlong W, Torrance GW, Goldsmith CH, Zhu Z, DePauw S, Denton M, Boyle M: Multiattribute and single-attribute utility functions for the health utilities index mark 3 system. Med Care 2002, 40: 113–128. 10.1097/00005650-200202000-00006
Torrance GW, Feeny DH, Furlong WJ, Barr RD, Zhang Y, Wang Q: Multiattribute utility function for a comprehensive health status classification system. Health Utilities Index Mark 2. Med Care 1996, 34: 702–722. 10.1097/00005650-199607000-00004
Brooks R: EuroQol: the current state of play. Health Policy 1996, 37: 53–72. 10.1016/0168-8510(96)00822-6
Dolan P: Modeling valuations for EuroQol health states. Med Care 1997, 35: 1095–1108. 10.1097/00005650-199711000-00002
Ware JEJ, Snow KK, Kosinski M, Gandek B: SF-36 Health Survey: Manual and Interpretation Guide. Lincoln, RI, Quality Metric Incorporated; 1993.
Ware JE, Kosinski M, Keller SD: SF-12: How to scores the SF-12 Physical and Mental Health Summary Scales. Lincoln, RI, QualityMetric Inc.; 1998.
Brazier J, Roberts J, Deverill M: The estimation of a preference-based measure of health from the SF-36. J Health Econ 2002, 21: 271–292. 10.1016/S0167-6296(01)00130-8
Franks P, Lubetkin EI, Gold MR, Tancredi DJ: Mapping the SF-12 to preference-based instruments: convergent validity in a low-income, minority population. Med Care 2003, 41: 1277–1283. 10.1097/01.MLR.0000093480.58308.D8
Fryback DG, Lawrence WF, Martin PA, Klein R, Klein BE: Predicting Quality of Well-being scores from the SF-36: results from the Beaver Dam Health Outcomes Study. Med Decis Making 1997, 17: 1–9.
Lawrence WF, Fleishman JA: Predicting EuroQoL EQ-5D preference scores from the SF-12 Health Survey in a nationally representative sample. Med Decis Making 2004, 24: 160–169. 10.1177/0272989X04264015
Lundberg L, Johannesson M, Isacson DG, Borgquist L: The relationship between health-state utilities and the SF-12 in a general population. Med Decis Making 1999, 19: 128–140.
Nichol MB, Sengupta N, Globe DR: Evaluating quality-adjusted life years: estimation of the health utility index (HUI2) from the SF-36. Med Decis Making 2001, 21: 105–112. 10.1177/02729890122062352
Shmueli A: The relationship between the visual analog scale and the SF-36 scales in the general population: an update. Med Decis Making 2004, 24: 61–63. 10.1177/0272989X03261562
Brazier JE, Roberts J: The estimation of a preference-based measure of health from the SF-12. Med Care 2004, 42: 851–859. 10.1097/01.mlr.0000135827.18610.0d
Franks P, Lubetkin EI, Gold MR, Tancredi DJ, Jia H: Mapping the SF-12 to the EuroQol EQ-5D Index in a national US sample. Med Decis Making 2004, 24: 247–254. 10.1177/0272989X04265477
Lee TA, Hollingworth W, Sullivan SD: Comparison of directly elicited preferences to preferences derived from the SF-36 in adults with asthma. Med Decis Making 2003, 23: 323–334. 10.1177/0272989X03256009
Lobo FS, Gross CR, Matthees BJ: Estimation and comparison of derived preference scores from the SF-36 in lung transplant patients. Qual Life Res 2004, 13: 377–388. 10.1023/B:QURE.0000018488.95206.d6
Lenert LA, Sherbourne CD, Sugar C, Wells KB: Estimation of utilities for the effects of depression from the SF-12. Med Care 2000, 38: 763–770. 10.1097/00005650-200007000-00008
Hollingworth W, Deyo RA, Sullivan SD, Emerson SS, Gray DT, Jarvik JG: The practicality and validity of directly elicited and SF-36 derived health state preferences in patients with low back pain. Health Econ 2002, 11: 71–85. 10.1002/hec.650
Angus DC, Linde-Zwirble WT, Clermont G, Ball DE, Basson BR, Ely EW, Laterre PF, Vincent JL, Bernard G, van Hout B: Cost-effectiveness of drotrecogin alfa (activated) in the treatment of severe sepsis. Crit Care Med 2003, 31: 1–11. 10.1097/00003246-200301000-00001
Keeler EB, Robalino DA, Frank JC, Hirsch SH, Maly RC, Reuben DB: Cost-effectiveness of outpatient geriatric assessment with an intervention to increase adherence. Med Care 1999, 37: 1199–1206. 10.1097/00005650-199912000-00003
Wu SY, Sainfort F, Tomar RH, Tollios JL, Fryback DG, Klein R, Klein BEK: Development and application of a model to estimate the impact of type 1 diabetes on health-related quality of life. Diabetes Care 1998, 21: 725–731.
Griffiths TL, Phillips CJ, Davies S, Burr ML, Campbell IA: Cost effectiveness of an outpatient multidisciplinary pulmonary rehabilitation programme. Thorax 2001, 56: 779–784. 10.1136/thorax.56.10.779
Gray A, McNamara I, Aziz T, Gregory A, Bain P, Wilson J, Scott R: Quality of life outcomes following surgical treatment of Parkinson's disease. Movement Disorders 2002, 17: 68–75. 10.1002/mds.1259
Pickard AS, Johnson JA, Feeny DH, Carriere KC, Shuaib A, Nasser AM: Agreement between patient and proxy assessments of health-related quality of life after stroke using the EQ-5D and Health Utilities Index. Stroke 2004, 35: 607–612. 10.1161/01.STR.0000110984.91157.BD
Bardage C, Isacson D, Ring L, Bingefors K: A Swedish population-based study on the relationship between the SF-36 and health utilities to measure health in hypertension. Blood Press 2003, 12: 203–210. 10.1080/08037050310002083
Gabriel SE, Kneeland TS, Melton LJ, Moncur MM, Ettinger B, Tosteson AN: Health-related quality of life in economic evaluations for osteoporosis: whose values should we use? Med Decis Making 1999, 19: 141–148.
National Institute for Clinical Excellence. Health Select Committee Inquiry: submission of supplementary evidence. Paper 2 of 2. http://www.niceorguk/pageaspx?o=27652 [accessed June 10, 2004] 2002.
National Institute for Clinical Excellence. NICE Guidance on the use of orlistat for the treatment of obesity in adults. Technology Appraisal Guidance. http://www.niceorguk/pageaspx?o=15712 [accessed June 10, 2004] 2002.
Towse A: What is NICE's threshold? An external view. In Devlin N, Towse A. (eds) Cost effectiveness thresholds: economic and ethical issues. King's Fund /Office of Health Economics: London. 2002.
Devlin N, Parkin D: Does NICE have a cost-effectiveness threshold and what other factors influence its decisions? A binary choice analysis. Health Econ 2004, 13: 437–452. 10.1002/hec.864
Laupacis A, Feeny D, Detsky AS, Tugwell PX: How attractive does a new technology have to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. Cmaj 1992, 146: 473–481.
Salzmann P, Kerlikowske K, Phillips K: Cost-effectiveness of extending screening mammography guidelines to include women 40 to 49 years of age. Ann Intern Med 1997, 127: 955–965.
Lee TT, Solomon NA, Heidenreich PA, Oehlert J, Garber AM: Cost-effectiveness of screening for carotid stenosis in asymptomatic persons. Ann Intern Med 1997, 126: 337–346.
Pickard AS, Johnson JA, Feeny DH: Responsiveness of the SF-36, HUI, and EQ-5D in stroke. Qual Life Res 2005, 14: 207–219. 10.1007/s11136-004-3928-3
Brazier J, Deverill M, Green C: A review of the use of health status measures in economic evaluation. J Health Serv Res Policy 1999, 4: 174–184.
Torrance GW, Feeny D, Furlong W: Visual analog scales: do they have a role in the measurement of preferences for health states? Med Decis Making 2001, 21: 329–334. 10.1177/02729890122062622
Johnson JA, Ohinmaa A, Murti B, Sintonen H, Coons SJ: Comparison of Finnish and U.S.-based visual analog scale valuations of the EQ-5D measure. Med Decis Making 2000, 20: 281–289.
Brazier J, Roberts J, Tsuchiya A, Busschbach J: A comparison of the EQ-5D and SF-6D across seven patient groups. Health Econ 2004, 13: 873–884. 10.1002/hec.866
Acknowledgements
Astrazeneca provided funding support for the original stroke study through an unrestricted investigator initiated research grant.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
Drs. Pickard and Lee were responsible for the conception of the study and acquisition of data. Mr. Wang analyzed the data. Dr. Pickard and Mr. Wang were involved in the drafting of the article. All authors contributed to the interpretation of results and revising the article for important intellectual content.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Pickard, A.S., Wang, Z., Walton, S.M. et al. Are decisions using cost-utility analyses robust to choice of SF-36/SF-12 preference-based algorithm?. Health Qual Life Outcomes 3, 11 (2005). https://doi.org/10.1186/1477-7525-3-11
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1477-7525-3-11