Abstract
Background
Delirium is a serious neurocognitive disorder among surgical patients in the post-anaesthetic care unit (PACU). Despite the development of screening tools to identify delirium, it is not clear which tool is the most accurate and reliable in assessing delirium in the PACU.
Aim
To examine the diagnostic accuracy of delirium screening tools used in the PACU.
Methods
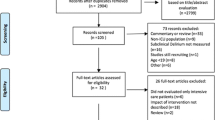
A systematic literature search of CINAHL, MEDLINE, Embase, PsycINFO and Scopus was conducted, using MeSH terms and relevant keywords, from databases establishment to 23 April 2021. Studies were assessed for methodological quality using the Standards for Reporting of Diagnostic Accuracy Studies (STARD) tool.
Results
A total of 1503 studies were screened from the database search, four studies met the inclusion criteria for this review. Six delirium screening tools used in the PACU were identified in the selected studies. Three studies evaluated screening tools in adult surgical patients without cognitive impairment and dementia. Two studies evaluated screening tools among patients who were scheduled for elective surgery. Review results indicated that two tools, the 4A’s test (4AT; sensitivity 96%; specificity 99%) and the 3 min diagnostic interview for the Confusion Assessment Method (3D-CAM; sensitivity 100%; specificity 88%), had greatest validity and reliability as a screening tool for detecting delirium in the PACU.
Conclusion
Results indicate the 4AT and the 3D-CAM are most accurate screening tools to detect delirium in the PACU. Further research is required to validate those tools among a broader surgical population, including patients with cognitive impairment, dementia and those undergoing emergency surgical procedures.



Similar content being viewed by others
References
Inouye SK, Westendorp RGJ, Saczynski JS (2014) Delirium in elderly people. Lancet 9920:911
Aldwikat RK, Manias E, Nicholson P (2020) Incidence and risk factors for acute delirium in older patients with a hip fracture: a retrospective cohort study. Nurs Health Sci. https://doi.org/10.1111/nhs.12753
Lee HB et al (2011) Predisposing factors for postoperative delirium after hip fracture repair in individuals with and without dementia. J Am Geriatr Soc 59:2306–2313
Lee KH et al (2011) Frequency, risk factors, and prognosis of prolonged delirium in elderly patients after hip fracture surgery. Clin Orthop Relat Res 469:2612–2620
Saller T et al (2019) Screening for delirium after surgery: validation of the 4 A’s test (4AT) in the post-anaesthesia care unit. Anaesthesia 74:1260–1266
Neufeld KJ et al (2013) Evaluation of two delirium screening tools for detecting post-operative delirium in the elderly. Br J Anaesth 111:612–618
Veiga D et al (2012) Postoperative delirium in intensive care patients: risk factors and outcome. Braz J Anesthesiol 62:469–483
Marcantonio ER (2020) Still predicting delirium after all these years. Anesth Analg 130:76–78
Aldecoa C et al (2017) European society of anaesthesiology evidence-based and consensus-based guideline on postoperative delirium. Eur J Anaesthesiol 34:192–214
Sendelbach S, Guthrie PF (2009) Acute confusion/delirium: evidence-based practice guideline. University of Iowa Gerontological Nursing Interventions Research Center
National Institute for Health and Care Excellence (2014) Delirium: prevention, diagnosis and management. https://www.nice.org.UK/Guidance/cg103. Accessed 2 Aug 2020
Qian Z et al (2021) Delirium screening tools in the emergency department: a protocol for systematic review and meta-analysis. Medicine 100:1–5
Bond P, Goudie K (2015) Identifying and managing patients with delirium in acute care settings. Nurs Older People 27:28–32
American Psychiatric Association (1980) The diagnostic and statistical manual of mental disorders: DSM-III in 1980, 3rd edn. American Psychiatric Publishing
Saller T et al (2021) Implementation of strategies to prevent and treat postoperative delirium in the post-anesthesia caring unit: a German survey of current practice. J Clin Monit Comput 35:599–605
Grover S, Kate N (2012) Assessment scales for delirium: a review. World J Psychiatry 2:58–70
Olbert M et al (2018) 3D-CAM guideline-conform translation for german-speaking countries. Anasthesiol Intensivmed Notfallmed Schmerzther 53:793–796
Stukenberg S et al (2016) How can postoperative delirium be predicted in advance? A secondary analysis comparing three methods of early assessment in elderly patients. Minerva Anestesiol 82:751–759
McInnes MDF et al (2018) Preferred reporting items for a systematic review and meta-analysis of diagnostic test accuracy studies: the PRISMA-DTA statement. JAMA 319:388–396
Akobeng AK (2007) Understanding diagnostic tests 1: sensitivity, specificity and predictive values. Acta Paediatr 96:338–341
De J, Wand AP (2015) Delirium screening: a systematic review of delirium screening tools in hospitalized patients. Gerontologist 55:1079–1099
Bossuyt PM et al (2003) The STARD statement for reporting studies of diagnostic accuracy: explanation and elaboration. Clin Chem 1:7
Olbert M et al (2019) Validation of 3-minute diagnostic interview for CAM-defined delirium to detect postoperative delirium in the recovery room: a prospective diagnostic study. Eur J Anaesthesiol 36:683–687
Radtke FM et al (2008) Comparison of three scores to screen for delirium in the recovery room. Br J Anaesth 101:338–343
Tim M, Dawid P (2019) An algorithm for the classification of study designs to assess diagnostic, prognostic and predictive test accuracy in systematic reviews. Syst Rev 8:1–8
Kamarudin AN, Cox T, Kolamunnage-Dona R (2017) Time-dependent ROC curve analysis in medical research: current methods and applications. BMC Med Res Methodol 17:53
Abelha FJ et al (2010) Evaluation of delirium in postoperative patients: translation and validation of the intensive care delirium screening checklist in a Portuguese post anesthesia care unit. Arq Med 24:121–128
Hight DF et al (2018) Inattentive delirium vs. Disorganized thinking: a new axis to subcategorize PACU delirium. Front Syst Neurosci. https://doi.org/10.3389/fnsys.2018.00022
Pipanmekaporn T et al (2014) Validity and reliability of the Thai version of the confusion assessment method for the intensive care unit (CAM-ICU). Clin Interv Aging 9:879–885
Conti G et al (2014) Sedation and weaning from mechanical ventilation: time for ‘best practice’ to catch up with new realities? Multidiscip Respir Med 9:45
Moreira FT, Neto AS (2016) Sedation in mechanically ventilated patients—time to stay awake? Ann Transl Med. https://doi.org/10.21037/atm.2016.09.37
Australian College of Peri Anaesthesia Nurses, Statement on Staffing. 2018: ACPAN, Retreived 05 Sep 2020, <https://acpan.edu.au/statements=>
Yates C et al (2009) Screening instruments for delirium in older people with an acute medical illness. Age Ageing 38:235–237
Leung JLM et al (2008) Clinical utility and validation of two instruments (the confusion assessment method algorithm and the Chinese version of nursing delirium screening scale) to detect delirium in geriatric inpatients. Gen Hosp Psychiatry 30:171–176
Bellelli G et al (2014) Validation of the 4AT, a new instrument for rapid delirium screening: a study in 234 hospitalised older people. Age Ageing 43:496–502
Acknowledgements
We would like to thank Lisa Grbin librarian at Deakin University for her assistance with the development of the search strategy and systematic search. We also thank Susan Monaghan at the Royal Melbourne Hospital for her assistance with EndNote referencing system.
Funding
For this study, there is no funding source.
Author information
Authors and Affiliations
Contributions
RA, EM, ET and PN have contributed to the design of the systematic review. RA, MA, ET and PN were responsible for performing data collection. RA, EM, ET and PN have conducted analysis and interpretation of the data. RA was responsible for drafting the first version of the paper. EM, ET and PN critically revised the manuscript. All authors agree to be fully accountable for ensuring the integrity and accuracy of the work and read and approved final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors of this study declare no competing interests.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Statement of human and animal rights
This article does not contain any studies with human participants or animals performed by the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Aldwikat, R.K., Manias, E., Tomlinson, E. et al. Delirium screening tools in the post-anaesthetic care unit: a systematic review and meta-analysis. Aging Clin Exp Res 34, 1225–1235 (2022). https://doi.org/10.1007/s40520-021-02057-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-021-02057-w