Abstract
Introduction
Patient reporting in pharmacovigilance is important and contributes to signal detection. However, descriptions of methodologies for using patient reports in signal detection are scarce, and published experiences of how patient reports are used in pharmacovigilance are limited to a few individual countries.
Objective
Our objective was to explore the contribution of patient reports to global signal detection in VigiBase.
Methods
Data were retrieved from VigiBase in September 2016. Drug–event-combination series were restricted to those with >50% patient reports, defined as reporter type “Consumer/non-health professional” per E2B reporting standard. vigiRank was applied to patient reports to prioritize combinations for assessment. Product information for healthcare professionals (HCPs) as well as patient information leaflets (PILs) were used as reference for information on adverse drug reactions (ADRs). Staff from the Uppsala Monitoring Centre and the Netherlands Pharmacovigilance Centre Lareb categorized the combinations. Potential signals proceeded to a more in-depth clinical review to determine whether the safety concern should be communicated as a “signal.”
Results
Of the 212 combinations assessed, 20 (9%) resulted in eight signals communicated within the World Health Organization (WHO) programme for international drug monitoring. Review of PILs revealed insufficient ADR descriptions for patients and examples of poor consistency with product information for HCPs. Patient narratives provided details regarding the experience and impact of ADRs and evidence that patients make causality and personal risk assessments.
Conclusions
Safety concerns described in patient reports can be identified in a global database including previously unknown ADRs as well as new aspects of known ADRs. Patient reports provide unique information valuable in signal assessment and should be included in signal detection. Novel approaches to highlighting patient reports in statistical signal detection can further improve the contribution of patient reports to pharmacovigilance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
New drug safety concerns described in patient reports can be identified in a global database. |
Case narratives from patient reports provide detailed clinical stories that describe the experiences and the impact of adverse drug reactions on the patient’s quality of life. |
To benefit from the unique information available in patient reports to pharmacovigilance, signal detection practice that focuses on the review of case narratives, such as case-by-case assessments, is preferable. When this is not possible, we recommend considering tailoring statistical signal detection to capture patient concerns. |
1 Introduction
Since their inception, spontaneous reporting systems have primarily relied on healthcare professionals (HCPs) to make clinical judgements about suspected adverse drug reactions (ADRs) and report them to national pharmacovigilance centres, either directly or via drug companies. The USA, Canada, and Australia have accepted reports directly from patients since the 1960s, and legislation passed in 2012 in the EU requires all European countries to incorporate patient reporting in their spontaneous reporting systems [1]; however, some countries have not yet introduced patient reporting.
A recent systematic review confirmed that patient reports contribute positively to the practice of pharmacovigilance [2]. While research has found that the clinical information provided in the reports differs little from that in HCP reports [3], patient reports typically contain more detailed information on quality of life, severity of ADRs, and circumstances of use [3,4,5,6]. The use of patient information in signal assessment is key to addressing the patient’s perspective in drug safety [2, 6,7,8,9].
Experience has shown that patient reports contribute to signal detection both in case-by-case review and in using disproportionality analyses to detect signalsFootnote 1 [11, 12]. Additionally, examples exist where patient reports were the primary source for signals, for both registered drugs and natural health products [7, 8, 13]. However, the contribution of patient reports to signal detection has mostly been studied in European countries, and data quantifying the contribution of patient reports are limited. In the Netherlands between 2003 and 2008, a total of 9% of the reports in published signals were received directly from patients [11]; in 2010–2015, this had increased to 26% on average [14]. In the UK, 53 of the 277 signals investigated by the Medicines & Healthcare products Regulatory Agency (MHRA) in 2010 contained reports from patients. In 15 signals, the index case was a patient report [15].
Descriptions of methodologies for using patient reports in signal detection are scarce. Despite the increased promotion of and progress in the collection of patient reports in pharmacovigilance, some national centres do not routinely include them in their data analysis, or they struggle with how to best use information directly from patients [7, 13].
Finally, published evidence of the contribution patient reports make to signal detection using internationally collected reports is limited. To explore the nature of safety signaling on patient reports in an international setting, the Uppsala Monitoring Centre (UMC) and the Netherlands Pharmacovigilance Centre Lareb collaborated in a signal-detection workshop focused on patient reports in VigiBase, the World Health Organization (WHO) global database of individual case safety reports (ICSRs) [16]. The objective of this paper is to describe the results and reflections from this exploration.
2 Methods
2.1 Dataset
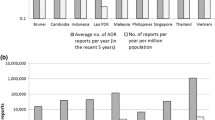
The dataset used was extracted from VigiBase on 1 September 2016, when it contained more than 13 million reports. “Patient reports” were defined as reporter type “Consumer/non-health professional” according to the E2B reporting standard [17] and consisted of 3.6 million reports. Not all patient reports in VigiBase could be captured, as reports with older reporting formats lacked the structured information identifying them as reported by patients. Figure 1 provides an overview of the number of patient reports in VigiBase over the years.
A pilot study was performed prior to the workshop to understand reporting patterns and specific features of patient reports in VigiBase and to define the inclusion and exclusion criteria for the drug–adverse event combination list (hereafter referred to as drug–event combinations). In this pilot study, a set of randomly selected serious and non-serious reports were manually reviewed in depth, and patient report features were quantitatively compared with all other reports in VigiBase.
Suspected duplicate reports were removed using the vigiMatch algorithm [18, 19], and reports from patient support programs/studies were excluded given concerns for both their active form of collection (i.e., not true spontaneous reports) and their poor completeness.
A drug–event combinations assessment list was generated using both patient and non-patient reports. Combinations were included in the list if they fulfilled the following criteria: more than 50% patient reports within the combination and at least one patient report received in 2014 or later (to focus on current issues). Case series with 30 patient reports or less were included in the primary manual review to balance the chance of identifying new potential signals with the feasibility of an in-depth assessment of all reports included in the case series during the workshop.
vigiRank, a predictive model using multiple strength-of-evidence aspects, was used to rank the combinations according to the likelihood of the combinations being potential signals [20]. The vigiRank algorithm was applied only to the patient reports within a given combination.
The WHODrug dictionary preferred base was used to define the substance, and the Medical Dictionary for Regulatory Activities (MedDRA®) preferred term was used to define the event in the ‘drug–event’ combination list.
The drug–event combinations included both serious and non-serious events to encompass any reaction that would be of concern for a patient.
2.2 Signal Detection and Assessment Process
During the workshop, a multidisciplinary team of pharmacists, physicians, and data scientists from UMC and Lareb conducted a primary assessment of statistically highlighted drug–event combinations. The aim of the workshop was to investigate the feasibility of identifying “potential signals” (i.e., drug–event combinations requiring further in-depth clinical assessment) from case series comprising a majority of patient reports. Based on previous experience and the estimated manual capacity to clinically assess potential signals, a goal of finding nine potential signals during the 4-day workshop was set. The signal-detection workshop ended when the targeted number of potential signals was met. However, when this goal was reached, some drug–event combinations were still undergoing assessment, resulting in an additional two, and thus a final total of 11, potential signals.
The primary assessment of the drug–event combinations included a review of the case narratives for information required to assess causality and describing the patient’s perception of the event. It also included a review of the product information regarding the ADRs, as recommended in Council for International Organizations of Medical Sciences (CIOMS) guidance [10]. While traditional UMC signal assessment includes only a review of drug product information for HCPs, patient information leaflets (PILs) were also reviewed in this exercise to ensure ADRs were described in a way that patients could understand. The three main sources, chosen to cover what is most likely known for prescribers globally, were the summary of product characteristics (SmPC) and PILs available at the European Medicines Agency (EMA) [21] or the United Kingdom electronic Medicines Compendium (UKeMC) [22] and the information available at the US DailyMed [23], all available online. When a drug–event combination included a large proportion of reports from a specific country, or the drug product was not licensed in the UK or USA, the local country SmPC (or similar) and patient information were also reviewed. Reports representing drug–event combinations not adequately described in the reviewed drug product information and PILs were clinically assessed for causality and then classified as “adequately labelled, non-signal, keep under review,” or as a “potential signal.” Potential signals later proceeded to a more in-depth clinical review to determine whether the safety concern should be communicated as a “signal” within the WHO programme for international drug monitoring.
3 Results
3.1 Drug–Event Combinations
In total, during the workshop primary assessments, 212 drug–event combinations were reviewed, including both patient and non-patient reports from 74 countries. See Table 1 for country distribution. Of these, 116 (55%) combinations were classified as adequately labelled in the PIL, 68 (32%) were non-signals, eight (4%) were combinations to be kept under review, and 20 (9%) combinations were joined to be classified as 11 potential signals (similar event terms and drugs being combined). Further in-depth assessment of the 11 potential signals resulted in two non-signals, one keep under review, and eight signals that were communicated within the WHO programme for international drug monitoring and subsequently made publicly available in the WHO Pharmaceuticals Newsletter [24]. Five signals described previously unlabeled suspected ADRs, whereas three described new relevant aspects of previously known ADRs, e.g., regarding severity or previously inadequate descriptions in the PILs. Table 2 provides an overview of the signals.
The proportion of patient reports within the combinations varied between 51 and 100%; the combination with the highest proportion of patient reports (94%) was desogestrel–panic attacks, which was classified as a signal together with the adverse events suicidal ideation and self-injurious behavior. Among the patient reports within the combinations, the sex distribution was 2347 (70%) reports from females, 915 (27%) reports from males, and 92 (3%) reports for which the sex was unknown. The patient sex distribution for VigiBase as a whole is 57% female, 37% male, and 6% unknown.
Levothyroxine and desogestrel were the drugs that most frequently occurred (Table 3) among the reviewed combinations in the combination list. Possible explanations could be their widespread use or high reporting rates secondary to public media coverage and/or known patient association concerns for the drugs in some countries, e.g., Netherlands and Sweden [21, 25].
Most of the events were non-serious, such as constipation, abdominal pain, and alopecia (Table 4).
3.2 Signals Describing New Suspected Adverse Reactions
The signals of new, unlabeled ADRs were depression with desloratadine; panic attack, suicidal ideation, and self-injurious behavior with desogestrel; color vision distortion with pregabalin; panic attacks with levothyroxine; and dry eyes with amitriptyline.
Reviewing the report narratives allowed identification of signals that may have been overlooked or misinterpreted by the treating physicians. In the levothyroxine–panic attacks signal, many symptoms associated with panic attacks, such as tremor, tachycardia or irregular heartbeat, and sweating are listed and suggestive of levothyroxine overdose. In these reports, neither the patients nor the physicians recognized that the severity of these symptoms could present as panic attacks; they therefore missed an opportunity to alleviate the symptoms by lowering the dose. Therefore, the product label should be reviewed and updated.
In the amitriptyline–dry eyes signal, the reaction could have been considered an expected finding as it is a known manifestation of the anticholinergic effects of the drug. In a more routine signal-detection exercise, this combination would likely be considered as “known,” as its anticholinergic effects should be known to HCPs. However, “dry eyes” is not listed as an ADR in either the SmPCs or the PILs, leaving patients without information that the reaction could be caused by the drug and HCPs without an important reminder.
3.3 Signals Describing New Aspects of Previously Known Adverse Reactions
Some signals described new aspects of previously known ADRs. They were loss of libido with systemic hormonal contraceptives; genital pruritus with sodium glucose-linked transporters subtype 2 (SGLT-2) inhibitors; and headache, stomach ache, and chest pain with noscapine.
The first two signals are examples of known ADRs that are labelled in the product information and where patient report narratives described new aspects of the ADRs that were deemed relevant to communicate.
The first, loss of libido, was highlighted for two systemic hormonal contraceptives, desogestrel (monotherapy) and the combined oral contraceptive ethinylestradiol/levonorgestrel. In one of the case narratives, the patient questioned the necessity of taking the drug “if you never want to have sex.” A review revealed that “decreased libido” and “changes in libido” were included in labels for almost all systemic hormonal contraceptives, but (complete) loss of libido was not, suggesting that current labelling is not sufficiently informative to patients.
The second signal initially highlighted the event genital pruritus with dapagliflozin. Genital pruritus is a well-known ADR for all currently marketed SGLT-2 inhibitors, which mediate their action by inducing loss of glucose through the urine. The patient narratives revealed that pruritus could be described as “severe” and with additional, unintended consequences, such as “orgasm-like feeling during several days.” Furthermore, a large proportion of the patients experiencing the ADR discontinued use of the medication. Current labelling fails to inform of the potential severity of the ADR, nor does it provide advice on potential management or the need to discuss discontinuation of the medication with HCPs.
In the third case, the signal for noscapine is an example of known ADRs being inconsistently labelled between countries. Noscapine was highlighted with reports from five main countries for the events headache, stomach ache, and chest pain. These events were assessed as being adequately labelled in three countries, insufficiently labelled in one, and not labelled at all in the last two countries. The signals were forwarded in full to the two relevant reporting countries and communicated in brief to the rest of the network.
3.4 Patient Information Leaflets
The PIL should be a direct reflection of the information included in the SmPC for HCPs, presented in a way that most patients can understand. As stated in the Best Practice Guidance for Patient Information Leaflets from the UK MHRA; “Good information helps patients to participate fully in concordant decision-making about medicines prescribed for or recommended to them by healthcare professionals” [26].
During this workshop, we observed cases where PILs could be improved to help patients make well-informed decisions regarding their drug treatment. Highlighting the importance of clarity and context for ADRs is exemplified by looking for the ADR “blurred vision” in two different PILs. The ADR was found under “eye problems” in one PIL and under “anticholinergic effects” in another. Most patients would find the latter a less obvious place to search for the event [27, 28].
Examples of poor consistency between the PIL and the SmPC were observed. During the review of the combination of nitrofurantoin and neuropsychiatric effects, the Sm PC used more vivid and descriptive terms (depression, euphoria, confusion, psychotic reactions), whereas the PIL used general wording that could be more difficult for patients to interpret (extreme changes of mood or mental state) [28].
We also found good examples of particularly informative and patient-oriented PILs. One example is a PIL for an oral contraceptive that put the potential ADR into a clearer context, comparing the risks of blood clots for women taking the drug with those for women not taking the drug and pregnant women:
Your chances of having a blood clot are increased by taking the pill. • Of 100,000 women who are not on the pill and not pregnant, about 5–10 may have a blood clot in a year. • Of 100,000 women taking a pill like Erlibelle, 30–40 may have a blood clot in a year, the exact number is unknown. • Of 100,000 women who are pregnant, around 60 may have a blood clot in a year [29].
3.5 Patient Narratives
According to the International Conference on Harmonization (ICH) E2B guideline [17], a report narrative is the “original reporter’s words and/or short phrases used to describe the reaction/event.” A “focused, factual and clear description of the case should be given, including the words or short phrases used by the reporter” [17].
One of the known benefits of patient reports is that they provide more information on the severity of the experienced events as well as how these events impact their quality of life [3]. The signals detected in this signal-detection workshop provided several illustrative examples of valuable patient narratives.
In the signal of noscapine, the case narratives reported events concerning severity: “this [chest and abdominal pain] went on for a couple of hours,” during which the patient felt “a sense of doom/death on account of the pain.” Another reported “horrible pain, I was completely sure that I had gotten a heart attack or aneurysm.”
A narrative describing panic attacks with levothyroxine illustrates both the severity and the impact of the experienced events: “Severe panic attacks, chest pain, anger and mood swings, difficulty breathing, headaches, feeling dizzy and ‘spaced out,’ neck pain and blocked nasal passage. Possibly an error in dosing but they were only 25 mg [sic], which I understand is a low dosage. Once stopped the symptoms began to disperse. A thoroughly unpleasant and frightening experience. Will certainly not be taking any more of this thyroid medication.” The patient revealed that the ADR had a large enough impact on her that she made a personal assessment to stop taking the medication.
Patient narratives assessed also revealed that patients often make causality assessments based on their individual experiences, noting such observations as a positive de-challenge on stopping the drug. “Severe depression, anxiety and panic attacks. Sought additional treatment for depression/anxiety from general practitioner but symptoms abated once stopped taking [the drug].” Similarly, another woman described her panic attacks and how they disappeared when she stopped taking the drug as “Episodes of anxiety, panic and panic attacks in pressured situations. I connected this to my current life situation before I stopped [the drug]. At the same time, the panic attacks I anticipated in certain situations did not occur. I did never suspect [the drug] to have any role in my anxiety or panic attacks before I stopped the drug and realized that my problems went away. Thinking back, I realize that my problems started in the same period as I started taking [the drug].”
Finally, we found evidence from patient narratives that patients review PILs in the context of their individual experiences as well as making risk assessments and recommendations for others. One example from a patient described ADRs experienced with nitrofurantoin: “This is to report that I had in addition to the vast majority of ‘Possible side effects’ listed in the leaflet, I have suffered severe side effects … memory gaps whist talking … severe disorientation … horrendous headaches feeling my skull was going to explode … I would not wish anybody of my age to suffered from these side effects to and I think this tablets should be withdrawn from the market if prescribed to the elderly.”
4 Discussion
This is the first description of signal-detection results and reflections based on patient reports in a global database. It demonstrates that adjustments to statistical signal-detection algorithms and assessment can be implemented to focus on safety concerns reported by patients.
The drug–event combinations assessed in this workshop mostly concerned drugs that have been on the market for long periods of time and non-serious events. Current statistical signal detection performed in large databases by industry and regulatory authorities prioritize ADR reports for review using “seriousness” designations of case reports and targeted medical events [30]. Also, reports received for newer drugs are typically a focus in pharmacovigilance, particularly drugs whose licensure may have been subject to rapid or accelerated reviews.
The patient narrative was key in both the identification and the assessment of signals within this workshop. Through the narratives, patients told their stories, which described the severity of the reaction as experienced by the patient, what impact it had on their quality of life, and what actions they took with the drug. Reviewing these stories allowed our clinical assessors to identify signals of ADRs that may have been overlooked or misinterpreted by the treating physicians (e.g., panic attacks and levothyroxine) and of new aspects of ADRs already included in the labelling (e.g., genital pruritus and dapagliflozin).
Case-by-case signal detection allows assessors to take the rich patient narratives into account and is encouraged when possible. However, personnel constraints or the sheer size of the database mean case-by-case review is not feasible as the primary mode of signal detection in some settings. Using statistical signal detection only based upon disproportionality of single ADR terms does not consider the content of the narrative; narratives are only reviewed after suspect drug–event combinations are identified; signals that are only possible to identify from narratives will go undetected.
Using the PIL in the assessment of drug–event combinations was a novel approach compared with routine signal-detection practice within the UMC, which uses product information written for HCPs. A comparison of the PIL with patient narratives enabled some insights into how patients comprehend and use safety information provided by regulatory authorities as well as into how the information is presented to patients. Access to good-quality information about ADRs should be as easy accessible as possible for patients and, when such information exists, it should contain descriptions of the reactions, including severity information and—most importantly—what to do when adverse reactions are experienced.
The conclusions drawn from our experiences in the patient signal-detection workshop in a global database have some limitations. As the maturity of patient reporting in the national pharmacovigilance systems differs between countries within the WHO programme for international drug monitoring, reports from countries with more established systems (e.g., the Netherlands, the USA, South Korea) are over-represented. Countries that provide narratives were more likely to contribute to the assessments in our workshop. However, only narratives written in languages that at least one of the participating staff could read could contribute to the signal evaluation. For example, South Korea contributed a large number of patient reports, but unfortunately the narratives could not be included in the assessments. Notably, some countries, such as the USA, contribute many reports but do not share narratives into VigiBase. It should also be noted that the quality of case narratives varies widely within the database. Patient stories are collected and captured in reports in different ways; some stories are transcribed into a short summary by staff at the national pharmacovigilance centre, others are automatically constructed by computer algorithms from data captured in structured report fields, and some patient stories may be reflected as originals in the reporting form.
To take full advantage of the information in patient reports available to pharmacovigilance, re-thinking current strategies for signal detection should be considered with emerging methods such as natural language processing of data within narratives as a complement to traditional disproportionality methods. Inclusion of new data-collection fields regarding severity grading or reporting on decisions to stop medications would allow for more consistent and structured capture of such data from patient reports. Currently the local reporting forms for some countries (e.g., Italy, the UK, and the Netherlands) ask for information on the impact of an ADR on quality of life, but these countries have different ways of soliciting such information. With the growing amount of available unstructured information, the application of text mining to ICSRs is a potential way to make use of the richness of patient ADR experiences [31].
5 Conclusion
Safety concerns reported directly by patients can be identified in a global database. Case narratives provided by patients tell stories that more fully describe their experiences with ADRs. Case-by-case review to identify potential signals from patient reports is preferable whenever possible as it ensures review of these patient stories. Novel approaches to highlighting patient reports in statistical signal detection should be considered to make better use of their important contribution within pharmacovigilance.
Notes
CIOMS signal definition: “information that arises from one or multiple sources (including observations or experiments), which suggests a new, potentially causal association, or a new aspect of a known association between an intervention (e.g., administration of a medicine) and an event or set of related events, either adverse or beneficial, that is judged to be of sufficient likelihood to justify verificatory action” [10].
References
Council Directive (EC). Council Directive (EC) 2010/84/EC of 15 December 2010 on the Community code relating to medicinal products for human use. Off J Eur Union. 2010. https://ec.europa.eu/health/sites/health/files/files/eudralex/vol-1/dir_2010_84/dir_2010_84_en.pdf. Accessed 20 May 2017.
Inacio P, Cavaco A, Airaksinen M. The value of patient reporting to the pharmacovigilance system: a systematic review. Br J Clin Pharmacol. 2017;83(2):227–46.
Rolfes L, van Hunsel F, Wilkes S, van Grootheest K, van Puijenbroek E. Adverse drug reaction reports of patients and healthcare professionals: differences in reported information. Pharmacoepidemiol Drug Saf. 2015;24(2):152–8.
Avery AJ, Anderson C, Bond CM, Fortnum H, Gifford A, Hannaford PC, et al. Evaluation of patient reporting of adverse drug reactions to the UK ‘Yellow Card Scheme’: literature review, descriptive and qualitative analyses, and questionnaire surveys. Health Technol Assess. 2011;15(20):1–234 (iii–iv).
van Hunsel F, Passier A, van Grootheest K. Comparing patients’ and healthcare professionals’ ADR reports after media attention: the broadcast of a Dutch television programme about the benefits and risks of statins as an example. Br J Clin Pharmacol. 2009;67(5):558–64.
Harmark L, van Hunsel F, Grundmark B. ADR reporting by the general public: lessons learnt from the Dutch and Swedish systems. Drug Saf. 2015;38(4):337–47.
Matos C, Harmark L, van Hunsel F. Patient reporting of adverse drug reactions: an International Survey of National Competent Authorities’ Views and Needs. Drug Saf. 2016;39(11):1105–16.
van Hunsel F, Harmark L, Pal S, Olsson S, van Grootheest K. Experiences with adverse drug reaction reporting by patients: an 11-country survey. Drug Saf. 2012;35(1):45–60.
Vilhelmsson A, Svensson T, Meeuwisse A, Carlsten A. Experiences from consumer reports on psychiatric adverse drug reactions with antidepressant medication: a qualitative study of reports to a consumer association. BMC Pharmacol Toxicol. 2012;13:19. doi:10.1186/2050-6511-13-19
Council for International Organizations of Medical Sciences. Practical aspects of signal detection in pharmacovigilance: Report of CIOMS Working Group VIII. Geneva: CIOMs; 2010.
van Hunsel F, Talsma A, van Puijenbroek E, de Jong-van den Berg L, van Grootheest K. The proportion of patient reports of suspected ADRs to signal detection in the Netherlands: case-control study. Pharmacoepidemiol Drug Saf. 2011;20(3):286–91.
Hazell L, Cornelius V, Hannaford P, Shakir S, Avery AJ, Yellow Card Study C. How do patients contribute to signal detection? A retrospective analysis of spontaneous reporting of adverse drug reactions in the UK’s Yellow Card Scheme. Drug Saf. 2013;36(3):199–206.
Sarinic V, Di Giusti M, Banovac M, et al. SCOPE Work Package 4: Survey Report, Topic 2 Patient reporting. 2016. http://www.scopejointaction.eu/_assets/files/SCOPE-WP4-Topic-1,2,5-survey-report.pdf. Accessed 1 May 2017
van Hunsel F, de Waal S, Härmark L. The contribution of direct patient reported ADRs to drug safety signals in the Netherlands from 2010 to 2015. Pharmacoepidemiol Drug Saf. 2017;26(8):977–83.
Foy MGS, Cumber S, Jadeja MM. The yellow card scheme: patient reporting of adverse drug reactions and signals they have generated [abstract]. Drug Saf. 2011;34(10):903.
Lindquist M. Vigibase, the WHO Global ICSR database system: basic facts. Drug Inf J. 2008;42(5):409–19.
International conference on harmonisation of technical requirements for registration of pharmaceuticals for human use expert working group. ICH guideline on clinical safety data management: data elements for transmission of individual case safety reports E2B (R2). ICH. 2001. http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E2B/Step4/E2B_R2__Guideline.pdf. Accessed 1 May 2017.
Tregunno PM, Fink DB, Fernandez-Fernandez C, Lazaro-Bengoa E, Noren GN. Performance of probabilistic method to detect duplicate individual case safety reports. Drug Saf. 2014;37(4):249–58.
Norén GN, Orre R, Bate A, Edwards IR. Duplicate detection in adverse drug reaction surveillance. Data Min Knowl Discov. 2007;14:305–28.
Caster O, Juhlin K, Watson S, Noren GN. Improved statistical signal detection in pharmacovigilance by combining multiple strength-of-evidence aspects in vigiRank. Drug Saf. 2014;37(8):617–28.
European Medicines Agency. European Medicines Agency update on combined contraceptives [media release]. 2013. http://www.ema.europa.eu/ema/index.jsp?curl=pages/news_and_events/news/2013/01/news_detail_001688.jsp&mid=WC0b01ac058004d5c1. Accessed 1 November 2013.
Datapharm. Electronic Medicines Compendium. 2017. http://www.medicines.org.uk/. Accessed 20 Jan 2017.
US National Library of Medicine. DailyMed. https://dailymed.nlm.nih.gov/dailymed/index.cfm. Accessed 20 Jan 2017.
World Health Organization. WHO Pharmaceuticals Newsletter. http://www.who.int/medicines/publications/newsletter/en/. Accessed 20 May 2017.
Rolfes L, van Hunsel F, Taxis K, van Puijenbroek E. The impact of experiencing adverse drug reactions on the patient’s quality of life: a retrospective cross-sectional study in the Netherlands. Drug Saf. 2016;39(8):769–76.
Medicines & Healthcare products. Regulatory Agency, UK, Best practice guidance on patient information leaflets. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/328405/Best_practice_guidance_on_patient_information_leaflets.pdf. Accessed 15 Mar 2017.
Electronic Medicines Compendium. Amitriptyline 10mg, 25mg and 50mg tablets [patient information leaflet]. Barnstable: Actavis. 2017. https://www.medicines.org.uk/emc/PIL.18030.latest.pdf. Accessed 20 Apr 2017.
Electronic Medicines Compendium. Amitriptyline hydrochloride 10mg/5ml oral solution [patient information leaflet]. Wrexham: Wockhardt. 2017. https://www.medicines.org.uk/emc/PIL.32813.latest.pdf. Accessed 20 Apr 2017.
Electronic Medicines Compendium. Erlibelle 30micrograms/150micrograms film-coated tablets [patient information leaflet]. https://www.medicines.org.uk/emc/medicine/28955. Accessed 18 Apr 2017.
European Medicines Agency. Inspections, Human Medicine, Pharmacovigilance and Committees Division. Screening for adverse reactions in EudraVigilance. EMA/849944/2016. London: EMA; 2016. http://www.ema.europa.eu/docs/en_GB/document_library/Other/2016/12/WC500218606.pdf. Accessed 20 May 2017.
Jacobsson R, Bergvall T, Sandberg L, Ellenius J. Extraction of Adverse Event Severity Information from Clinical Narratives Using Natural Language Processing. Pharmacoepidemiology and Drug Safety, 2017; 26(Suppl. 2): 37.
Acknowledgements
The authors are indebted to all the patients who reported their experiences as well as the national centres contributing the reports to VigiBase. The opinions and conclusions in this study are not necessarily those of the various national centers nor of the WHO. We would also like to thank Jeltje Boer, Ellen Ederveen, and Niklas Norén for their contributions in the workshop.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist in the preparation of this study.
Conflicts of interest
Sarah Watson, Rebecca E. Chandler, Henric Taavola, Linda Härmark, Birgitta Grundmark, Alem Zekarias, Kristina Star, and Florence van Hunsel have no conflicts of interest that are directly relevant to the content of this study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Watson, S., Chandler, R.E., Taavola, H. et al. Safety Concerns Reported by Patients Identified in a Collaborative Signal Detection Workshop using VigiBase: Results and Reflections from Lareb and Uppsala Monitoring Centre. Drug Saf 41, 203–212 (2018). https://doi.org/10.1007/s40264-017-0594-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-017-0594-2