Abstract
Background
Biosurfactants (BS) are amphiphilic compounds produced by microbes, either on the cell surface or secreted extracellularly. BS exhibit strong antimicrobial and anti-adhesive properties, making them good candidates for applications used to combat infections. In this study, our goal was to assess the in vitro antimicrobial, anti-adhesive and anti-biofilm abilities of BS produced by Lactobacillus jensenii and Lactobacillus rhamnosus against clinical Multidrug Resistant (MDR) strains of Acinetobacter baumannii, Escherichia coli, and Staphylococcus aureus (MRSA). Cell-bound BS from both L. jensenii and L. rhamnosus were extracted and isolated. The surface activities of crude BS samples were evaluated using an oil spreading assay. The antimicrobial, anti-adhesive and anti-biofilm activities of both BS against the above mentioned MDR pathogens were determined.
Results
Surface activities for both BS ranged from 6.25 to 25 mg/ml with clear zones observed between 7 and 11 cm. BS of both L. jensenii and L. rhamnosus showed antimicrobial activities against A. baumannii, E. coli and S. aureus at 25-50 mg/ml. Anti-adhesive and anti-biofilm activities were also observed for the aforementioned pathogens between 25 and 50 mg/ml. Finally, analysis by electron microscope indicated that the BS caused membrane damage for A. baumannii and pronounced cell wall damage in S. aureus.
Conclusion
Our results indicate that BS isolated from two Lactobacilli strains has antibacterial properties against MDR strains of A. baumannii, E. coli and MRSA. Both BS also displayed anti-adhesive and anti-biofilm abilities against A. baumannii, E. coli and S. aureus. Together, these capabilities may open up possibilities for BS as an alternative therapeutic approach for the prevention and/or treatment of hospital-acquired infections.
Similar content being viewed by others
Background
Biosurfactants (BS) are amphiphilic compounds produced mostly by microbes on their cell surface, or secreted extracellularly and exhibit strong surface and emulsifying activities. They contain both hydrophobic and hydrophilic moieties that can reduce the surface or interfacial tension in liquids [1]. BS are complex molecules that include glycolipids, rhamnolipids, lipopeptides, polysaccharide-protein complexes, phospholipids, fatty acids and neutral lipids [2]. Unlike synthetic surfactants, BS are diverse and biodegradable, and have the potential for highly selective, specialized functions. Several BS exhibit anti-bacterial, anti-fungal and anti-viral activities, making them appropriate candidates to combat infections [3].
The list of known BS includes surfactin, the most powerful BS known, which is produced by Bacillus subtilis[4]. Other BS with antimicrobial activity include iturin, also produced by B. subtilis[4], mannosylerythritol lipids from Candida antarctica[5], rhamnolipids from Pseudomonas aeruginosa[6] and those isolated from probiotic bacteria Streptococcus thermophilus A and Lactococcus lactis[7–9]. Probiotic lactobacilli, which constitute an important part of natural microbiota, are recognized as potent interfering bacteria due to the production of various antimicrobial agents including BS [10]. In one study, 15 Lactobacillus strains were tested in vitro for BS production. It was found that all released surface active components during their mid-exponential and stationary growth phases [6].
Another valuable attribute of BS is their use as anti-adhesive/anti-biofilm agents [3, 11] as shown previously in the lack of adhesion of Enterococcus faecalis to glass with an adsorbed BS layer from Lactobacillus acidophilus RC14 or Lactobacillus fermentum B54 [12].
Biofilms are conglomerations of bacterial cells protected by self-synthesized extracellular polysaccharide matrices (EPS). Biofilm infections are extremely challenging to treat because antimicrobials are less effective than planktonic cells [13, 14], thus making clearance more challenging. The presence of biofilms causes numerous problems in the field of medicine, interfering with clinical therapy of chronic and wound-related infections as well as persistent infections of various indwelling medical devices [15]. Although numerous strategies have been established and are currently in use to control biofilms, the pursuit for novel, natural, and effective anti-biofilm agents still continues [16–18].
In recent years, the use of BS as alternatives to control biofilms has been explored extensively [19–21]. BS have been shown to modify the surface properties of bacterial cells and reduce their adhesive properties [4]. In addition, BS produced by bacteria have been shown to interfere with biofilm development and cell to cell communication [22–24].
Studies in the past have demonstrated the ability of probiotic bacteria L. acidophilus-derived BS to inhibit staphylococcal biofilm development and also induce its dispersion [25]. BS produced by probiotic lactobacilli have been shown to reduce adhesion of pathogenic bacteria to glass, silicone rubber, surgical implants, and voice prostheses [8, 12, 26, 27]. It is believed that when BS is applied to a substratum surface, it modifies its hydrophobicity, interfering in the microbial adhesion and desorption processes [28, 29]. Consequently, prior application of BS on catheters and other medical insertion materials may be used as a preventive strategy to delay the onset of pathogenic biofilm growth of MDR bacteria on wounds, medical insertion materials and inert surfaces in the hospital environment [8, 12, 25–27, 30]. Thus, the prevention of biofilm formation or disruption by natural lactobacilli-derived agents was tested in these in vitro studies as a possible approach leading to novel antimicrobials.
The aims of this study were to determine the antimicrobial, anti-adhesive, and anti-biofilm activities of cell-bound BS isolated from L. jensenii and L. rhamnosus against several clinical isolates of multidrug-resistant pathogens.
Results
Oil spreading assay
The oil spreading assay was utilized to study the surface activities of crude BS. This assay is rapid, and is highly sensitive to surface active compounds [31, 32]. Both L. jensenii and L. rhamnosus strains demonstrated oil displacement activity in motor oil. The oil displacement activity, as measured by the area of the clear zone on the oil-water surface, increased with an increase in the concentration of BS (Table 1).
Antimicrobial assay with BS
The crude BS of both L. jensenii and L. rhamnosus were tested against two clinical isolates of MDR A. baumannii, E. coli and S. aureus. We found both BS to be effective in killing all three MDR pathogens at 50 mg/ml (Table 2). L. jensenii BS exhibited almost 100% activity against all the strains tested (Table 2). The activity of L. rhamnosus ranged from 96-97% against A. baumannii and 72-85% against E. coli. For S. aureus strains UAMS-1 and MRSA respectively, activity was between 80 and 93% respectively (Table 2).
Impact of BS on bacterial attachment to abiotic surface
Biofilm formation is a complex process that generally involves three stages: (1) primary adhesion to surfaces, (2) accumulation of multilayered clusters of cells, and (3) detachment. Because binding of host proteins is a major contributor to primary adhesion, it was important to test initial adherence to surfaces that were coated with plasma. Experiments were performed to determine the stage at which BS disrupts biofilm formation. Using an adherence assay, the ability of two BS to inhibit the cell attachment in the presence of host proteins was measured by coating the plates with human plasma. After various concentrations of BS ranging from 25-50 mg/ml were tested, it was found that the two BS significantly impaired the attachment of A. baumannii and E. coli at 50 mg/ml (Figure 1). S. aureus adherence to abiotic surfaces was disrupted at concentrations between 25 and 50 mg/ml (Figure 1).
The ability of biosurfactant from L. jensenii (BSLJ) and L. rhamnosus (BSLR) to reduce initial adherence of A. baumannii, E. coli and S. aureus is indicated. BS was used at 50 mg/ml for A. baumannii, E. coli and at 25 mg/ml for S. aureus. Treated cells were statistically different from controls. The results represent the means plus SEM. Student’s paired t test was used to determine the statistical significance of the treated versus untreated conditions (*, P < 0.05).
Impact of BS on biofilm development
Next, it was determined if the static biofilm assay could show whether both BS possessed anti-biofilm activity against A. baumannii, E. coli and S. aureus. The BS produced by both L. jensenii and L. rhamnosus significantly reduced biofilm development by A. baumannii and E. coli at 50 mg/ml (Figure 2). Furthermore, the two BS significantly inhibited S. aureus biofilms at both concentrations of 25 mg/ml respectively (Figure 2).
The ability of biosurfactants from L. jensenii (BSLJ) and L. rhamnosus (BSLR) in reducing biofilm formation in A. baumannii, E. coli and S. aureus is indicated. BS was used at 50 mg/ml for A. baumannii, E. coli and at 25 mg/ml for S. aureus. Treated cells were statistically different from controls. The results represent the means plus SEM. Student’s paired t test was used to determine the statistical significance of the treated versus untreated conditions (*, P < 0.05).
Dispersion of preformed biofilms by BS
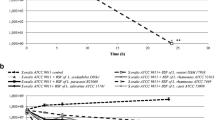
In the experiments thus far, the BS were added concurrently with inoculation of bacteria. To determine if these compounds dispersed preformed biofilms, A. baumannii and E. coli biofilms were developed on MBEC pegs, and then exposed to varying concentrations of BS in fresh media for varying time intervals. After removal of the pegs, the amounts of bacteria that remained on the pegs were quantified by crystal violet staining. Compared to the controls, preformed A. baumannii and E. coli biofilms treated with BS at 100 mg/ml for 1 hr did not produce any dispersion effect. However, when biofilms were exposed for longer durations (~18 hrs), an increased biofilm dispersion was observed (Figure 3). Furthermore, an increase in dispersion was also observed for S. aureus biofilms when exposed to the BS at concentrations of 50 mg/ml for 18 hrs respectively (Figure 3).
The ability of biosurfactants from L. jensenii (BSLJ) and L. rhamnosus (BSLR) in dispersing biofilm formation in A. baumannii, E. coli and S. aureus is indicated. BS was used at 100 mg/ml for A. baumannii, E. coli and at 50 mg/ml for S. aureus. Treated cells were statistically different from controls. The results represent the means plus SEM. Student’s paired t test was used to determine the statistical significance of the treated versus untreated conditions (*, P < 0.05).
Cytotoxicity assays for BS in eukaryotic cells
Results from the cell-mediated cytotoxicity assay are presented in Figure 4. Human A549 lung epithelial cells were treated with BS from both Lactobacilli strains at various concentrations (25, 50, 100 and 200 mg/ml) for 24 h. Cytotoxicity was determined by LDH release according to the manufacturer’s instructions and the total cell number assay (Figure 4). Concentrations of 25-100 mg/ml showed no toxicity. Both BS showed very low toxicity levels at 200 mg/ml (Figure 4).
Transmission electron microscopy
TEM was used to evaluate the ultra-structural morphological alterations exerted to A. baumannii and S. aureus in the presence of BSLR. We chose A. baumannii 5075 and S. aureus UAMS-1 strains to represent a Gram negative and Gram positive pathogen for analysis. Untreated cells of the both A. baumannii and S. aureus showed a normal cell shape with an intact structure of the cell wall, inner membrane and outer membrane. The images of the A. baumannii samples treated with L. rhamnosus BS were markedly different to those of the untreated cells. Several BSLR treated A. baumannii cells had their membranes damaged at certain areas of the bacterial cell with accumulation of dense substance (Figure 5). Surprisingly we also found that L. rhamnosus BS seems to cause more damage specifically to the ends of the bacterial cell (Figure 5). S. aureus cells treated with L. rhamnosus BS exhibited profound structural differences when compared to untreated cells. Several cells were observed devoid of cell walls, a phenomenon called as “ghost” cells. The dark and light areas observed in the cells were indicative of high and low electron densities respectively. Several cells were found to contain septa when compared with the control samples (Figure 5). This may be due to BS interfering with the cell division process and this is probably indicative of one of the mechanisms of action of BSLR by inhibiting the cell division.
Transmission electron microscope details on A. baumanni and S. aureus treated with BSLR. A. baumannii and S. aureus grown in the presence and absence of BSLR (4X MIC) were imaged at 3 h post incubation. Photographs were taken at a magnification of × 15000. The thick arrow indicates septum formation and the thin arrow indicates the ghost cells appearance respectively. For S. aureus, images were also acquired at lower magnification of ×8000, where a visible difference was seen between treated and untreated samples. BSLR treated S. aureus showed many more ghost cells (thin arrows) and cells without visible intracellular organelles compared to untreated cells (thick double arrows).
Discussion
Here, we describe two cell-associated biosurfactants derived from probiotic lactobacilli bacteria that possess both antibacterial activities and inhibit biofilm formation by several important drug-resistant pathogens. Although some strains of lactobacilli are known to produce surfactants, to the best of our knowledge there are no reports on the abilities of L. jensenii and L. rhamnosus BS as anti-biofilm agents. The crude BS derived from aforementioned bacteria showed significant antimicrobial activities against A. baumannii, E. coli, MRSA and S. aureus at MIC concentrations ranging between 25 and 50 mg/ml. L. jensenii BS showed antimicrobial activity at 25 mg/ml against all three pathogens with killing that varied from 75-99.9%, and at 12.5 mg/ml, it showed 90-100% killing against MRSA. In addition, we observed similar antimicrobial activities from both BS with similar MIC concentrations against MDR Klebsiella pneumoniae (Table 2). In this study, we clearly showed the effect of BS on the bacterial cells by transmission electron microscopy (Figure 5). The bacterial cell membrane appears to be the target of BS activity and subsequent microbicidal activity of BS may be due to the leakage of cellular contents. BS that exhibit antimicrobial activity has been previously described [33–35], but to date there have been very few studies on the activity of BS isolated from lactobacilli [8, 9, 28, 29, 33]. The antimicrobial results generated from our studies were similar to the results from crude BS studies on L. paracasei ssp. paracasei A20 and L. lactis, which completely inhibited the growth of several micro-organisms at concentrations ranging between 25 and 100 mg/ml [8, 9, 33]. In addition, BS exhibited excellent anti-adhesive properties against S. aureus, A. baumannii and E. coli, as evidenced in our adhesion based assays.
Next, the biofilm inhibition and dispersal capability of BS against the above mentioned three pathogens was evaluated. The crude BS isolated in this study exhibited very good anti-biofilm activities against select microorganisms. In the past, several studies have documented the anti-biofilm activity of BS isolated from different bacteria [19–21]. Preformed biofilms of all the three bacteria tested in microtiter plate wells were effectively disrupted by the BS. The BS dispersed all three bacteria when exposed for longer durations. The inhibition of biofilms using surfactants has been reported previously [12]. In addition, BS have been shown to disperse biofilms of Bordetella bronchiseptica and B. pumilus[19, 22]. The increased anti-biofilm and dispersal ability of the BS currently being investigated may be due to the two important properties that it displays, namely, antimicrobial and surfactant activity. Previous studies with a BS isolated from Lactobacillus spp. have only demonstrated its antimicrobial and anti-adhesive properties [33]. Here we report for the first time BS isolated from lactobacillus also displaying anti-biofilm properties. Both L. jensenii and L. rhamnosus BS were able to significantly reduce biofilm development by A. baumannii, E. coli and S. aureus.
The use and applications of BS in the medical field has increased considerably in the last years. The impact of BS in bacterial adhesion and desorption has been widely discussed, and subsequent adsorption of these BS to solid abiotic surfaces could prove an effective strategy to reduce bacterial adhesion, thereby combating microbial colonization in both medicine and industry [7, 30, 36, 37]. The anti-biofilm and anti-adhesive activities of the BS observed against several pathogens in our studies opens up the possibility of using them to coat a variety of medical surfaces to drastically reduce microbial colonization.
In conclusion, in this work we have demonstrated the antimicrobial, anti-biofilm, and anti-adhesive properties of the crude BS isolated from L. jensenii against several pathogenic MDR bacteria. We also observed that addition of both BS at effective concentrations to eukaryotic cells resulted in low cytotoxicity (Figure 4), suggesting the safety of these compounds for topical delivery. Biofilm encroachment on biomaterial is an extremely important concern post-surgery. Hence, our results open the possibility of using BS-modified materials for the construction of biofilm-resistant medical implantable devices, given its broad-spectrum activity against both Gram-positive and Gram-negative bacterial strains. BS exhibits potential as a new therapeutic strategy to inhibit biofilm formation. Because the increased prevalence of antibiotic-resistant bacteria generates a need for alternate and novel strategies to combat biofilms, we believe that co-administering antibiotics with anti-biofilm agents that possess surface activities such as BS may form the basis of future clinical protocols against biofilm-based infections.
Currently, experiments are underway to characterize the crude fractions of the surfactants by high performance liquid chromatography. We have identified certain fractions that exhibit excellent antimicrobial activities against A. baumanni, S. aureus, K. pneumoniae and E. coli. These fractions are being further analyzed by mass spectrometry and Matrix assisted laser desorption/ionization- time of flight (MALDI-TOF) to identify the active component/s.
Conclusion
The BS produced by L. jensenii and L. rhamnosus showed antiadhesive, antimicrobial and antibiofilm activities against several MDR bacteria, such as E. coli, A. baumannii and S. aureus, which are prominent biofilm formers on wounds, medical implants and industrial surfaces. Antiadhesive and antimicrobial activities were seen between 25-100 mg/ml. MBEC based biofilm assays confirmed the inhibitory action of BS on biofilm development at concentrations ranging 25-50 mg/ml. In addition, BS dispersed preformed biofilms of A. baumannii and S. aureus at concentrations ranging 50-100 mg/ml. Due to its surface tension reduction properties, BS can be used to coat medical surfaces to prevent microbial colonization by variety of bacteria causing indwelling device associated infections.
Methods
Strains and growth conditions
L. jensenii 25258 and L. rhamnosus 7469 were purchased from ATCC (ATCC, Manassas, VA, USA). The strains were stored at -80°C in MRS broth (Difco, Sparks, MD, USA) containing 20% (v/v) glycerol. Multi-drug-resistant test strains were stored at −80°C in the appropriate media with 15% (v/v) glycerol until use. E. coli strains EC433, EC438, A. baumannii strains AB5075, AB5711 were cultured in LB broth and S. aureus clinical isolate 243 (MRSA) and UAMS-1 in trypticase soy broth. All the strains were grown at 37°C for 4 h in the appropriate media, and were washed in PBS 2X and resuspended in PBS to the appropriate OD at 600 nm for testing.
BS production and isolation
To isolate cell-associated BS, the following protocol was pursued according to previously published methods used by several other investigators for lactobacilli BS [8, 10, 33]. For crude BS production by L. jensenii 25258, 1200 ml of MRS culture broth was inoculated with 10 ml of an overnight culture of L. jensenii and incubated for 48 h at 37°C at 120 RPM on a shaker. For L. rhamnosus, 1200 ml culture of MRS broth was inoculated with 10 ml of an overnight culture and incubated for 48 h at 33°C without shaking. After 48 hours, cell pellets were collected by centrifugation (10000 × g, 10 min, 10°C), washed twice in demineralized water, and re-suspended in 100 ml of PBS. This solution was gently stirred at room temperature for 2 h to release the cell-bound BS. After 2 hours, bacteria were removed by centrifugation and the supernatant liquid was collected by filtering through a 0.22 um filter. The filtered sterile supernatant was lyophilized. The freeze-dried BS was stored at -20°C, and resuspended in deionized water at 100 mg/ml (w/vol).
Antimicrobial assay with BS
The antimicrobial activities of L. jensenii and L. rhamnosus crude BS against several pathogens were determined in 96-well tissue culture plates by a modified microdilution method [33]. Briefly, 100 μl of sterile, double-strength MHB broth was placed into the first column of the 96-well microplate and 100 μl of sterile, single-strength MHB broth in the remaining wells. Subsequently, 100 μl of BS solution in PBS (100 mg/ml) was added to the first column of the microplate and mixed with the medium; this resulted in a BS concentration of 50 mg/ml, and 100 μl was transferred serially to the subsequent wells, resulting in two-fold dilutions. Columns without BS served as positive growth controls. All the wells were inoculated with 100 μl of 108 CFU from each of the test strains from a log phase culture. Microtiter plates were covered and incubated for 24 h under the appropriate growth conditions for each microorganism. Three independent preparations of crude BS were tested in duplicate. The contents of each well were plated onto LB agar plates with appropriate dilutions, and CFU were enumerated the next day. Percent killing was calculated as 1- (treated/control × 100).
Oil spreading assay to determine surfactant activity
For the oil spreading assay, 50 ml of demineralized water was added to a 150 mm diameter Petri dish and 20 μl of motor oil was added to the surface of the water. Ten microliters of crude BS from either L. jensenii or L. rhamnosus, dissolved in deionized water was then added to the surface of the oil at concentrations ranging from 6.25 to 50 mg/ml. Surfactin was used as a positive control at the same concentrations, and a negative control was included with PBS. The diameters of clear zones of triplicate assays from the same sample were determined.
Cytotoxicity assay
The human lung epithelial cell line (A549) was used in this study. The cytotoxicity of the crude BS from both Lactobacilli was evaluated on eukaryotic cells by the release of lactate dehydrogenase (LDH) and total cell number assay. The LDH cytotoxicity assay was performed according to the manufacturer’s guidelines (CytoTox 96 Non-Radioactive Cytotoxicity Assay, Promega, Madison, WI, USA). After the addition of the crude BS at different concentrations for 24 h, the cell culture medium was collected for LDH measurement after lysis of cells. An aliquot of 50 μl cell medium was used for LDH activity analysis and the absorption was measured using a UV–visible spectrophotometer. Percentage cytotoxicity was calculated as the percentage of LDH released compared to untreated cells. All experiments were repeated three times, each in triplicate.
Assessment of biofilm formation
Biofilm formation was measured under two static conditions using a quantitative crystal violet assay. BS was added to the wells that contained the media and bacterial cells. BS were used at 25-50 mg/ml concentrations in final total volume not exceeding 165 μl, the volume at which the biofilms develop well in the MBEC biofilm assay. Biofilms of A. baumannii were developed on polystyrene 96-well and MBEC (Biosurface Technologies, Bozeman, MT, USA) as described previously by Sambanthamoorthy, 2012 [38]. Briefly, cultures grown overnight were standardized to an OD595 of 0.05 and 165 μl was transferred to the wells of a 96-well polystyrene microtiter plate, and the MBEC lid was placed on top of the wells. BS were added concurrently to the wells and biofilms were grown on the pegs under shaking conditions for 24 h. The lid was removed and the pegs were gently washed twice with 200 μl of PBS to remove non-adherent cells. Adherent biofilms on the pegs were fixed with 200 μl of 100% ethanol prior to staining for 2 min with 200 μl of 0.41% (wt/vol) crystal violet in 12% ethanol (Biochemical Sciences, Swedesboro, NJ, USA). The pegs were washed several times with PBS to remove excess stain. Quantitative assessment of biofilm formation was obtained by the immersion of pegs in a sterile polystyrene microtiter plate which contained 200 μl of 100% ethanol and incubation at room temperature for 10 min before the absorbance at 595 nm was determined. Three independent experiments were performed for each of these assays. Biofilms of S. aureus were developed on polystyrene 96-well plates and evaluated against the BS as previously described [39].
Biofilm dispersal
To determine if the BS could disperse preformed biofilms, bacterial biofilms were established as previously described [38, 40]. Briefly, established biofilms were exposed to varying concentrations of the BS in fresh media for short time intervals. Adherent biofilms on the pegs were fixed with 200 μl of 100% ethanol prior to staining for 2 min with 200 μl of 0.41% (wt/vol) crystal violet in 12% ethanol (Biochemical Sciences, Swedesboro, NJ, USA). Quantitative assessment of biofilm formation was obtained by the immersion of pegs in a sterile polystyrene microtiter plate which contained 200 μl of 100% ethanol; the absorbance at 595 nm was determined using a SpectraMax M5 microplate spectrophotometer system. Results were interpreted by the comparison of BS on treated biofilms to untreated biofilms. Experiments were performed in triplicate and three independent experiments were performed for each of these assays.
Adherence of A. baumannii, E. coli and S. aureus to abiotic surfaces
An initial adherence assay was used to measure the impact of BS on the surface binding capacity of A. baumannii, E. coli and S. aureus. The assay was performed by modifying a microtiter biofilm assay as described previously [39]. Briefly, overnight cultures of A. baumannii and S. aureus test strains were diluted to an absorbance value of 0.05 at 595 nm in fresh medium, and 200 μl was added to each well (polystyrene pre-coated with human plasma) in triplicate. This was followed by adding BS at relevant concentration to be tested into the wells. Following 1 h incubation at 37°C, the microtiter wells were washed three times with PBS. Adherent cells were then fixed with 200 μl of 100% ethanol for 10 min. The ethanol was removed and the wells were air dried for 2 min. Adherent cells were stained for 2 min with 200 μl of 0.41% crystal violet (w/v in 12% ethanol), then washed three times with PBS. The wells were allowed to dry and then eluted with ethanol. Absorbance readings were made at 595 nm using a SpectraMax M5 microplate spectrophotometer system (Molecular Devices, Sunnyvale, CA, USA). Experiments were performed in triplicate and three independent experiments were performed for each of these assays.
Transmission electron microscopy
A log phase culture of A. baumannii and S. aureus in separate tubes containing LB broth was split into 1.5 ml aliquots. The cells were collected by centrifugation (10000 × g, 5 min) and resuspended in PBS (Sigma-Aldrich, St. Louis, MO, USA). Four samples were prepared; two untreated, two treated with BSLR (4X MIC). The samples were incubated at 37°C for 3 h. The cells were collected by centrifugation (10000 × g, 5 min) to aspirate the supernates. To fix the cells, 4% glutaraldehyde was added to the pellet and the samples were incubated at 4°C for 1 h. The cells were collected by centrifugation (10000 rpm, 5 min) and washed twice with 0.1 M phosphate buffer. To postfix the cells, 1% osmium tetraoxide was added and the samples were left at room temperature for 1 h. The samples were dehydrated with graded ethanol solutions (50% ethanol for 15 min, 70% ethanol for 15 min, 95% ethanol for 15 min, and 100% ethanol for 30 min), embedded in epon and left to polymerize for 24 hrs. From each sample 10 thin slices (approximately 100 nm) were cut with Leica ultra cut UCT (Leica, Buffalo grove, IL, USA). Each of these sections was examined with a JEOL 1400 transmission electron microscope (JEOL, Peabody, MA, USA).
Abbreviations
- BS:
-
Biosurfactants
- MDR:
-
Multidrug-resistant
- MRSA:
-
Methicillin resistant Staphylococcus aureus
- EPS:
-
Extracellular polysaccharide
- MBEC:
-
Minimum biofilm eradication concentration.
References
Van Hamme JD, Singh A, Ward OP: Physiological aspects. Part 1 in a series of papers devoted to surfactants in microbiology and biotechnology. Biotechnol Adv. 2006, 24 (6): 604-620.
Cameotra SS, Makkar RS, Kaur J, Mehta S: Synthesis of biosurfactants and their advantages to microorganisms and mankind. Biosurfaces. 2010, 672: 261-280.
Singh P, Cameotra SS: Potential applications of microbial surfactants in biomedical sciences. Trends Biotechnol. 2004, 22 (3): 142-146.
Ahimou F, Jacques P, Deleu M: Surfactin and iturin A effects on bacillus subtilis surface hydrophobicity. Enzyme Microb Technol. 2000, 27 (10): 749-754.
Arutchelvi JI, Bhaduri S, Uppara PV, Doble M: Mannosylerythritol lipids: a review. J Ind Microbiol Biotechnol. 2008, 35 (12): 1559-1570.
Benincasa M, Abalos A, Oliveira I, Manresa A: Chemical structure, surface properties and biological activities of the biosurfactant produced by Pseudomonas aeruginosa LBI from soapstock. Antonie Van Leeuwenhoek. 2004, 85 (1): 1-8.
Rodrigues L, van der Mei H, Banat IM, Teixeira J, Oliveira R: Inhibition of microbial adhesion to silicone rubber treated with biosurfactant from Streptococcus thermophilus A. FEMS Immunol Med Microbiol. 2006, 46 (1): 107-112.
Rodrigues L, van der Mei H, Teixeira JA, Oliveira R: Biosurfactant from Lactococcus lactis 53 inhibits microbial adhesion on silicone rubber. Appl Microbiol Biotechnol. 2004, 66 (3): 306-311.
Rodrigues L, van der Mei HC, Teixeira J, Oliveira R: Influence of biosurfactants from probiotic bacteria on formation of biofilms on voice prostheses. Appl Environ Microbiol. 2004, 70 (7): 4408-4410.
Velraeds MMC, van der Mei HC, Reid G, Busscher HJ: Physicochemical and biochemical characterization of biosurfactants released by Lactobacillus strains. Colloids Surf B Biointerfaces. 1996, 8 (1–2): 51-61.
Rodrigues L, Banat IM, Teixeira J, Oliveira R: Biosurfactants: potential applications in medicine. J Antimicrob Chemother. 2006, 57 (4): 609-618.
Velraeds MM, van der Mei HC, Reid G, Busscher HJ: Inhibition of initial adhesion of uropathogenic Enterococcus faecalis by biosurfactants from Lactobacillus isolates. Appl Environ Microbiol. 1996, 62 (6): 1958-1963.
Costerton JW, Lewandowski Z, Caldwell DE, Korber DR, Lappin-Scott HM: Microbial biofilms. Annu Rev Microbiol. 1995, 49: 711-745.
Anderl JN, Franklin MJ, Stewart PS: Role of antibiotic penetration limitation in Klebsiella pneumoniae biofilm resistance to ampicillin and ciprofloxacin. Antimicrob Agents Chemother. 2000, 44 (7): 1818-1824.
Fux CA, Costerton JW, Stewart PS, Stoodley P: Survival strategies of infectious biofilms. Trends Microbiol. 2005, 13 (1): 34-40.
Fusetani N: Biofouling and antifouling. Nat Prod Rep. 2004, 21 (1): 94-104.
Qian PY, Xu Y, Fusetani N: Natural products as antifouling compounds: recent progress and future perspectives. Biofouling. 2010, 26 (2): 223-234.
Tahmourespour A, Salehi R, Kermanshahi RK, Eslami G: The anti-biofouling effect of Lactobacillus fermentum-derived biosurfactant against Streptococcus mutans. Biofouling. 2011, 27 (4): 385-392.
Dusane DH, Nancharaiah YV, Zinjarde SS, Venugopalan VP: Rhamnolipid mediated disruption of marine Bacillus pumilus biofilms. Colloids Surf B Biointerfaces. 2010, 81 (1): 242-248.
Dusane DH, Rajput JK, Kumar AR, Nancharaiah YV, Venugopalan VP, Zinjarde SS: Disruption of fungal and bacterial biofilms by lauroyl glucose. Lett Appl Microbiol. 2008, 47 (5): 374-379.
Rivardo F, Turner RJ, Allegrone G, Ceri H, Martinotti MG: Anti-adhesion activity of two biosurfactants produced by Bacillus spp. prevents biofilm formation of human bacterial pathogens. Appl Microbiol Biotechnol. 2009, 83 (3): 541-553.
Irie Y, O’Toole GA, Yuk MH: Pseudomonas aeruginosa rhamnolipids disperse Bordetella bronchiseptica biofilms. FEMS Microbiol Lett. 2005, 250 (2): 237-243.
Rasmussen TB, Givskov M: Quorum-sensing inhibitors as anti-pathogenic drugs. Int J Med Microbiol. 2006, 296 (2–3): 149-161.
Valle J, Da Re S, Henry N, Fontaine T, Balestrino D, Latour-Lambert P, Ghigo JM: Broad-spectrum biofilm inhibition by a secreted bacterial polysaccharide. Proc Natl Acad Sci U S A. 2006, 103 (33): 12558-12563.
Walencka E, Rozalska S, Sadowska B, Rozalska B: The influence of Lactobacillus acidophilus-derived surfactants on staphylococcal adhesion and biofilm formation. Folia Microbiol. 2008, 53 (1): 61-66.
Busscher HJ, van Hoogmoed CG, Geertsema-Doornbusch GI, van der Kuijl-Booij M, van der Mei HC: Streptococcus thermophilus and its biosurfactants inhibit adhesion by Candida spp. on silicone rubber. Appl Environ Microbiol. 1997, 63 (10): 3810-3817.
Gan BS, Kim J, Reid G, Cadieux P, Howard JC: Lactobacillus fermentum RC-14 inhibits Staphylococcus aureus infection of surgical implants in rats. J Infect Dis. 2002, 185 (9): 1369-1372.
Rodrigues LR, Teixeira JA, van der Mei HC, Oliveira R: Isolation and partial characterization of a biosurfactant produced by Streptococcus thermophilus A. Colloids Surf B Biointerfaces. 2006, 53 (1): 105-112.
Rodrigues LR, Teixeira JA, van der Mei HC, Oliveira R: Physicochemical and functional characterization of a biosurfactant produced by Lactococcus lactis 53. Colloids Surf B Biointerfaces. 2006, 49 (1): 79-86.
Singh A, Van Hamme JD, Ward OP: Surfactants in microbiology and biotechnology: Part 2. Application aspects. Biotechnol Adv. 2007, 25 (1): 99-121.
Satpute S, Bhawsar BD, Dhakephalkar PK, Chopade BA: Assessment of different screening methods for selecting biosurfactant producing marine bacteria. IJMS. 2008, 37 (3): 243-250.
Walter V, Syldatk C, Hausmann R: Screening concepts for the isolation of biosurfactant producing microorganisms. Adv Exp Med Biol. 2010, 672: 1-13.
Gudina EJ, Rocha V, Teixeira JA, Rodrigues LR: Antimicrobial and antiadhesive properties of a biosurfactant isolated from Lactobacillus paracasei ssp. paracasei A20. Lett Appl Microbiol. 2010, 50 (4): 419-424.
Sriram MI, Kalishwaralal K, Deepak V, Gracerosepat R, Srisakthi K, Gurunathan S: Biofilm inhibition and antimicrobial action of lipopeptide biosurfactant produced by heavy metal tolerant strain Bacillus cereus NK1. Colloids Surf B Biointerfaces. 2011, 85 (2): 174-181.
Mukherjee S, Das P, Sivapathasekaran C, Sen R: Antimicrobial biosurfactants from marine Bacillus circulans: extracellular synthesis and purification. Lett Appl Microbiol. 2009, 48 (3): 281-288.
Nitschke M, Costa SGVAO: Biosurfactants in food industry. Trends Food Sci Technol. 2007, 18 (5): 252-259.
Falagas ME, Makris GC: Probiotic bacteria and biosurfactants for nosocomial infection control: a hypothesis. J Hosp Infect. 2009, 71 (4): 301-306.
Sambanthamoorthy K, Sloup RE, Parashar V, Smith JM, Kim EE, Semmelhack MF, Neiditch MB, Waters CM: Identification of small molecules that antagonize diguanylate cyclase enzymes to inhibit biofilm formation. Antimicrob Agents Chemother. 2012, 56 (10): 5202-5211.
Sambanthamoorthy K, Schwartz A, Nagarajan V, Elasri MO: The role of msa in staphylococcus aureus biofilm formation. BMC Microbiol. 2008, 8: 221-
Feng X, Sambanthamoorthy K, Palys T, Paranavitana C: The human antimicrobial peptide LL-37 and its fragments possess both antimicrobial and antibiofilm activities against multidrug-resistant Acinetobacter baumannii. Peptides. 2013, 49: 131-137.
Acknowledgments
The findings and opinions expressed herein belong to the authors and do not necessarily reflect the official views of the WRAIR, the U.S. Army, or the Department of Defense. This work was supported by a Defense Medical Research and Development Program (DMRDP) funding awarded to Dr. Chrysanthi Paranavitana. The authors would like to thank Ms. Amy Michels for editing the manuscript and Mr. Edward A. Asafo-Adjei for helping with electron microscopy experiments.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
KS designed and developed the assays for adhesion, biofilm inhibition and dispersion. KS also drafted the manuscript. XF carried out the antimicrobial and toxicity assays. SP and RP isolated the BS and performed the oil spreading assay. CP conceived of the study, participated in its design and coordination, and also drafted the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Sambanthamoorthy, K., Feng, X., Patel, R. et al. Antimicrobial and antibiofilm potential of biosurfactants isolated from lactobacilli against multi-drug-resistant pathogens. BMC Microbiol 14, 197 (2014). https://doi.org/10.1186/1471-2180-14-197
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2180-14-197