Abstract
Background
This study aimed to determine the age-specific aetiologic agents of diarrhoea in children aged less than five years. The study also assessed the efficacy of the empiric treatment of childhood diarrhoea using Integrated Management of Childhood Illness (IMCI) guidelines.
Methods
This study included 280 children aged less than 5 years, admitted with diarrhoea to any of the four major hospitals in Dar es Salaam. Bacterial pathogens were identified using conventional methods. Enzyme Linked Immunosorbent Assay (ELISA) and agglutination assay were used to detect viruses and intestinal protozoa, respectively. Antimicrobial susceptibility was determined using Kirby-Bauer disk diffusion method.
Results
At least one of the searched pathogens was detected in 67.1% of the cases, and mixed infections were detected in 20.7% of cases. Overall, bacteria and viruses contributed equally accounting for 33.2% and 32.2% of all the cases, respectively, while parasites were detected in 19.2% patients. Diarrhoeagenic Escherichia coli (DEC) was the most common enteric pathogen, isolated in 22.9% of patients, followed by Cryptosporidium parvum (18.9%), rotavirus (18.1%) and norovirus (13.7%). The main cause of diarrhoea in children aged 0 to 6 months were bacteria, predominantly DEC, while viruses predominated in the 7-12 months age group. Vibrio cholerae was isolated mostly in children above two years. Shigella spp, V. cholerae and DEC showed moderate to high rates of resistance to erythromycin, ampicillin, chloramphenicol and tetracycline (56.2-100%). V. cholerae showed full susceptibility to co-trimoxazole (100%), while DEC and Shigella showed high rate of resistance to co-trimoxazole; 90.6% and 93.3% respectively. None of the bacterial pathogens isolated showed resistance to ciprofloxacin which is not recommended for use in children. Cefotaxime resistance was found only in 4.7% of the DEC.
Conclusion
During the dry season, acute watery diarrhoea is the most common type of diarrhoea in children under five years in Dar es Salaam and is predominantly due to DEC, C. parvum, rotaviruses and noroviruses. Constant antibiotic surveillance is warranted as bacteria were highly resistant to various antimicrobial agents including co-trimoxazole and erythromycin which are currently recommended for empiric treatment of diarrhoea.
Similar content being viewed by others
Background
Infective diarrhoea is one of the leading cause of morbidity and mortality among children under five years in the developing world [1] and can be caused by a wide range of viruses, bacteria, or parasites [2, 3]. The prevalence of the different enteric pathogens varies with the geographical area [2].
There are relatively few studies on this aspect that have been conducted in Tanzania. Most of these studies have focused on few aetiological agents of diarrhoea and were conducted in late eighties and early nineties [4–6]. There is one recent study conducted in Ifakara, Tanzania in 2004, which shows the prevalence of different aetiological agents of diarrhoea, i.e. viruses, bacteria and parasites among children with diarrhoea. In that study diarrhoeagenic Escherichia coli (DEC) was the predominant enteropathogen. Moreover, Shigella spp. and rotavirus were more prevalent in the dry season than in the rainy season and Giardia lamblia was more prevalent in the rainy season [7].
For quite some time children with diarrhoea in Tanzania have been and are being treated empirically with erythromycin and co-trimoxazole according to the Integrated Management of Childhood Illness (IMCI) guidelines [8]. However current information regarding antimicrobial susceptibility pattern of bacteria causing diarrhoea in children is limited and thus it is uncertain whether the recommended antibiotics are still effective.
The present study aimed at detection of enteric pathogens in children with diarrhoea to provide an update on the spectrum and age specific causes of diarrhoea. The study also determined the antimicrobial resistance pattern of bacterial pathogens.
Methods
Study design and settings
This cross-sectional study was conducted in Dar es Salaam, Tanzania between December 2005 and February 2006. Participants were children ≤5 years, who during the study period, were admitted due to diarrhoea at Muhimbili National Referral Hospital (MNH), Amana, Mwananyamala and Temeke Municipal Hospitals in Dar es Salaam, Tanzania. Enrolment was subjected to obtaining an informed verbal consent from parent or guardian who accompanied the child.
Interviews
A structured questionnaire was used to obtain information of the children from the parents/guardians regarding age, sex, duration and description of the stool (watery, mucoid, or bloody) and the use of antibiotics prior to hospitalization. The definition and forms of diarrhoea were according to WHO guidelines [8].
Weight measurements
On admission infants less than two years of age were weighed using a 25 kg Salter hanging scales (CMS Weighing equipment, High Holborn, London, United Kingdom). Children over two years were weighed on scales calibrated before each session. Weight of children was recorded to the nearest kilogram.
Determination of nutritional status
Weight-for age Z-scores were calculated using EPI Info (USD, Inc., Stone Mountain, GA). According to WHO criteria children were considered to be undernourished if the Z-scores were less than -2SD[9].
Collection and transportation of stool
Stool specimens were collected using wide mouthed sterile plastic containers and transported to the Microbiology laboratory at Muhimbili National Hospital within two hours of collection. A portion of specimen was stored at -20°C until further analysis at Haukeland University Hospital in Bergen, Norway.
Isolation and identification of bacteria pathogens
Bacterial pathogens E. coli, V. cholerae, Salmonella spp and Shigella spp. were isolated and identified by conventional methods [10]. Identification of DEC was done as previously described [11].
Antimicrobial susceptibility testing of bacterial isolates
Susceptibility testing was performed by disk diffusion method according to Clinical and Laboratory Standards Institute guidelines (CLSI) [12]. Escherichia coli ATCC 25922 was used as a reference control strain. Antibiotics tested were ampicillin 10 μg, amoxycillin and clavulanic acid (Augmentin) 20/10 μg, erythromycin 15 μg, ciprofloxacin 100 μg, gentamicin 10 μg, cefotaxime 30 μg, cephalothin 30 μg, co-trimoxazole 25 μg, chloramphenicol 30 μg and tetracycline 30 μg (Remel, Lenexa, USA).
According to the size of the zones of inhibition, the organisms were classified as sensitive, intermediate or resistant to a specific antibiotic according to CLSI guidelines [12]. For the purpose of this study intermediate sensitivity was considered as sensitive.
Detection of viruses
The presence of four enteric viruses: rotavirus, norovirus, adenovirus and astrovirus were detected by commercially available enzyme linked immunosorbent assay (ELISA) according to manufacturer's instructions (Dako Ltd., Ely, United Kingdom). The tests detected specific antigens for group A rotaviruses, norovirus, adenoviruses type 40 and 41 and astroviruses, respectively.
Detection of intestinal protozoa Cryptosporidium parvum and Giardia lamblia
The presence of C. parvum and G. lamblia antigens was tested from frozen stool samples using ImmunoCard STAT! Rapid Assay (Meridian Bioscience, Belgium). This test simultaneously detects and distinguishes between C. parvum and G. lamblia antigens in aqueous extracts of patient stool specimens.
Ethical considerations
Ethical clearance was obtained from the Institutional Review Board of MUHAS, Dar es Salaam. Informed verbal consent was obtained from parents/guardians of the children before enrolment. Children were treated according to IMCI guidelines [8].
Data analysis
The Statistical Package for the Social Sciences (SPSS for windows, version 10.0) was used for statistical analysis. Assuming the data follows a normal distribution, comparison of proportions and statistical significance were tested by using the Chi-square test. A p value less than 0.05 was considered statistically significant.
Results
A total of 280 children (172 boys and 108 girls) aged 0-60 months with diarrhoea were enrolled. Of these 148(52.9%) were from Amana Hospital followed by MNH 47(16.8%), Temeke Hospital 47(16.8%) and Mwananyamala Hospital 38 (13.6%) (Table 1).
Two hundred and thirty five (83.9%) children presented mainly with acute watery followed by persistent diarrhoea in 27 (9.6%), while 28 (6.4%) had dysentery. Of the 51 children aged below six months, only six (11.8%) were exclusively breast-fed. About 97% of the children aged 7 to 12 months were still being breast-fed. Seventy nine children (28.2%) were malnourished.
At least one enteric pathogen was detected in 188 (67.1%) patients. Of these 93 (33.2%), 87 (32.2%) and 52 (19.2%) were bacteria, viruses and parasites respectively. Mixed infections with up to four different pathogens were detected in 56 (20.7%) of all cases. Most (75.9%) of the co-infections were with two pathogens, followed by three pathogens (20.4%) and a few (3.7%) were with four pathogens.
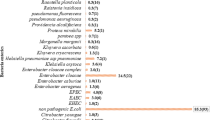
The prevalence of different enteric pathogens is shown in Table 2. DEC was the most common pathogen, isolated in 64 children (22.9%), followed by C. parvum detected in 51 (18.9%), rotavirus in 49 (18.1%) and norovirus in 37 (13.7%). V. cholerae and Shigella spp accounted for 5.7% and 5.4% of all cases of diarrhoea respectively. Of the DEC strains detected, 41(64.1%), 13(20.3%) and 10(15.6%) were EAEC, EPEC and ETEC respectively. All ETEC strains harboured only the stable toxin. There were no EIEC or EHEC detected in this group.
All V. cholerae isolates were sero group OI strains of Ogawa. Of the seven Salmonella isolated, four were Salmonella Typhimurium, two were Salmonella Enteritidis and one was Salmonella Typhi. Salmonella Paratyphi was not detected. Of the fifteen Shigella isolates, 10 were Shigella flexneri and five were Shigella dysenteriae. Shigella sonnei and Shigella boydii were not detected.
Table 3 shows that bacteria, viruses, parasites and mixed infection were highly prevalent in young infants aged 0-6 months (25.0%-56.8%) and 7-12 months (26.1%-52.3%) (p > 0.05), the prevalence of all pathogens decreasing with increasing age. When stratifying bacterial pathogens with age groups, DEC, was significantly higher (39.2%) in the age group of 0-6 months than the rest of the age groups (p = 0.01) while V. cholerae was significantly higher in older children >25 months (p = 0.01).
Overall, 86.2% - 97.4% of all the pathogens caused acute watery diarrhoea, with the exception of Shigella species which accounted for 40% of cases of dysentery (p < 0.05). Thirty-five (85.4%) of the 41 children with EAEC presented with acute watery diarrhoea, while five (12.2%) and one (2.4%) presented with persistent diarrhoea and dysentery respectively. Among children harbouring EPEC, ten (76.9%) had acute watery and three (23.1%) had persistent diarrhoea. Six (60.0%), two (20.0%) and two (20.0%) of the children with ETEC had acute watery diarrhoea, persistent diarrhoea and dysentery, respectively. Among the 92 children with diarrhoea whose aetiogical agents could not be detected; 87(94.6%) and 5(5.4%) presented with acute and persistent diarrhoea respectively.
Table 4 summarizes the antimicrobial resistance pattern of different bacterial pathogens. Overall, bacterial pathogens isolated showed no resistance to ciprofloxacin and cefotaxime except for DEC which showed 4.7% resistance to cefotaxime. Shigella spp, V. cholerae and DEC showed moderate to high rates of resistance to erythromycin, ampicillin, chloramphenicol and tetracycline (56.2-100%). V. cholerae showed full susceptibility to co-trimoxazole (100%), while DEC and Shigella spp showed high rate of resistance to co-trimoxazole; 90.6% and 93.3% respectively.
Discussion
In this study the prevalence of diarrhoea with an identified aetiology was 67.1% and consistent with previous findings from Ifakara, Tanzania [7]. Pathogens were not detected in 92(32.9%) of the children. This could be partly due to potential enteric pathogens such as helminths, Campylobacter spp, Yersinia enterocolitica and Aeromonas spp which were not searched for, or because of the fact that some of the children had a history of antibiotic use prior to admission.
We found bacterial pathogens in 33.3%, enteric viruses in 32.2% and the protozoas in 19.2% of patients. However when age stratification was done, the main cause of diarrohea in children aged 0-6 months were bacteria, predominantly DEC, while diarrhoea in children aged 7-12 months was more often due to viruses, mainly rotavirus and norovirus. Vibrio cholerae was isolated mainly in children aged above two. This age related pattern of pathogens is consistent with reports from studies conducted in other developing countries [2] and should be taken into account when considering appropriate management of childhood diarrhoea in Dar es Salaam.
Fifty six children (20.7%) had multiple infections with up to four associated pathogens, a figure comparable with findings in other developing countries [13, 14]. Dual infections raise the question of whether a single pathogen is responsible for illness, or whether several pathogens act in synergy. Further studies must be performed in order to obtain a better understanding of these infections. The predominance of DEC (64.1%) among all bacterial isolates is consistent with previous reports from Tanzania and other developing countries [7, 15], underlining their importance as the main bacterial causes of diarrhoea in children aged less than five years and the need to type them in order to know the types that cause diarrhoea in our setting.
Surprisingly, viruses were detected in four children with dysentery. One them had mixed infection with ETEC strain of DEC while the other three had no bacteria detected. Viruses do not normally cause bloody diarrhoea, the possible reason for this finding could be that enteric bacteria such as Shigella spp were not isolated because all the four children had history of taking antibiotics prior to the study or dysentery could have been caused by other enteric pathogens such Entamoeba histolytica which was not searched for in this study.
Overall, Shigella spp were detected in 5.7% of cases of diarrhoea but the frequency was significantly higher (40%) in children with bloody diarrhoea. The predominance of S. flexneri (66.7% of Shigella isolates) found in this study is consistent with the finding in Ifakara Tanzania [7].
The prevalence of Salmonella spp found in this study (5.7%) falls within the reported range of 1-5% of gastroenteritis cases in most developing countries [8] and the serotypes were mainly S. Enteritidis (28.6%) and S. Typhimurium (57.1%).
The high prevalence V. cholerae in the present study (5.7%) was due to an outbreak of cholera in the city during the time of study.
The prevalence of cryptosporidiosis reported in this study (18.9%) is higher than the 8.5% reported previously in Dar es Salaam [6]. The difference could be due to difference in HIV prevalence during the two study periods given the association between cryptosporidiosis and HIV infection [6]. However we did not screen for HIV infection in the current study. The difference could also be due to different methods used for detection of cryptosporidiosis. We found G. lamblia in only a minority of diarrhoea cases (1.9%), probably due to their limited role in childhood diarrhoea among children of Dar es Salaam.
We found no relationship between the enteric pathogens detected and the lack of exclusive breast feeding. This could be due to the fact that only a few children (11.2%) were exclusively breast-fed.
Our findings show that most bacterial pathogens isolated were sensitive to ciprofloxacin, cefotaxime, gentamicin, amoxicillin-clavulanic acid and cephalothin, probably due to their seldom use [16–19]. On the contrary, high rate of resistance was seen in commonly prescribed antibiotics such as ampicillin, tetracycline, including co-trimoxazole which are currently recommended for empirical treatment [8]. The high rate of resistance towards these antibiotics may be due to their overuse because they are readily available over the counter. The 4.7% prevalence of resistance of DEC to cefotaxime is noteworthy because third generation cephalosporin resistance is usually caused by expression of extended-spectrum beta-lactamase (ESBL) enzymes which may be the case in these strains although specific detection of ESBL production was not performed. ESBL producing-strains have been reported previously in septicaemic as well as Intensive Care Unit patients from Muhimbili National Hospital [20, 21].
The antimicrobial resistance of V. cholerae observed in this study when compared with those of Urrasa et al [17] does show an increase in rate the of resistance to ampicillin (17% and 53.4% in 1997 and 1999 respectively versus 75% in the present study), erythromycin (18.1% and 54% in 1997 and 1999 respectively versus 75%) and tetracycline (6.45 and 41.1%% in 1997 and 1999 respectively versus 93.7%). The study also found a decrease in the rate of resistance to co-trimoxazole (96.8% and 96.6% in 1997 and 1999 respectively versus 0% in the present study). The low rate of resistance of V. cholerae to co-trimoxazole supports the current national policy of treating cholera with co-trimoxazole. However there is a need for continuous surveillance to monitor and track potential development of resistance.
Conclusions
During the dry season, acute watery diarrhoea is the most common type of diarrhoea in children under five years in Dar es Salaam and is predominantly due to DEC, C. parvum, rotaviruses and noroviruses. High rate of resistance of bacteria to co-trimoxazole and erythromycin which are currently recommended for empiric treatment of diarrhoea and other antimicrobial agents, calls for continued antibiotic surveillance.
References
Bern C, Martines J, de Zoysa I, Glass RI: The magnitude of the global problem of diarrhoeal disease: a ten-year update. Bull World Health Organ. 1992, 70: 705-714.
Guerrant RL, Hughes JM, Lima NL, Crane J: Diarrhoea in developed and developing countries: magnitude, special settings, and etiologies. Rev infect Dis. 1990, 12: S41-50.
Gracey M: Diarrhoea and malnutrition: a challenge for pediatricians. J Pediatr Gastroenterol Nutr. 22: 6-16. 10.1097/00005176-199601000-00004.
Mhalu FS, Myrmel H, Msengi A, Haukenes G: Prevalence of infection with rotavirus and enteric adenoviruses among children in Tanzania. NIPH Ann. 1988, 11: 3-7.
Sam NE, Haukenes G, Szilvay AM, Mhalu F: Rotavirus infection in Tanzania: a virological, epidemiological and clinical study among young children. Apmis. 1992, 100: 790-796. 10.1111/j.1699-0463.1992.tb04001.x.
Cegielski JP, Msengi AE, Dukes CS, Mbise R, Redding-Lallinger R, Minjas JN, Wilson ML, Shao J, Durack DT: Intestinal parasites and HIV infection in Tanzanian children with chronic diarrhoea. AIDS. 1993, 7: 213-221. 10.1097/00002030-199302000-00009.
Vargas M, Gascon J, Casals C, Schellenberg D, Urassa H, Kahigwa E, Ruiz J, Vila J: Etiology of diarrhoea in children less than five years of age in Ifakara, Tanzania. Am J Trop Med Hyg. 2004, 70: 536-539.
WHO: IMCI Integrated Mangagement of Childhood Illness. Model Chapter for Textbooks. Document no WHO/FCH/CAH/00.40. 2001, Geneva: World Health Organization
Waterlow JC, Buzina R, Keller W, Lane TM, Nichman MZ, Taner JM: The presentation and use of height and weight data for comparing nutritional status of groups of children under age of 10 years. Bull Wld Hlth Org. 1977, 55: 489-498.
Baron Murray, Tenover Pfaller: Manual of Clinical Microbiology. 1999, American Society of Microbiology Press, Washington DC, 6:
Moyo SJ, Maselle SY, Matee MI, Langeland N, Mylvaganam H: Identification of diarrhoeagenic Escherichia coli isolated from infants and children in Dar es Salaam, Tanzania. BMC Infectious Diseases. 2007, 7: 92-10.1186/1471-2334-7-92.
Clinical and Laboratory Standards Institute: Ninth edition Document M2-A9. Clinical and Laboratory Standards Institute. 2006, Wayne, PA, Performance standards for antimicrobial disk susceptibility tests. Approved standard
Nimri LF, Elnasser Z, Batchoun R: Polymicrobial infections in children with diarrhoea in a rural area of Jordan. FEMS immunology and medical microbiology. 2004, 42: 255-259. 10.1016/j.femsim.2004.05.014.
Nair GB, Ramamurthy T, Bhattacharya MK, Krishnan T, Ganguly S, Rajendran K, Manna B, Ghosh M, Okamoto K, Takeda Y: Emerging trends in the etiology of enteric pathogens as evidenced from an active surveillance of hospitalized diarrhoeal patients in Kolkata, India. Gut Pathog. 2010, 2: 4-10.1186/1757-4749-2-4.
Presterl E, Zwick RH, Reichmann S, Aichelburg A, Winkler S, Kremsner PG, Graninger W: Frequency and virulence properties of diarrhoeagenic Escherichia coli in children with diarrhoea in Gabon. Am J Trop Med Hyg. 2003, 69: 406-4010.
Navia MM, Capitano L, Ruiz J, Vargas M, Urassa H, Schellemberg D, Gascon J, Vila J: Typing and characterization of mechanisms of resistance of Shigella spp. isolated from feces of children under 5 years of age from Ifakara, Tanzania. J Clin Microbiol. 1999, 37: 3113-3117.
Urassa WK, Mhando YB, Mhalu FS, Mjonga SJ: Antimicrobial susceptibility pattern of Vibrio cholerae O1 strains during two cholera outbreaks in Dar es Salaam, Tanzania. East Afr Med J. 2000, 77: 350-353.
Urio EM, Collison EK, Gashe BA, Sebunya TK, Mpuchane S: Shigella and Salmonella strains isolated from children under 5 years in Gaborone, Botswana, and their antibiotic susceptibility patterns. Trop Med Int Health. 2001, 6: 55-59. 10.1046/j.1365-3156.2001.00668.x.
Shapiro RL, Kumar L, Phillips-Howard P, Wells JG, Adcock P, Brooks J, Ackers ML, Ochieng JB, Mintz E, Wahlquist S, Waiyaki P, Slutsker L: Antimicrobial-resistant bacterial diarrhoea in rural western Kenya. J Infect Dis. 2001, 183: 1701-1704. 10.1086/320710.
Ndugulile F, Jureen R, Harthug S, Urassa W, Langeland N: Extended Spectrum β-Lactamases among Gram-negative bacteria of nosocomial origin from an Intensive Care Unit of a tertiary health facility in Tanzania. BMC Infect Dis. 2005, 5: 86-10.1186/1471-2334-5-86.
Blomberg B, Jureen R, Manji KP, Tamim BS, Mwakagile DS, Urassa WK, Fataki M, Msangi V, Tellevik MG, Maselle SY, Langeland N: High rate of fatal cases of pediatric caused by gram-negative bacteria with extended-spectrum beta lactamases in Dar es Salaam, Tanzania. J Clin Microbiol. 2005, 43: 745-749. 10.1128/JCM.43.2.745-749.2005.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2431/11/19/prepub
Acknowledgements
We would like to thank the administration of the Muhimbili National Hospital, Ilala, Mwananyamala and Temeke Municipal Hospitals for giving necessary administrative support. We would also like to thank the parents/guardians of the children who participated in this study without whom this study would have not been possible. We acknowledge the technical support accorded to this study by members of the Departments of Microbiology and Immunology of the Muhimbili University of Health and Allied Sciences (MUHAS) in Dares Salaam, Tanzania and Haukeland University Hospital in Bergen, Norway. We are grateful to the Haukeland University Hospital, Norwegian Public Health Institute in Oslo, Norway and Statens Serum Institute, Denmark, for providing the positive controls strains.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
SJM was the principal investigator, who conceived and designed study and was responsible for collection of specimens and clinical information as well as data analysis. Laboratory investigations were performed by SJM under the guidance of NG and HM. MIM, JK, HM, HM SYM and NL assisted in the development of the research proposal, data analysis and preparation of the manuscript. All authors have read and approved the final manuscript.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Moyo, S.J., Gro, N., Matee, M.I. et al. Age specific aetiological agents of diarrhoea in hospitalized children aged less than five years in Dar es Salaam, Tanzania. BMC Pediatr 11, 19 (2011). https://doi.org/10.1186/1471-2431-11-19
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2431-11-19