Abstract
Background
In 2005, spontaneous reporting of adverse drug reactions (ADRs) to the UK’s Yellow Card Scheme (YCS) was extended to include patient reports. Here, we investigate the potential pharmacovigilance impact of patient reporting.
Objectives
The aim of the study was to investigate the relative contribution of patient reporting to signal detection through disproportionality analysis.
Methods
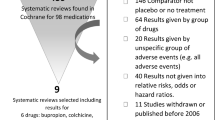
Data were analysed from all reports submitted directly to the YCS between October 2005 and September 2007. Three datasets of drug–ADR pairs were created: one for patient reports, one for healthcare professional (HCP) reports and one for all reports combined. The proportional reporting ratio (PRR) method was used to identify signals of disproportionate reporting (SDRs) in each dataset. The number of SDRs identified from patient and HCP reports were compared, as well as the type of ADR and suspect drug involved. A sensitivity analysis was performed to examine how combining the patient and HCP reports may affect the SDRs identified.
Results
Data were received for 5,180 patient and 20,949 HCP reports, relating to 16,566 and 28,775 drug–ADR pairs, respectively, with 4,340 (10.6 %) pairs found in both datasets. A significantly higher proportion of the SDRs identified from HCP reports involved reactions classified as serious by the Medicines and Healthcare products Regulatory Agency (MHRA), compared with patient reports (n = 931, 48.0 % vs. n = 185, 28.5 %), or involved newly marketed drugs (n = 596, 30.7 % vs. n = 71, 10.9 %). The proportion of SDRs assessed as not listed on the Summary of Product Characteristics (SPC) was similar in each group (~15 %, based on a random sample). After combining the patient and HCP reports, 278 (~11 %) of the SDRs identified when each group was analysed separately no longer met the SDR criteria, including 12 potentially serious ADRs not listed on the product’s SPC. On the other hand, the combined dataset identified an additional 508 SDRs that were not identified when patient or HCP reports were analysed separately. Approximately 10 % (n = 47) of these additional SDRs were assessed as serious ADRs and were not listed on the product’s SPC.
Conclusions
Although this study is limited to the UK experience, overall, the results suggest that patient reporting may provide a positive complementary contribution to that of HCPs. Patient reporting may make an important contribution to drug safety by identifying different SDRs not identified from HCP reports alone. The combination of reports from patients and HCPs, however, when used for the purposes of signal detection through disproportionality analysis, may result in the loss of some information. One possible strategy is to conduct such analyses using reports from patients and HCPs combined, as well as separately for each group.


Similar content being viewed by others
References
MedWatch. MedWatch online voluntary reporting form. Silver Spring: US Food and Drug Administration. 2011. http://www.fda.gov/medwatch/report.htm. Accessed 2 Mar 2011.
Medicines and Healthcare products Regulatory Agency (MHRA). Adverse drug reactions. London: MHRA. 2011. http://www.mhra.gov.uk/Safetyinformation/Reportingsafetyproblems/Reportingsuspectedadversedrugreactions/index.htm. Accessed 2 Mar 2011.
Davis S, King B, Raine J. Spontaneous reporting—UK. In: Mann RD, Andrews EB, editors. Pharmacovigilance. 2nd ed. Chichester: Wiley; 2007. p. 199–215.
Bate A, Evans SJW. Quantitative signal detection using spontaneous ADR reporting. Pharmacoepidemiol Drug Saf. 2009;18(6):427–36.
Hazell L, Shakir SAWS. Under-reporting of adverse drug reactions: a systematic review. Drug Saf. 2005;29:385–96.
Metters J. Report of an independent review of access to the Yellow Card Scheme. London: The Stationery Office; 2004.
van Grootheest AC, de Jong-van den Berg L. Review: patients’ role in reporting adverse drug reactions. Exp Opin Drug Saf. 2004;3:363–8.
de Langen J, van Hunsel F, Passier A, de Jong-van den Berg L, van Grootheest K. Adverse drug reaction reporting by patients in the Netherlands: three years of experience. Drug Saf. 2008;31:515–24.
Egberts TCG, Smulders M, de Koning FHP, Meyboom RHB, Leufkens HGM. Can adverse drug reactions be detected earlier? A comparison of reports by patients and professionals. BMJ. 1996;313:530–1.
Herxheimer A, Crombag M, Alves TL. Direct patient reporting of adverse drug reactions: a fifteen-country survey & literature review (Paper Series Reference 01–2010/05). Amsterdam: Health Action International (HAI) Europe; 2010.
European Commission. The EU pharmacovigilance system. Brussels: European Commission. 2011. http://ec.europa.eu/health/human-use/pharmacovigilance/index_en.htm. Accessed 7 Mar 2011.
McLernon D, Bond CM, Hannaford PC, Watson MC, Lee AJ, Hazell L, Avery AJ, on behalf of the Yellow Card Collaboration. Adverse drug reaction reporting in the UK: a retrospective observational comparison of Yellow Card reports submitted by patients and healthcare professionals. Drug Saf. 2010;33(9):775–88.
WHO Collaborating Centre for Drug Statistics Methodology. ATC structure and principles. Oslo: WHO. 2010. http://www.whocc.no/atc/structure_and_principles/. Accessed 7 Mar 2010.
Medical Dictionary for Regulatory Activities Maintenance and Support Services Organization. Chantilly, VA: MedDRA and the MSSO. 2011. http://www.meddramsso.com/. Accessed 7 Mar 2011.
Evans SJ, Waller PC. Use of proportional reporting ratios (PRRs) for signal generation from spontaneous adverse drug reaction reports. Pharmacoepidemiol Drug Saf. 2001;10:483–6.
EMEA. Guideline of the use of statistical signal detection methods in the Eudravigilance Data Analysis System. London: EMEA. 2006. http://www.emea.europa.eu/pdfs/human/phvwp/10646406en.pdf. Accessed 14 Dec 2009.
Norén GN. Statistical methods for knowledge discovery in adverse drug reaction surveillance (PhD thesis). Stockholm: Stockholm University. 2007. http://su.diva-portal.org/smash/record.jsf?pid=diva2:197004. Accessed 14 Dec 2009.
Aagaard L, Lars Hougaard N, Ebba Holme H. Consumer reporting of adverse drug reactions: a retrospective analysis of the Danish Adverse Drug Reaction Database from 2004 to 2006. Drug Saf. 2009;32:1067–74.
van Hunsel F, Talsma A, van Puijenbroek E, de Jong-van den Berg L, van Grootheest K. The proportion of patient reports of suspected ADRs to signal detection in the Netherlands: case-control study. Pharmacoepidemiol Drug Saf. 2011;20(3):286–91.
Avery AJ, Anderson C, Bond CM, Fortnum H, Gifford A, Hannaford PC, et al. Evaluation of patient reporting of adverse drug reactions to the UK ‘Yellow Card Scheme’: literature review, descriptive and qualitative analyses, and questionnaire surveys. Health Technol Assess. 2011;15(20). http://www.hta.ac.uk/fullmono/mon1520.pdf. Accessed 25 Jan 2013.
Acknowledgments
The MedDRA® trademark is owned by the International Federation of Pharmaceutical Manufacturers & Associations (IFPMA) on behalf of the ICH. Some of the text, tables and figures in this article have been reproduced or adapted from the previously published Health Technology Assessment (no. 1520) [20]. This work was carried out at the DSRU in Southampton, UK. The Yellow Card Study Collaboration also includes Heather Fortnum, Alison Gifford, Janet Krska, Amanda Lee, Elizabeth Murphy, Tim Payne, Claire Anderson, Margaret Watson, David McLernon and Christine Bond. We wish to thank the Yellow Card Study Collaboration Advisory Group for their feedback and the UK MHRA for providing us with their data and assisting with any queries. We also thank Mr Andrew Hauschild, Software Developer, DSRU, and Professor Stephen Evans, Professor of Pharmacoepidemiology, London School of Hygiene and Tropical Medicine, for statistical advice.
Conflict of interest and funding
The DSRU is a registered independent charity (No. 327206) that works in association with the University of Portsmouth. It receives unconditional donations from pharmaceutical companies. These companies have no control over the conduct or publication of studies performed by the DSRU. Saad Shakir has received lecturing fees from the pharmaceutical industry and consultancy fees, although not in relation to the current study. As the current study regards no particular pharmaceutical product, there is no conflict interest. This research was supported by the UK National Health Service Research & Development Programme Health Technology Assessment Programme (project number 06/92/03). The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the Department of Health. The study sponsor did not participate in the study design; in the collection, analysis or interpretation of data; in the writing of the report; or in the decision to submit the paper for publication. All researchers were independent from the funder. The authors have no conflicts of interest to report.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Hazell, L., Cornelius, V., Hannaford, P. et al. How Do Patients Contribute to Signal Detection?. Drug Saf 36, 199–206 (2013). https://doi.org/10.1007/s40264-013-0021-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-013-0021-2