Abstract
Bcl-3 is an established oncogene in hematologic malignancies, such as B-cell chronic lymphocytic leukemias. Nevertheless, recent research has shown that it also participates in progression of diverse solid tumors. The present review summarizes the current knowledge of Bcl3 role in solid tumors progression, including some new insights in its possible molecular mechanisms of action.
Similar content being viewed by others
Background
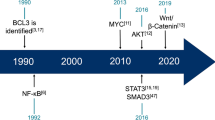
BCL3 was identified as a translocation into the immunoglobulin alpha-locus in several cases of B-cell chronic lymphocytic leukemias [1–4]. This oncogene is an atypical member of the Inhibitor of Kappa-B (IkappaB) family of proteins. Ikappa B proteins repress the activation of the NFkappa-B signaling cascade by direct binding to the dimeric transcription factors NFKB1, NFKB2, RELA, RELB or c-Rel. Interestingly, even with a high structural homology to the other family members [5, 6], Bcl-3 is instead a nuclear protein with both transactivation and transrepressor functions [7–10]. These actions are mainly mediated by the formation of heterocomplexes with NFKB1 (p50) or NFKB2 (p52) homodimers, in which Bcl-3 provides two transactivating domains to the complex.
Little is known about the physiological signaling cascades that activate Bcl-3. It has been reported that this oncogene is upregulated by several cytokines, including TNF alpha [11, 12], IL-4 [13], IL-1 [14, 15], IL-6 [16], IL-10 [17], adiponectin [18] and IL-12 [19]. These cytokines have in common their induction the activation of diverse signaling modules, such as AP1 [13] and STAT3 [16, 20, 21]. 'As with other members of the NF-kappa B family, Bcl-3 is regulated by NFKB1 and by itself, creating an autoregulatory loop to terminate its activation [16, 22]. In addition, as described below, Bcl-3 is downregulated by p53 [23] (Figure 1).
Bcl-3 signaling cascade. Diverse cytokines activate an IKK or IKK-related kinase to induce processing of the p105 precursor to p50, which in turn dimerizes and binds Bcl-3. Bcl-3 is regulated by phosphorylation and ubiquitination, both of which have a positive effect on its function. CYLD deubiquitinates Bcl-3 and prevents its nuclear translocation and GSK3. Bcl-3 is also phosphorylated by GSK3, which delays its degradation by the proteosomal pathway. Nuclear Bcl-3 can both induce and repress expression of a diverse array of genes.
Bcl-3 is also regulated by post-transcriptional mechanisms, such as translation [24, 25] and protein stability [26–30]. Recently, in ovarian cancer cells, a new regulation step was found, which involves miR-125b a microRNA that decreased Bcl-3 translation [31], inhibiting tumor formation in nude mice. Less is known about the reported nuclear translocation regulation, in which the cylindromatosis gene product, CYLD, plays an important role in interleukin-mediated activation [15, 32].
As stated previously, Bcl-3 forms a complex with p50 or p52 homodimers to regulate transcription. The first reports showed that Bcl-3 could be acting to enhance NF-kappa B-mediated transactivation by removing inhibitory p50 homodimers from NF-kappa consensus sites in diverse promoters [8, 33]. Subsequent studies using better reagents, demonstrated that Bcl-3 could not dissociate p50 homodimers from promoters [9]. Instead, Bcl-3 can act as a coactivator for p50 and p52 dimers [7]. More recently, it has also been shown that, for other specific promoters, such as the TNF-alpha promoter, Bcl-3 is indeed able to inhibit NF-kappa B-mediated transactivation, by binding to p50 homodimers, without dissociating them from a promoter, but also without inducing transactivation [17, 34, 35].
In addition to the gene products of the NF-kappa B signaling cascade, Bcl-3 also associates with several proteins such as Jab1, Pirin, Tip60 (KAT5) and Bard1, which are transcriptional co-regulators [36]. Bcl-2 also associates with B3BP, which is protein involved in DNA damage responses [37]; Lck, an important tyrosine kinase in hematological malignancies [38] and ERRalpha and PGC-1alpha, involved in metabolism [39]. Recent reports have shown that CtBP1, a transcriptional co-repressor [40]; IRS3, a substrate of insulin receptor and insulin-like growth factor (IGF)-I receptor tyrosine kinases [41] and Bcl-10 a CARD-containing protein that induces apoptosis [42] are also binding partners of Bcl-3 (Figure 2). These interactions and their physiological consequences have been little studied.
A) Proteins that interact with Bcl-3. B) Schematic representation of protein interactions from STRING (Search Tool for the Retrieval of Interacting Genes). Blue lines represent direct binding [79].
BCL3 locus has been found to be translocated not only in B-cell chronic leukemias, but also in other hematological malignancies, such as small lymphocytic lymphomas, Burkitt-like lymphoma and diffuse large cell lymphoma [43]. In addition, overexpression without translocation has been found in multiple subtypes of non-Hodgkin and Hodgkin lymphomas [44, 45]. These results underscore the importance of this oncogene in hematological neoplasias. In addition to this, Bcl-3 has been found to be deregulated in breast cancer [46], nasopharyngeal carcinoma [47], endometrial cancer [48] and colorectal cancer [40]. Here, we present current knowledge of the role of this oncogene in solid tumor progression, including some new insights in its possible molecular mechanisms of action.
Mechanism of deregulation
As with hematological malignancies, the most common Bcl-3 alteration found in solid tumors is overexpression. Nevertheless, in carcinomas, no translocations in the BCL3 locus have been found, pointing toward an activating upstream signal transduction cascade and/or epigenetic mechanism(s). Since NF-kappa B modulates BCL3 expression in an auto regulatory loop [22, 35], and NF-kappa B is constitutively activated in several tumors [49–51], it is probably that the observed Bcl-3 deregulation could be due to aberrant NF-kappa B activation. Additionally, most of the studies rely solely in the amount of nuclear Bcl-3 as a surrogate marker for its activation, since there is no reliable specific DNA consensus-binding site for the oncogene. Since it has been shown that Bcl-3 is heavily phosphorylated and this phosphorylation modulates its activity [26], it remains an open question whereas lower Bcl-3 levels of a specific phosphoisoform could be also acting in cancer progression. As stated previously, recent reports have shown that cylindromatosis (CYLD) gene product regulates Bcl-3 [28, 52]. The CYLD protein deubiquitinates Bcl-3 and inhibits its nuclear translocation, so alterations in these gene or upstream events to it present an additional layer of regulation.
It is important to note that the Catalog of Somatic Mutations in Cancer (COSMIC) [53] has a very low number of BCL3 mutations (2 missense mutations, one in a lung cancer and a second in an ovarian cancer patient) among its large database. These mutations most probably represent passenger mutations, since they apparently do not affect overall protein structure (additional file 1), and are not located in potential phosphorylation sites (not shown).
Deregulation in Solid Tumors
Breast cancer was the first solid tumor in which evidence for Bcl-3 deregulation was found. Cogswell, et al demonstrated that Bcl-3 mRNA and protein is over expressed in breast tumors and cell lines [46]. Their results also suggested that NF-kappa B was active in the tissue, as genes regulated by this signaling cascade were also concomitantly regulated, in contrast to surrounding normal stroma. Supporting this finding is the report that transgenic mice overexpressing c-Rel under the strong promoter of mouse mammary tumor virus (MMTV) developed tumors that overexpressed p50, p52, RelA, RelB, and the Bcl-3 protein [54]. Additional evidence comes from animal studies, in which it has been shown that overexpression of Bcl-3 is able to increase the establishment and growth of breast cancer xenografts [55]. In addition, estrogen withdrawal in breast cancer cell lines increased the expression and activity of Bcl-3, providing an alternative proliferation pathway and further advantage for tumor growth in mice.
Bcl-3 is also overexpressed and activated in nasopharyngeal carcinomas [47], where it is bound to p50 homodimers. Among others, this complex is bound to the promoter of the receptor for the Epidermal Growth Factor, playing a crucial role in the overexpression of this oncogene [47, 56, 57]. Similar to this report, it has been shown that Bcl-3 is also overexpressed in endometrial tumors [48], where its nuclear expression correlates with p52 immunostaining. It is interesting to note that Bcl-3 was the NF-kappa B subunit most detected, with 62% of the patient samples presenting nuclear Bcl-3 protein.
Recently, the first report associating Bcl-3 expression with a clinical outcome has been published. Puvvada, et al demonstrated that nuclear immunostaining of Bcl-3 was strongly associated with survival, even more than the other NF-kappa B subunits analyzed in colorectal cancer. Using a weighted score that combines percentage of positive nuclei with staining intensity, these authors found a 91% increase in hazard for a death event for each 50-point increase in nuclear Bcl-3 expression [58].
It is interesting to note that, even with the evidence presented here, there is only one article [58] exploring the possible use of Bcl-3 as a diagnostic/prognostic factor. Clearly, more research in this area is needed. In this regard, it is interesting that, in addition to the known deregulation in leukemias and lymphomas, genome-wide expression studies have shown that Bcl-3 is overexpressed in breast cancer, glioblastoma tumors, ovarian cancer and, intriguingly, teratomas and embryonal carcinomas (additional file 2). Although not validated, these results support the potential importance of this oncogene in a variety of tumors.
Mechanisms of oncogenesis
Two main effects of Bcl-3 on oncogenesis of solid tumors have been described: modulation of cell death and proliferation:
Cell death
One initial discovery suggested that one of the main oncogenic effects of Bcl-3 in hematopoietic malignancies is to increase survival in a subset of cells. Transgenic mice overexpressing the oncogene developed splenomegaly and presented increased mature B cells in lymph nodes and bone marrow [59]. Similar results were obtained from in vitro studies with T cells, [60–63]. The expansion of these cell compartments could be due to a decrease in cell death, by means of apoptosis inhibition and an increase in proliferation, discussed below [63]. Diminished cell death and its consequent increased cell number could provide an advantage to survival and mutation accumulation, as demonstrated in other models [64].
Less studied is the role of Bcl-3 in apoptosis inhibition of solid tumors. Initial reports showed that Bcl-3-p52 dimers are able to transactivate the antiapoptotic gene BCL2 in MCF7AZ breast cancer cells [65]. More important, it has been shown that, in breast cancer cells, DNA damage up regulates Bcl-3, which induces the expression of HDM2, the main negative regulator of p53 [66]. p53 is a tumor suppressor gene that, in response to DNA damage, arrests cell cycle and induces apoptosis. HDM2 in turn, inhibits both expression and activity of p53 [67]. It has also been shown in a variety of cancer cells that basal apoptosis is suppressed by Bcl-3 in a regulatory loop induced by JNK1 and suppressed by the related JNK2 [68]. It is interesting to note that this loop is not involved in suppressing basal cell apoptosis in non-cancerous cells, pointing toward a possible "gene addiction" role of Bcl-3. More recently, a new interaction partner of Bcl-3, CtBP1, was found in breast cancer cells [40]. Bcl-3 stabilizes CtBP1 by blocking its degradation by the proteasome and inhibiting apoptosis, leading to the sustained repression of pro-apoptotic gene expression and subsequent inhibition of apoptosis. Interestingly, expression of Bcl-3 and CtBP1 is strongly correlated in breast cancer samples.
Recently, we have reported that Bcl-3 is involved in an additional death pathway that is independent of apoptosis [69]. Cervical cell lines in which Bcl-3 is knocked-down by a specific shRNA arrested temporally in G2/M, presented a DNA damage response and enter unsuccessful mitosis cycles which ultimately leads to centrosome amplification, increased aneuploidy, leading to a clonogenic death. These results could imply that Bcl-3 participates in an oncogene addiction phenomenon, in which inactivation of this gene would specifically kill cancer cells overexpressing Bcl-3, as reported for other genes [70]. Further research is needed to elucidate the exact molecular basis for this response, since p53 is already downregulated in these cells by human papillomavirus E6 protein [71] and thus, an additional mechanism could be expected. In this regard, we have found that Bcl-3 regulates STAT3 in cervical cancer cells [20]. STAT3 is an important oncogene in solid tumors that, among other functions, regulates the DNA damage response [72–74]. It has been reported that Bcl-3 is induced by activation of STAT3 due to Epstein-Barr LMP1 oncoprotein [21] and also by granulocyte colony-stimulating factor [75]. On the other hand, we have shown that Bcl-3 depletion decreases STAT3 expression [69]. Since both genes are regulated by each other [21, 75], DNA damage may create an amplification loop that could be necessary for a correct cellular response. Forced expression or concomitant inhibition of both genes should provide an answer to this question.
Proliferation
The first evidence for the effects in cell growth came from the previously mentioned transgenic mice overexpressing Bcl-3 [59]. These finding were extended to hematological malignancies, such as multiple myeloma [12]. More evidence of effects in proliferation is known from solid tumor models. Westerheide, et al demonstrated in breast cancer cell lines that Bcl-3, acting as a coactivator of p52 dimers, induced the expression of cyclin D1, and thus, increased the transition at G1/S cell cycle phase [76]. In turn, it has been shown that p53 decreased the expression of Bcl-3 changing p52/Bcl-3 to p52/HDAC complexes in the cyclin D1 promoter, thus inhibiting cyclin expression [23]. In the skin, Bcl-3 participates in a signaling module downstream of CYLD [28]. CYLD is mutated in the human syndrome cylindromatosis, in which affected patients present benign tumors in skin adnexa. In these cases, mutated CYLD is unable to deubiquitinate Bcl-3, allowing increased proliferation in cell of the skin adnexa [28]. Adding to this, it has been shown that CYLD is downregulated by Snail in malignant melanomas [77]. This downregulation allowed the stabilization, nuclear localization and transcriptional activation of Bcl-3, enhancing proliferation and invasion of these cells. Finally, the role of Bcl-3 in skin/adnexal tumorigenesis is also supported by a mouse model of skin carcinogenesis in which Bcl-3 is strongly overexpressed in late papillomas and squamous cell carcinoma [78].
Conclusion
Bcl-3 is an established oncogene in hematologic malignancies, such as B-cell chronic lymphocytic leukemias. Nevertheless, recent research has shown that it also participates in progression of diverse solid tumors. As more information is available, it is clear that Bcl-3 is involved in central oncogenic pathways that regulate cell death and apoptosis, so it could be important as a target to validation as a diagnostic or prognostic marker in these tumors.
Abbreviations
- Bcl-3:
-
B-Cell Lymphoma 3
- NFkappa B:
-
Nuclear factor kappa-light-chain-enhancer of activated B cells
- TNF-α:
-
Tumor necrosis factor-α
- Lck:
-
lymphocyte-specific protein tyrosine kinase
- Jab1:
-
Jun Activation Domain Binding Protein 1
- Pirin:
-
iron-binding nuclear protein
- KAT5:
-
K(lysine) acetyltransferase 5
- Bard1:
-
BRCA1 associated RING domain 1
- B3BP:
-
Bcl-3 Binding Protein
- STAT3:
-
signal transducer and activator of transcription
- IL1-12:
-
Interleukin 1 to 12
- ERRalpha:
-
estrogen-related receptor alpha
- PGC-1a:
-
Peroxisome proliferator-activated receptor gamma coactivator 1-alpha
- CYLD:
-
cylindromatosis (turban tumor síndrome)
- CtBP1:
-
C-terminal-binding protein 1
- IRS3:
-
insulin receptor substrate 3
- GSK3:
-
Glycogen synthase kinase 3.
References
Bours V, Villalobos J, Burd PR, Kelly K, Siebenlist U: Cloning of a mitogen-inducible gene encoding a kappa B DNA-binding protein with homology to the rel oncogene and to cell-cycle motifs. Nature. 1990, 348 (6296): 76-80. 10.1038/348076a0
Ohno H, Takimoto G, McKeithan TW: The candidate proto-oncogene bcl-3 is related to genes implicated in cell lineage determination and cell cycle control. Cell. 1990, 60 (6): 991-997. 10.1016/0092-8674(90)90347-H
Tanaka S, Nishigaki H, Nakagawa H, Okuda T, Nishida K, Tsuda S, Taniwaki M, Imanishi H, Misawa S, Kashima K: Reciprocal t(14;19)(q32.3;q13.1) in a patient with B-cell lymphoma. Cancer Genet Cytogenet. 1990, 49 (2): 219-224. 10.1016/0165-4608(90)90144-Y
van Krieken JH, McKeithan TW, Raghoebier S, Medeiros LJ, Kluin PM, Raffeld M: Chromosomal translocation t(14;19) as indicated by bcl-3 rearrangement is a rare phenomenon in non-Hodgkin's lymphoma and chronic lymphocytic leukemia: a molecular genetic analysis of 176 cases. Leukemia. 1990, 4 (12): 811-812.
Kerr LD, Duckett CS, Wamsley P, Zhang Q, Chiao P, Nabel G, McKeithan TW, Baeuerle PA, Verma IM: The proto-oncogene bcl-3 encodes an I kappa B protein. Genes Dev. 1992, 6 (12A): 2352-2363. 10.1101/gad.6.12a.2352
Wulczyn FG, Naumann M, Scheidereit C: Candidate proto-oncogene bcl-3 encodes a subunit-specific inhibitor of transcription factor NF-kappa B. Nature. 1992, 358 (6387): 597-599. 10.1038/358597a0
Bours V, Franzoso G, Azarenko V, Park S, Kanno T, Brown K, Siebenlist U: The oncoprotein Bcl-3 directly transactivates through kappa B motifs via association with DNA-binding p50B homodimers. Cell. 1993, 72 (5): 729-739. 10.1016/0092-8674(93)90401-B
Franzoso G, Bours V, Azarenko V, Park S, Tomita-Yamaguchi M, Kanno T, Brown K, Siebenlist U: The oncoprotein Bcl-3 can facilitate NF-kappa B-mediated transactivation by removing inhibiting p50 homodimers from select kappa B sites. Embo J. 1993, 12 (10): 3893-3901.
Fujita T, Nolan GP, Liou HC, Scott ML, Baltimore D: The candidate proto-oncogene bcl-3 encodes a transcriptional coactivator that activates through NF-kappa B p50 homodimers. Genes Dev. 1993, 7 (7B): 1354-1363. 10.1101/gad.7.7b.1354
Inoue J, Takahara T, Akizawa T, Hino O: Bcl-3, a member of the I kappa B proteins, has distinct specificity towards the Rel family of proteins. Oncogene. 1993, 8 (8): 2067-2073.
Heissmeyer V, Krappmann D, Wulczyn FG, Scheidereit C: NF-kappaB p105 is a target of IkappaB kinases and controls signal induction of Bcl-3-p50 complexes. Embo J. 1999, 18 (17): 4766-4778. 10.1093/emboj/18.17.4766
Brenne AT, Fagerli UM, Shaughnessy JD, Vatsveen TK, Ro TB, Hella H, Zhan F, Barlogie B, Sundan A, Borset M: High expression of BCL3 in human myeloma cells is associated with increased proliferation and inferior prognosis. Eur J Haematol. 2009, 82 (5): 354-363. 10.1111/j.1600-0609.2009.01225.x
Rebollo A, Dumoutier L, Renauld JC, Zaballos A, Ayllon V, Martinez AC: Bcl-3 expression promotes cell survival following interleukin-4 deprivation and is controlled by AP1 and AP1-like transcription factors. Mol Cell Biol. 2000, 20 (10): 3407-3416. 10.1128/MCB.20.10.3407-3416.2000
Elliott SF, Coon CI, Hays E, Stadheim TA, Vincenti MP: Bcl-3 is an interleukin-1-responsive gene in chondrocytes and synovial fibroblasts that activates transcription of the matrix metalloproteinase 1 gene. Arthritis Rheum. 2002, 46 (12): 3230-3239. 10.1002/art.10675
Hu X, Nesic-Taylor O, Qiu J, Rea HC, Fabian R, Rassin DK, Perez-Polo JR: Activation of nuclear factor-kappaB signaling pathway by interleukin-1 after hypoxia/ischemia in neonatal rat hippocampus and cortex. J Neurochem. 2005, 93 (1): 26-37. 10.1111/j.1471-4159.2004.02968.x
Brocke-Heidrich K, Ge B, Cvijic H, Pfeifer G, Loffler D, Henze C, McKeithan TW, Horn F: BCL3 is induced by IL-6 via Stat3 binding to intronic enhancer HS4 and represses its own transcription. Oncogene. 2006, 25 (55): 7297-7304. 10.1038/sj.onc.1209711
Kuwata H, Watanabe Y, Miyoshi H, Yamamoto M, Kaisho T, Takeda K, Akira S: IL-10-inducible Bcl-3 negatively regulates LPS-induced TNF-alpha production in macrophages. Blood. 2003, 102 (12): 4123-4129. 10.1182/blood-2003-04-1228
Folco EJ, Rocha VZ, Lopez-Ilasaca M, Libby P: Adiponectin inhibits pro-inflammatory signaling in human macrophages independent of interleukin-10. J Biol Chem. 2009, 284 (38): 25569-25575. 10.1074/jbc.M109.019786
Valenzuela JO, Hammerbeck CD, Mescher MF: Cutting Edge: Bcl-3 Up-Regulation by Signal 3 Cytokine (IL-12) Prolongs Survival of Antigen-Activated CD8 T Cells. J Immunol. 2005, 174 (2): 600-604.
Maldonado V, Espinosa M, Pruefer F, Patino N, Ceballos-Canciono G, Urzua U, Juretic N, Melendez-Zajgla J: Gene regulation by BCL3 in a cervical cancer cell line. Folia Biol (Praha). 2010, 56 (4): 183-193.
Kung CP, Meckes DG, Raab-Traub N: Epstein-Barr virus LMP1 activates EGFR, STAT3, and ERK through effects on PKCdelta. J Virol. 2011, 85 (9): 4399-4408. 10.1128/JVI.01703-10
Brasier AR, Lu M, Hai T, Lu Y, Boldogh I: NF-kappa B-inducible BCL-3 expression is an autoregulatory loop controlling nuclear p50/NF-kappa B1 residence. J Biol Chem. 2001, 276 (34): 32080-32093. 10.1074/jbc.M102949200
Rocha S, Martin AM, Meek DW, Perkins ND: p53 represses cyclin D1 transcription through down regulation of Bcl-3 and inducing increased association of the p52 NF-kappaB subunit with histone deacetylase 1. Mol Cell Biol. 2003, 23 (13): 4713-4727. 10.1128/MCB.23.13.4713-4727.2003
Pabla R, Weyrich AS, Dixon DA, Bray PF, McIntyre TM, Prescott SM, Zimmerman GA: Integrin-dependent control of translation: engagement of integrin alphaIIbbeta3 regulates synthesis of proteins in activated human platelets. J Cell Biol. 1999, 144 (1): 175-184. 10.1083/jcb.144.1.175
Kraiss LW, Weyrich AS, Alto NM, Dixon DA, Ennis TM, Modur V, McIntyre TM, Prescott SM, Zimmerman GA: Fluid flow activates a regulator of translation, p70/p85 S6 kinase, in human endothelial cells. Am J Physiol Heart Circ Physiol. 2000, 278 (5): H1537-1544.
Viatour P, Dejardin E, Warnier M, Lair F, Claudio E, Bureau F, Marine JC, Merville MP, Maurer U, Green D: GSK3-mediated BCL-3 phosphorylation modulates its degradation and its oncogenicity. Mol Cell. 2004, 16 (1): 35-45. 10.1016/j.molcel.2004.09.004
Garate M, Wani AA, Li G: The NAD(P)H:Quinone Oxidoreductase 1 induces cell cycle progression and proliferation of melanoma cells. Free Radic Biol Med. 2010, 48 (12): 1601-1609. 10.1016/j.freeradbiomed.2010.03.003
Massoumi R, Chmielarska K, Hennecke K, Pfeifer A, Fassler R: Cyld inhibits tumor cell proliferation by blocking Bcl-3-dependent NF-kappaB signaling. Cell. 2006, 125 (4): 665-677. 10.1016/j.cell.2006.03.041
Keutgens A, Shostak K, Close P, Zhang X, Hennuy B, Aussems M, Chapelle JP, Viatour P, Gothot A, Fillet M: The repressing function of the oncoprotein BCL-3 requires CtBP, while its polyubiquitination and degradation involve the E3 ligase TBLR1. Mol Cell Biol. 2010, 30 (16): 4006-4021. 10.1128/MCB.01600-09
Keutgens A, Zhang X, Shostak K, Robert I, Olivier S, Vanderplasschen A, Chapelle JP, Viatour P, Merville MP, Bex F: BCL-3 degradation involves its polyubiquitination through a FBW7-independent pathway and its binding to the proteasome subunit PSMB1. J Biol Chem. 2010, 285 (33): 25831-25840. 10.1074/jbc.M110.112128
Guan Y, Yao H, Zheng Z, Qiu G, Sun K: MiR-125b targets BCL3 and suppresses ovarian cancer proliferation. Int J Cancer. 2011, 128 (10): 2274-2283. 10.1002/ijc.25575
Wickstrom SA, Masoumi KC, Khochbin S, Fassler R, Massoumi R: CYLD negatively regulates cell-cycle progression by inactivating HDAC6 and increasing the levels of acetylated tubulin. Embo J. 2010, 29 (1): 131-144. 10.1038/emboj.2009.317
Franzoso G, Bours V, Park S, Tomita-Yamaguchi M, Kelly K, Siebenlist U: The candidate oncoprotein Bcl-3 is an antagonist of p50/NF-kappa B-mediated inhibition. Nature. 1992, 359 (6393): 339-342. 10.1038/359339a0
Watanabe N, Iwamura T, Shinoda T, Fujita T: Regulation of NFKB1 proteins by the candidate oncoprotein BCL-3: generation of NF-kappaB homodimers from the cytoplasmic pool of p50-p105 and nuclear translocation. Embo J. 1997, 16 (12): 3609-3620. 10.1093/emboj/16.12.3609
Caamano JH, Perez P, Lira SA, Bravo R: Constitutive expression of Bc1-3 in thymocytes increases the DNA binding of NF-kappaB1 (p50) homodimers in vivo. Mol Cell Biol. 1996, 16 (4): 1342-1348.
Andrews N, Helliwell T, Walker C, Jones AS: Differing expression of bax and bcl-3 may influence the different cure rates in mouth and orophayrngeal cancer. Clin Otolaryngol. 2000, 25 (6): 570-576.
Watanabe N, Wachi S, Fujita T: Identification and characterization of BCL-3-binding protein: implications for transcription and DNA repair or recombination. J Biol Chem. 2003, 278 (28): 26102-26110. 10.1074/jbc.M303518200
Zhao Y, Ramakrishnan A, Kim KE, Rabson AB: Regulation of Bcl-3 through interaction with the Lck tyrosine kinase. Biochem Biophys Res Commun. 2005, 335 (3): 865-873. 10.1016/j.bbrc.2005.07.162
Yang J, Williams RS, Kelly DP: Bcl3 interacts cooperatively with peroxisome proliferator-activated receptor gamma (PPARgamma) coactivator 1alpha to coactivate nuclear receptors estrogen-related receptor alpha and PPARalpha. Mol Cell Biol. 2009, 29 (15): 4091-4102. 10.1128/MCB.01669-08
Choi HJ, Lee JM, Kim H, Nam HJ, Shin HJ, Kim D, Ko E, Noh DY, Kim KI, Kim JH: Bcl3-dependent stabilization of CtBP1 is crucial for the inhibition of apoptosis and tumor progression in breast cancer. Biochem Biophys Res Commun. 2010, 400 (3): 396-402. 10.1016/j.bbrc.2010.08.084
Kabuta T, Hakuno F, Cho Y, Yamanaka D, Chida K, Asano T, Wada K, Takahashi S: Insulin receptor substrate-3, interacting with Bcl-3, enhances p50 NF-kappaB activity. Biochem Biophys Res Commun. 2010, 394 (3): 697-702. 10.1016/j.bbrc.2010.03.054
Chan KK, Shen L, Au WY, Yuen HF, Wong KY, Guo T, Wong ML, Shimizu N, Tsuchiyama J, Kwong YL: Interleukin-2 induces NF-kappaB activation through BCL10 and affects its subcellular localization in natural killer lymphoma cells. J Pathol. 2010, 221 (2): 164-174. 10.1002/path.2699
Au WY, Horsman DE, Ohno H, Klasa RJ, Gascoyne RD: Bcl-3/IgH translocation (14;19)(q32;q13) in non-Hodgkin's lymphomas. Leuk Lymphoma. 2002, 43 (4): 813-816. 10.1080/10428190290016935
Canoz O, Rassidakis GZ, Admirand JH, Medeiros LJ: Immunohistochemical detection of BCL-3 in lymphoid neoplasms: a survey of 353 cases. Mod Pathol. 2004, 17 (8): 911-917. 10.1038/modpathol.3800140
Schlette E, Rassidakis GZ, Canoz O, Medeiros LJ: Expression of bcl-3 in chronic lymphocytic leukemia correlates with trisomy 12 and abnormalities of chromosome 19. Am J Clin Pathol. 2005, 123 (3): 465-471. 10.1309/6Q27Q3NDGV8LW1BU
Cogswell PC, Guttridge DC, Funkhouser WK, Baldwin AS: Selective activation of NF-kappa B subunits in human breast cancer: potential roles for NF-kappa B2/p52 and for Bcl-3. Oncogene. 2000, 19 (9): 1123-1131. 10.1038/sj.onc.1203412
Thornburg NJ, Pathmanathan R, Raab-Traub N: Activation of nuclear factor-kappaB p50 homodimer/Bcl-3 complexes in nasopharyngeal carcinoma. Cancer Res. 2003, 63 (23): 8293-8301.
Pallares J, Martinez-Guitarte JL, Dolcet X, Llobet D, Rue M, Palacios J, Prat J, Matias-Guiu X: Abnormalities in the NF-kappaB family and related proteins in endometrial carcinoma. J Pathol. 2004, 204 (5): 569-577. 10.1002/path.1666
Rayet B, Gelinas C: Aberrant rel/nfkb genes and activity in human cancer. Oncogene. 1999, 18 (49): 6938-6947. 10.1038/sj.onc.1203221
Karin M, Cao Y, Greten FR, Li ZW: NF-kappaB in cancer: from innocent bystander to major culprit. Nat Rev Cancer. 2002, 2 (4): 301-310. 10.1038/nrc780
Ben-Neriah Y, Karin M: Inflammation meets cancer, with NF-kappaB as the matchmaker. Nat Immunol. 2011, 12 (8): 715-723. 10.1038/ni.2060
Hovelmeyer N, Wunderlich FT, Massoumi R, Jakobsen CG, Song J, Worns MA, Merkwirth C, Kovalenko A, Aumailley M, Strand D: Regulation of B cell homeostasis and activation by the tumor suppressor gene CYLD. J Exp Med. 2007, 204 (11): 2615-2627. 10.1084/jem.20070318
Forbes SA, Bindal N, Bamford S, Cole C, Kok CY, Beare D, Jia M, Shepherd R, Leung K, Menzies A: COSMIC: mining complete cancer genomes in the Catalogue of Somatic Mutations in Cancer. Nucleic Acids Res. 2011, D945-950. 39 Database,
Romieu-Mourez R, Kim DW, Shin SM, Demicco EG, Landesman-Bollag E, Seldin DC, Cardiff RD, Sonenshein GE: Mouse mammary tumor virus c-rel transgenic mice develop mammary tumors. Mol Cell Biol. 2003, 23 (16): 5738-5754. 10.1128/MCB.23.16.5738-5754.2003
Pratt MA, Bishop TE, White D, Yasvinski G, Menard M, Niu MY, Clarke R: Estrogen withdrawal-induced NF-kappaB activity and bcl-3 expression in breast cancer cells: roles in growth and hormone independence. Mol Cell Biol. 2003, 23 (19): 6887-6900. 10.1128/MCB.23.19.6887-6900.2003
Paine E, Scheinman RI, Baldwin AS, Raab-Traub N: Expression of LMP1 in epithelial cells leads to the activation of a select subset of NF-kappa B/Rel family proteins. J Virol. 1995, 69 (7): 4572-4576.
Miller WE, Earp HS, Raab-Traub N: The Epstein-Barr virus latent membrane protein 1 induces expression of the epidermal growth factor receptor. J Virol. 1995, 69 (7): 4390-4398.
Puvvada SD, Funkhouser WK, Greene K, Deal A, Chu H, Baldwin AS, Tepper JE, O'Neil BH: NF-kB and Bcl-3 activation are prognostic in metastatic colorectal cancer. Oncology. 2010, 78 (3-4): 181-188. 10.1159/000313697
Ong ST, Hackbarth ML, Degenstein LC, Baunoch DA, Anastasi J, McKeithan TW: Lymphadenopathy, splenomegaly, and altered immunoglobulin production in BCL3 transgenic mice. Oncogene. 1998, 16 (18): 2333-2343. 10.1038/sj.onc.1201771
Rangelova S, Kirschnek S, Strasser A, Hacker G: FADD and the NF-kappaB family member Bcl-3 regulate complementary pathways to control T-cell survival and proliferation. Immunology. 2008, 125 (4): 549-557. 10.1111/j.1365-2567.2008.02869.x
Mitchell TC, Teague TK, Hildeman DA, Bender J, Rees WA, Kedl RM, Swanson B, Kappler JW, Marrack P: Stronger correlation of bcl-3 than bcl-2, bcl-xL, costimulation, or antioxidants with adjuvant-induced T cell survival. Ann N Y Acad Sci. 2002, 975: 114-131. 10.1111/j.1749-6632.2002.tb05946.x
Mitchell TC, Thompson BS, Trent JO, Casella CR: A short domain within Bcl-3 is responsible for its lymphocyte survival activity. Ann N Y Acad Sci. 2002, 975: 132-147. 10.1111/j.1749-6632.2002.tb05947.x
Bauer A, Villunger A, Labi V, Fischer SF, Strasser A, Wagner H, Schmid RM, Hacker G: The NF-kappaB regulator Bcl-3 and the BH3-only proteins Bim and Puma control the death of activated T cells. Proc Natl Acad Sci USA. 2006, 103 (29): 10979-10984. 10.1073/pnas.0603625103
Baguley BC: The paradox of cancer cell apoptosis. Front Biosci. 2011, 16: 1759-1767. 10.2741/3819
Viatour P, Bentires-Alj M, Chariot A, Deregowski V, de Leval L, Merville MP, Bours V: NF- kappa B2/p100 induces Bcl-2 expression. Leukemia. 2003, 17 (7): 1349-1356. 10.1038/sj.leu.2402982
Kashatus D, Cogswell P, Baldwin AS: Expression of the Bcl-3 proto-oncogene suppresses p53 activation. Genes Dev. 2006, 20 (2): 225-235. 10.1101/gad.1352206
Meek DW: Tumour suppression by p53: a role for the DNA damage response?. Nat Rev Cancer. 2009, 9: 714-723.
Ahmed SU, Milner J: Basal cancer cell survival involves JNK2 suppression of a novel JNK1/c-Jun/Bcl-3 apoptotic network. PLoS One. 2009, 4 (10): e7305- 10.1371/journal.pone.0007305
Zamora R, Espinosa M, Ceballos-Cancino G, Segura B, Maldonado V, Melendez-Zajgla J: Depletion of the oncoprotein Bcl-3 induces centrosome amplification and aneuploidy in cancer cells. Mol Cancer. 2010, 9: 223- 10.1186/1476-4598-9-223
Weinstein IB, Joe A: Oncogene addiction. Cancer Res. 2008, 68: 3077-3080. discussion 3080, 10.1158/0008-5472.CAN-07-3293
Lagunas-Martinez A, Madrid-Marina V, Gariglio P: Modulation of apoptosis by early human papillomavirus proteins in cervical cancer. Biochim Biophys Acta. 2010, 1805 (1): 6-16.
Barry SP, Townsend PA, Knight RA, Scarabelli TM, Latchman DS, Stephanou A: STAT3 modulates the DNA damage response pathway. Int J Exp Pathol. 2010, 91 (6): 506-514. 10.1111/j.1365-2613.2010.00734.x
Courapied S, Sellier H, de Carne Trecesson S, Vigneron A, Bernard AC, Gamelin E, Barre B, Coqueret O: The cdk5 kinase regulates the STAT3 transcription factor to prevent DNA damage upon topoisomerase I inhibition. J Biol Chem. 2010, 285 (35): 26765-26778. 10.1074/jbc.M109.092304
Bito T, Sumita N, Masaki T, Shirakawa T, Ueda M, Yoshiki R, Tokura Y, Nishigori C: Ultraviolet light induces Stat3 activation in human keratinocytes and fibroblasts through reactive oxygen species and DNA damage. Experimental dermatology. 2010, 19 (7): 654-660. 10.1111/j.1600-0625.2010.01084.x
Kreisel D, Sugimoto S, Tietjens J, Zhu J, Yamamoto S, Krupnick AS, Carmody RJ, Gelman AE: Bcl3 prevents acute inflammatory lung injury in mice by restraining emergency granulopoiesis. J Clin Invest. 2011, 121 (1): 265-276. 10.1172/JCI42596
Westerheide SD, Mayo MW, Anest V, Hanson JL, Baldwin AS: The putative oncoprotein Bcl-3 induces cyclin D1 to stimulate G(1) transition. Mol Cell Biol. 2001, 21 (24): 8428-8436. 10.1128/MCB.21.24.8428-8436.2001
Massoumi R, Kuphal S, Hellerbrand C, Haas B, Wild P, Spruss T, Pfeifer A, Fassler R, Bosserhoff AK: Down-regulation of CYLD expression by Snail promotes tumor progression in malignant melanoma. J Exp Med. 2009, 206 (1): 221-232. 10.1084/jem.20082044
Budunova IV, Perez P, Vaden VR, Spiegelman VS, Slaga TJ, Jorcano JL: Increased expression of p50-NF-kappaB and constitutive activation of NF-kappaB transcription factors during mouse skin carcinogenesis. Oncogene. 1999, 18 (52): 7423-7431. 10.1038/sj.onc.1203104
Szklarczyk D, Franceschini A, Kuhn M, Simonovic M, Roth A, Minguez P, Doerks T, Stark M, Muller J, Bork P: The STRING database in 2011: functional interaction networks of proteins, globally integrated and scored. Nucleic Acids Res. 2011, D561-568. 39 Database,
Arnold K, Bordoli L, Kopp J, Schwede T: The SWISS-MODEL workspace: a web-based environment for protein structure homology modelling. Bioinformatics. 2006, 22 (2): 195-201. 10.1093/bioinformatics/bti770
Sun L, Hui AM, Su Q, Vortmeyer A, Kotliarov Y, Pastorino S, Passaniti A, Menon J, Walling J, Bailey R: Neuronal and glioma-derived stem cell factor induces angiogenesis within the brain. Cancer Cell. 2006, 9 (4): 287-300. 10.1016/j.ccr.2006.03.003
Finak G, Bertos N, Pepin F, Sadekova S, Souleimanova M, Zhao H, Chen H, Omeroglu G, Meterissian S, Omeroglu A: Stromal gene expression predicts clinical outcome in breast cancer. Nat Med. 2008, 14 (5): 518-527. 10.1038/nm1764
Welsh JB, Zarrinkar PP, Sapinoso LM, Kern SG, Behling CA, Monk BJ, Lockhart DJ, Burger RA, Hampton GM: Analysis of gene expression profiles in normal and neoplastic ovarian tissue samples identifies candidate molecular markers of epithelial ovarian cancer. Proc Natl Acad Sci USA. 2001, 98 (3): 1176-1181. 10.1073/pnas.98.3.1176
Korkola JE, Houldsworth J, Chadalavada RS, Olshen AB, Dobrzynski D, Reuter VE, Bosl GJ, Chaganti RS: Down-regulation of stem cell genes, including those in a 200-kb gene cluster at 12p13.31, is associated with in vivo differentiation of human male germ cell tumors. Cancer Res. 2006, 66 (2): 820-827. 10.1158/0008-5472.CAN-05-2445
Acknowledgements
JM-Z work is supported by CONACyT's grants 132931, 87855 and 132931.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
JM-Z wrote the first draft, VM contributed with specific sections, JM-Z and VM reviewed the manuscript and wrote the final version. Both authors read and approved the final manuscript.
Electronic supplementary material
12943_2011_975_MOESM1_ESM.JPEG
Additional file 1: Structure prediction of mutated Bcl-3 proteins found in COSMIC database. Bcl-3 sequence was retrieved from NCBI and mutation data from COSMIC. Proteins were modeled using SWISS-MODEL structure-homology server [80]. A) Bcl-3 wild type structure B) Bcl-3 pP420A mutant from a lung cancer sample C) Bcl-3 p.R145W mutant from an ovary cancer sample. (JPEG 210 KB)
12943_2011_975_MOESM2_ESM.JPEG
Additional file 2: Overexpression of Bcl-3 in different tumor types. Oncomine™ (Compendia Bioscience, Ann Arbor, MI) Expression Arrays Database was used for analysis and visualization. A) Overexpression in Glioblastoma (180 samples) from Su, et. al.[81]. P-value in T test 1.44-9 with a fold change of 3.307. Light blue (number 1) represents normal brain controls. Dark blue (number 2) are cancer samples. B) Overexpression in Breast Cancer from Finak, et. al. [82] (59 samples). P-value in T test 7.10-15 with a fold change of 2.266. Light blue (number 1) represents normal breast controls. Dark blue (number 2) are cancer samples. C) Overexpression in ovarian cancer (32 samples) from Welsh, et. al. [83]. P-value in T test 6.04-8 with a fold change of 23.955. Light blue (number 1) represents normal ovary controls. Dark blue (number 2) are cancer samples. D) Overexpression in teratomas from Korkola, et. al. [84] (20 samples). P-value in T test 6.64-10 with a fold change of 11.591. Light blue (number 1) represents normal testis controls. Dark blue (number 2) are cancer samples. E) Overexpression in embryonal carcinomas (21 samples) from Korkola, et. al. [84]. P-value in T test 2.22-6 with a fold change of 2.295. Light blue (number 1) represents normal testis controls. Dark blue (number 2) are cancer samples. (JPEG 235 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Maldonado, V., Melendez-Zajgla, J. Role of Bcl-3 in solid tumors. Mol Cancer 10, 152 (2011). https://doi.org/10.1186/1476-4598-10-152
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1476-4598-10-152