Abstract
Introduction
Patient reporting of adverse drug reactions (ADRs) to spontaneous reporting systems can make a valuable contribution to pharmacovigilance. However, the implementation and promotion of patient reporting systems (PRSs) differ worldwide.
Objective
The objective of the study was to describe attitudes toward PRSs, and progress toward implementing such systems among national competent authorities participating in the World Health Organization Programme for International Drug Monitoring.
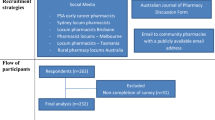
Methods
A web-based questionnaire was constructed based on qualitative interviews, and distributed through SurveyMonkey® to all countries listed on the World Health Organization Programme for International Drug Monitoring (n = 178) during November and December of 2015. Data were analyzed using descriptive statistics and Chi-square tests.
Results
A total of 143 valid questionnaires were received from 141 countries (79.2 %). A spontaneous reporting system for both healthcare professionals and patients was present in 58 countries (41.1 %). An official PRS to report ADRs directly was implemented in 44 countries (31.2 %) and in a pilot stage in five countries (3.5 %). Patients were not allowed to report in 34 countries (24.1 %). The reasons for not having an official PRS were mainly a lack of resources/budget (56.5 %) or a lack of information/education for patients (56.5 %). When analyzing the attitudes among the respondents toward a PRS, most acknowledge that the general public contributes to the detection or strength of drug safety signals (82.2 % agree or strongly agree) and with information that is not present in healthcare professional reports (80.7 % agree or strongly agree). For respondents, giving feedback to patients could be an incentive for patients to report more (80.8 % agree or strongly agree). To be able to further PRSs, guidelines on promoting a PRS efficiently to the general public (87.4 % agree or strongly agree), training courses/conferences (86.7 % agree or strongly agree), or a public list of Lareb’s scientific publications (86.7 % agree or strongly agree) were the support measures most well accepted by the respondents.
Conclusions
Most countries accept ADR reports from patients by an official reporting system designed for patients or through the existing system for healthcare professionals. The main reasons for not having a PRS is financial restraints and a lack of information/education of patients. Attitudes toward a PRS are positive, but some countries fear that they will not be able to handle an increase in reports.
Similar content being viewed by others
References
Härmark L, van Hunsel F, Grundmark B. ADR reporting by the general public: lessons learnt from the Dutch and Swedish systems. Drug Saf. 2015;38(4):337–47.
Blenkinsopp A, Wilkie P, Wang M, Routledge PA. Patient reporting of suspected adverse drug reactions: a review of published literature and international experience. Br J Clin Pharmacol. 2007;63(2):148–56.
van Hunsel F, Talsma A, van Puijenbroek E, et al. The proportion of patient reports of suspected ADRs to signal detection in the Netherlands: case-control study. Pharmacoepidemiol Drug Saf. 2011;20(3):286–91.
Ahmad SR. Comment on:“adverse drug reaction reporting by patients: an overview of fifty countries”. Drug Saf. 2015;38(1):109–10.
Margraff F, Bertram D. Authors’ reply to Ahmad SR:“adverse drug reaction reporting by patients: an overview of fifty countries”. Drug Saf. 2015;38(1):111.
Margraff F, Bertram D. Adverse drug reaction reporting by patients: an overview of fifty countries. Drug Saf. 2014;37(6):409–19.
Herxheimer A, Crombag M, Alves TL. Direct patient reporting of adverse drug reactions: a fifteen-country survey and literature review. Amsterdam: Health Action International (HAI) Europe; 2010 (Paper Series Reference 01–2010/05). http://haieurope.org/wp-content/uploads/2010/12/10-May-2010-Report-Direct-patient-reporting-of-adversedrug-reactions.pdf.
van Hunsel F, Härmark L, Pal S, et al. Experiences with adverse drug reaction reporting by patients. Drug Saf. 2012;35(1):45–60.
EC. Directive 2010/84/EU of the European Parliament and of the Council of 15 December 2010 amending, as regards pharmacovigilance. Directive 2001/83/EC on the Community code relating to medicinal products for human us [online]. http://ec.europa.eu/health/files/eudralex/vol-1/dir_2010_84/dir_2010_84_en.pdf. Accessed 30 May 2016.
Borg J-J, Aislaitner G, Pirozynski M, Mifsud S. Strengthening and rationalizing pharmacovigilance in the EU: where is Europe heading to? Drug Saf. 2011;34(3):187–97.
Matos C, van Hunsel F, Joaquim J. Are consumers ready to take part in the pharmacovigilance system? A Portuguese preliminary study concerning ADR reporting. Eur J Clin Pharmacol. 2015;71(7):883–90.
McLernon DJ, Bond CM, Lee AJ, et al. Patient views and experiences of making adverse drug reaction reports to the Yellow Card Scheme in the UK. Pharmacoepidemiol Drug Saf. 2011;20(5):523–31.
Robertson J, Newby DA, Robertson J. Low awareness of adverse drug reaction reporting systems: a consumer survey. Med J Aust. 2013;199(10):684–6.
Jha N, Rathore DS, Shankar PR, et al. Need for involving consumers in Nepal’s pharmacovigilance system. Australas Med J. 2014;7(4):191–5.
Fortnum H, Lee AJ, Rupnik B, Avery A. Survey to assess public awareness of patient reporting of adverse drug reactions in Great Britain. J Clin Pharm Ther. 2012;37(2):161–5.
van Hunsel F, van Puijenbroek E, de Jong-van den Berg L, van Grootheest K. Media attention and the influence on the reporting odds ratio in disproportionality analysis: an example of patient reporting of statins. Pharmacoepidemiol Drug Saf. 2010;19(1):26–32.
Olsson S. The role of the WHO programme on international drug monitoring in coordinating worldwide drug safety efforts. Drug Saf. 1998;19(1):1–10.
Lareb. Conference on patient reporting. 2015. http://www.lareb.nl/whocc/Conference-on-Patient-Reporting. Accessed 13 Jul 2016.
Lareb. Netherlands Pharmacovigilance Centre Lareb training courses. 2015. http://www.lareb.nl/whocc/Training-courses?lang=en-GB. Accessed 24 Jul 2016.
SurveyMonkey. Sending surveys via email invitation. 2016. http://help.surveymonkey.com/articles/en_US/kb/Email-Invitation-Collector. Accessed 14 Jul 2016.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrance Eribaum Association; 1988.
United Nations. United Nations Member States. http://www.un.org/en/member-states/. Accessed 27 Jul 2016.
Danish Medicines Agency. The Danish Medicines Agency’s annual pharmacovigilance report 2009. Annual Report. 2010.
Faasse K, Cundy T, Petrie KJ. Thyroxine: anatomy of a health scare. BMJ. 2009;339:b5613.
Opaleye ES, Noto AR, Zv Sanchez, et al. Recreational use of benzydamine as a hallucinogen among street youth in Brazil. Rev Bras Psiquiatr. 2009;31(3):208–13.
World Health Organization. Drug Alert 129: Contaminated Dextromethorphan active pharmaceutical ingredient. 2013. http://www.who.int/medicines/publications/drugalerts/App_Drug_Alert_No_129_Paraguay_Dextro.pdf. Accessed 25 April 2016.
ISOP. 11th ISoP annual meeting “Next Stop: Istanbul—Bridging the Continents”, Istanbul, Turkey, 26–28 October, 2011. Drug Saf. 2011;34(10):883–1026.
Olsson MS, Pal SN, Stergachis A, Couper M. Pharmacovigilance activities in 55 low-and middle-income countries. Drug Saf. 2010;33(8):689–703.
Uppsalla Monitoring Center. Joining the WHO Programme for International Drug Monitoring. 2010. http://www.who.int/medicines/areas/quality_safety/safety_efficacy/Joining_the_WHO_Programme.pdf?ua=1. Accessed 24 Jul 2016.
Krause N. A comprehensive strategy for developing closed-ended survey items for use in studies of older adults. J Gerontol Ser B Psychol Sci Soc Sci. 2002;57(5):S263–74.
Sue VM, Ritter LA. Conducting online surveys. Thousand Oaks, CA: Sage Publications; 2007.
Pal SN, Olsson S, Brown EG. The Monitoring Medicines Project: a multinational pharmacovigilance and public health project. Drug Saf. 2015;38(4):319–28.
Plöen M, Wallberg M, Olsson S. User-driven development of a web-based tool for patient reporting of drug-related harm. Drug Saf. 2015;38(4):359–64.
World Health Organization. Safety monitoring of medicinal products: reporting system for the general public. Geneva: WHO; 2012.
Ghosh R, Lewis D. Aims and approaches of Web-RADR: a consortium ensuring reliable ADR reporting via mobile devices and new insights from social media. Expert Opin Drug Saf. 2015;14(12):1845–53.
Web-RADR project. https://web-radr.eu/. Accessed 30 May 2016.
Leone R, Moretti U, D’Incau P, et al. Effect of pharmacist involvement on patient reporting of adverse drug reactions: first Italian study. Drug Saf. 2013;36(4):267–76.
Parretta E, Rafaniello C, Magro L, et al. Improvement of patient adverse drug reaction reporting through a community pharmacist-based intervention in the Campania region of Italy. Expert Opin Drug Saf. 2014;13(Suppl. 1):21–9.
Härmark L, Raine J, Leufkens H, et al. Patient-reported safety information: a renaissance of pharmacovigilance? Drug Saf. 2016. doi:10.1007/s40264-016-0441-x.
Acknowledgments
The authors thank Anna Hegerius, PharmD at the Uppsala Monitoring Centre, WHO Collaborating Centre for International Drug Monitoring, Sweden for her feedback on the questionnaire.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist in the preparation of this article.
Conflicts of interest
Cristiano Matos, Linda Härmark, and Florence van Hunsel have no conflicts of interest that are directly relevant to the content of this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Matos, C., Härmark, L. & van Hunsel, F. Patient Reporting of Adverse Drug Reactions: An International Survey of National Competent Authorities’ Views and Needs. Drug Saf 39, 1105–1116 (2016). https://doi.org/10.1007/s40264-016-0453-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-016-0453-6