Abstract
Background and Objectives
In the management of attention-deficit hyperactivity disorder (ADHD) in adults it is important to recognize that individual patients respond to a wide range of methylphenidate doses. Studies with methylphenidate modified release long acting (MPH-LA) in children have reported the need for treatment optimization for improved outcomes. We report the results from a post hoc analysis of a 5-week dose optimization phase from a large randomized, placebo-controlled, multicenter 40-week study (9-week double-blind dose confirmation phase, 5-week open-label dose optimization phase, and 26-week double-blind maintenance of effect phase).
Methods
Patients entering the open-label dose optimization phase initiated treatment with MPH-LA 20 mg/day; up/down titrated to their optimal dose (at which there was balance between control of symptoms and side effects) of 40, 60, or 80 mg/day in increments of 20 mg/week by week 12 or 13. Safety was assessed by monitoring the adverse events (AEs) and serious AEs. Efficacy was assessed by the Diagnostic and Statistical Manual of Mental Disorders, fourth edition, Attention-Deficit Hyperactivity Disorder Rating Scale (DSM-IV ADHD RS) and Sheehan Disability Scale (SDS) total scores.
Results
At the end of the dose confirmation phase, similar numbers of patients were treated optimally with each of the 40, 60, and 80 mg/day doses (152, 177, and 160, respectively) for MPH-LA. Mean improvement from baseline in the dose confirmation phase in total scores of DSM-IV ADHD RS and SDS were 23.5 ± 9.90 and 9.7 ± 7.36, respectively.
Conclusions
Dose optimization with MPH-LA (40, 60, or 80 mg/day) improved treatment outcomes and was well-tolerated in adult ADHD patients.
Similar content being viewed by others
At the end of the open-label dose optimization phase, similar numbers of patients were treated optimally with each of 40, 60, and 80 mg/day doses (152, 177, and 160, respectively) for methylphenidate modified release long acting (MPH-LA), indicating that all three doses of MPH-LA are required for optimal treatment of adult attention-deficit hyperactivity disorder (ADHD) patients. |
No new or unexpected safety concerns were observed during the study, and no rebound symptoms were observed upon sudden tapering of the MPH-LA dose. |
Dose optimization with MPH-LA (40, 60, or 80 mg/day) improved treatment outcomes, and MPH-LA was well-tolerated in adult ADHD patients. |
1 Introduction
Stimulants are one of the most commonly used treatments in the management of adult attention-deficit hyperactivity disorder (ADHD), and National Institute for Health and Care Excellence (NICE) guidelines recommend use of methylphenidate as the first-line agent [1]. While studies conducted in children and adolescents with stimulants report a dose–response relationship, in adults such a dose–response relationship has not been clearly established [2–4]. Moreover, studies conducted in children also report that treatment optimization with individual dose titration and careful monitoring of adverse events (AEs) provides improvement in ADHD symptoms and a good tolerability profile [5]. For the treatment of adults with ADHD, the European consensus statement recommends individual dose adjustment based on response and tolerability [6].
Methylphenidate modified release long acting (MPH-LA) is a modified-release formulation of methylphenidate, designed to deliver a bimodal release of the drug so as to mimic a ‘twice-a-day’ dosing regimen. It uses the Spheroidal Oral Drug Absorption System (SODAS) technology comprising 50 % immediate-release formulation and 50 % extended-release beads. In a 40-week randomized, double-blind, placebo-controlled multicenter study using this formulation, comprising three phases [a double-blind dose confirmation phase (9 weeks), open-label dose optimization phase (5 weeks), and double-blind maintenance of effect phase (6 months)], MPH-LA, used at a fixed dose of 40–80 mg/day in adults with ADHD in the 9-week dose confirmation phase, controlled symptoms as well as decreased functional impairment.
NICE guidelines recommend individual, patient-tailored titration of the dose of methylphenidate so as to achieve optimal treatment [1]. Therefore, the open-label dose optimization phase was conducted to determine the optimal dose of MPH-LA, such that during the double-blind maintenance of effect phase patients could receive their optimal dose or placebo and be analyzed for the maintenance of effect of MPH-LA. Thus, it was of interest to study whether all three doses (40, 60, and 80 mg) are optimal in the management of ADHD patients. There was no dose–response relationship observed between the fixed doses used and the response rate during the dose confirmation phase. Moreover, all three doses used were well-tolerated [7]. The main objective of this post hoc analysis of the 5-week open-label dose optimization phase was to evaluate the optimal MPH-LA dose to which patients respond with minimal AEs. It was also of interest to see whether patients who received a particular dose (40, 60, or 80 mg/day) in the 9-week randomized phase continued on the same dose as optimal therapy during the open-label phase.
2 Methods
2.1 Study Design and Treatment
The detailed methodology has been previously described [7] and is briefly summarized here. This study was conducted at 67 sites in nine countries and designed in accordance with the guidelines issued by the European Medical Agency (EMA) (EMEA/CHMP/EWP/431734/2008) with respect to investigation of medicinal products for ADHD treatment. The protocol (NCT01259492) was in line with the Declaration of Helsinki and ethical approval was obtained before the start of the study.
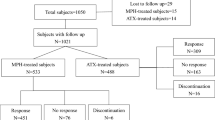
This was a 40-week double-blind, randomized, placebo-controlled, international, multicenter efficacy and safety study of MPH-LA for the treatment of adult patients with ADHD. Both male and female patients (18–60 years) with all types of ADHD according to Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) diagnostic criteria (and a confirmed childhood onset) and a DSM-IV ADHD Rating Scale (DSM-IV ADHD RS) total score of ≥30 at screening and baseline were included in the study. The study design consisted of three treatment phases (Fig. 1), as follows: (1) A 9-week double-blind dose confirmation phase, in which all eligible patients (n = 725) were randomized (1:1:1:1) to once-daily MPH-LA 40, 60, 80 mg/day, or placebo (3-week titration, 6-week fixed dose). Treatment was initiated at a dose of 20 mg/day and increased at weekly intervals in increments of 20 mg/day until the assigned dose of 40 mg, 60 mg, or 80 mg was reached. Following the 3-week titration period, patients received their allocated dose for a period of 6 weeks. (2) A 5-week open-label dose optimization phase, in which all patients, including those treated with placebo in the dose confirmation phase, received MPH-LA. (3) A 6-month double-blind maintenance of effect phase, in which patients were re-randomized in a 3:1 ratio either to their optimal dose of MPH-LA (40, 60, or 80 mg/day) or placebo to evaluate the maintenance effect of MPH-LA in adults with ADHD. During this 6-month withdrawal period, patients with ≥30 % worsening from baseline of this maintenance of effect phase and <30 % remaining improvement from the dose confirmation phase baseline on the DSM-IV ADHD RS were required to discontinue the study due to a lack of therapeutic effect.
Study design including the three study phases and extension study: double-blind dose confirmation phase, open-label dose optimization phase, double-blind maintenance of effect phase, and the long-term safety extension. Reproduced from Huss et al. [7], with kind permission from Springer Science + Business Media
While the dose confirmation phase was designed to evaluate the efficacy and safety of MPH-LA in the treatment of adult ADHD patients using a classic four-arm double-blinded, randomly allocated, forced titration design, the open-label dose optimization phase was designed to evaluate dose of MPH-LA for each individual patient based on open-label systematic clinical judgment. Optimal dose was defined as the dose considered by the investigator as achieving an optimal balance between control of symptoms and AEs that was maintained for a period of at least 1 week prior to the last week (Week 14 of the study) of this phase.
In the open-label dose optimization phase, the dose of MPH-LA was re-titrated on an individual basis for all patients. All patients, including those on placebo during the dose confirmation phase, received MPH-LA starting at 20 mg/day, which was increased at weekly intervals in increments of 20 mg/day until each patient’s optimal dose (40, 60, or 80 mg) was reached. Patients were allowed to down-titrate the dose by 20 mg/day on Week 12 or 13 of the study at the discretion of the investigator. At the last visit, all responders, defined as patients with ≥30 % improvement on the DSM-IV ADHD RS compared to the baseline score at the start of the dose confirmation phase, entered the double-blind maintenance of effect phase.
Non-responders to MPH-LA during the optimization phase, defined as <30 % improvement in DSM-IV ADHD RS compared to the baseline of the dose confirmation phase, were discontinued from the study and treated at the discretion of the investigator.
Subjects with a prior history of poor response, hypersensitivity, or intolerance to stimulants were excluded from the study. Other exclusion criteria included presence of pre-existing cardiovascular, cerebrovascular, or any other psychiatric disorder requiring medical intervention/therapy; pregnancy; seizures; recent alcohol or drug abuse; patients with a ≥30 % improvement in DSM-IV ADHD RS total score at baseline relative to that at screening; and patients on other investigational drugs at the time of enrollment or within 30 days or five half-lives of enrollment (whichever was longer).
2.2 Compliance with Ethics and Guidelines
The study protocol was approved by the institutional review board at each participating center and the study was conducted in accordance with the principles of Good Clinical Practice, the provisions of the Declaration of Helsinki of 1975, as revised in 2000 and 2008, and other applicable local regulations. Written informed consent was provided by all patients before enrollment.
2.3 Assessments
The primary objective of the open-label dose optimization phase was to assess the optimal dose needed for the management of ADHD. Safety assessments included monitoring of all AEs and serious AEs (SAEs) during each week (10, 11, 12, 13, and 14) of this phase. Clinical laboratory parameters and cardiac safety parameters were also monitored. All data were summarized based on the treatment assigned in the dose confirmation phase.
The efficacy measures included the evaluation of both symptomatic and functional domains on various scales, including the DSM-IV ADHD RS, Sheehan Disability Scale (SDS), Clinical Global Impression–Improvement (CGI-I), and Clinical Global Impression–Severity (CGI-S). DSM-IV ADHD RS (total score ranging from 0 to 54) is among the most widely used DSM-based clinician-rated scales and was used to assess ADHD symptoms. The frequency of each symptom for the prior week was recorded by the clinician. SDS (total score ranging from 0 to 30) is a patient self-rating scale used to assess work, social, and family life impairment due to his/her symptoms. Patients were asked to indicate the extent to which their regular activities were affected in the past week on a scale ranging from 0 (not at all) to 10 (extremely). Both DSM-IV ADHD RS and SDS total scores were evaluated as the change from dose confirmation phase baseline to the end of open-label dose optimization phase (14 weeks in total). The CGI-I scale was employed to assess the overall change of illness relative to the baseline for dose confirmation phase. The scale consists of seven ratings ranging from 1 (very much improved) to 7 (very much worse). Improvement on the CGI-I scale reported in this study was defined as a visit rating of 1 (very much improved) or 2 (much improved). The CGI-S was employed to assess the current illness state of the patient. The CGI-S scale also consists of seven ratings ranging from 1 (normal, not at all ill) to 7 (among the most extremely ill patients). Both the CGI-I and CGI-S are clinician rated and were evaluated as the proportion of patients with improvement from dose confirmation phase baseline to the end of open-label dose optimization phase.
DSM-IV ADHD RS and CGI-I measurements were recorded every week during the open-label dose optimization phase, while SDS and CGI-S measurements were recorded at the end (Week 9) of the dose confirmation phase and the end (Week 14) of the open-label dose optimization phase.
2.4 Statistical Analysis
Efficacy data were summarized for all randomized patients who took at least one dose of study medication (full analysis set) during the open-label dose optimization phase and reported by treatment received during the dose confirmation phase. Missing post-baseline scores were imputed based on last observation carried forward (LOCF). No inferential efficacy analyses were performed during this phase. Safety data were summarized for all MPH-LA-treated patients during the open-label dose optimization phase.
3 Results
3.1 Patient Disposition
The patient disposition of the full study has been described previously [7]. Of a total of 863 adult patients (18–60 years) that were screened, 725 patients entered the dose confirmation phase and were randomized to receive once daily dose of MPH-LA 40 mg (N = 181), 60 mg (N = 182), 80 mg (N = 181), or placebo (N = 181). Of these, 584 (80.6 %) patients completed this phase and entered the open-label dose optimization phase. A total of 489 patients completed the open-label dose optimization phase and entered the maintenance of effect phase. During this maintenance of effect phase, as described previously, patients with a lack of therapeutic effect (≥30 % worsening from baseline of maintenance of effect phase in this phase and <30 % remaining improvement from dose confirmation phase baseline on the DSM-IV ADHD RS) were required to discontinue from the study. Thus, overall, 235 patients completed the maintenance of effect phase, marking the end of the full 40-week study period. Patients who did not respond to MPH-LA during the open-label dose optimization phase were not allowed to enter the maintenance of effect phase.
Among the 95 patients who discontinued from the open-label dose optimization phase, unsatisfactory therapeutic effect was the most common reason, reported in 40 patients, followed by AEs (n = 22), withdrawal of consent (n = 20), lost to follow-up (n = 10), and protocol deviation (n = 3). The demographics and baseline characteristics of the patients entering the study has been discussed previously and were similar across patients randomized to the various doses of MPH-LA and placebo in the dose confirmation phase (Table 1).
As defined in the protocol, all patients were initiated on treatment with an open-label dose of 20 mg/day and titration was individualized to achieve the effective dose that was safe. At the end of the 5-week open-label dose optimization phase (Week 14), a similar number of patients were found to be treated optimally with each of the three doses tested: 152, 177, and 160 patients for MPH-LA 40, 60, and 80 mg/day, respectively (Fig. 2). Treatment optimization at the end of the study for the 489 patients, by the randomization treatment received in the dose confirmation phase, is shown in Table 2. There were 125 patients in the dose optimization phase who were randomized to placebo in the prior dose confirmation phase. Of these, 36 patients were optimized to MPH-LA 40 mg, 43 patients to MPH-LA 60 mg, and 46 patients to MPH-LA 80 mg. Compared with the number of patients in each fixed-dose arm of the 9-week dose confirmation phase, a shift in the dose needed for optimization was observed for two-thirds of the patients in each of the three arms of 40, 60, and 80 mg/day (Table 2).
As analyzed by Cochran-Mantel-Haenszel test in a post hoc manner (P = 0.2477), there was no relationship between the dose levels in the dose confirmation phase and in the open-label dose optimization phase. Thus, we do not find any signal indicating that the protocol-driven pre-treatment dose had any influence on the clinically driven dose in the open-label dose optimization phase.
3.2 Safety Assessments
The mean duration of exposure to study drug during the open-label dose optimization phase was 34.4 ± 6.01 days. No deaths related to study drug occurred during the course of this phase (or the entire course of the study). Overall, incidence of AEs during this study phase was 65.2 %. The most common AEs observed included headache, decreased appetite, and dry mouth (Table 3). The percentage of AEs leading to discontinuation in the open-label dose optimization phase (3.8 %) was less than the percentage of AEs that led to discontinuation in the dose confirmation phase (11.3 %). The most common AE leading to discontinuation was anxiety (n = 4; 0.7 %).
The incidence of AEs possibly related to rebound symptoms (anxiety, depression, irritability, nervous activity, agitation, fatigue, excessive sleeping, increased appetite, and psychosis) was low and similar for MPH-LA- and placebo-treated patients during Weeks 1 and 2 of the dose optimization phase (Table 4).
No clinically meaningful differences were observed with respect to laboratory findings, vital signs, or electrocardiograms. The percentage of patients with clinically notable QT and Bazett’s-corrected QT (QTcB) intervals (≥30 ms) was 5.2 and 13.2 %, respectively, in the MPH-LA-treated group. None of the patients had a QT, QTcB, or Fridericia-corrected QT (QTcF) interval ≥500 ms during this study phase (Table 5).
3.3 Efficacy Assessments
At the end of the 5-week open-label dose optimization phase, improvement from baseline (of the dose confirmation phase) was seen in all scales (14 weeks of treatment in total). The mean improvement from baseline in DSM-IV ADHD RS total score and SDS total score were 23.5 ± 9.90 and 9.7 ± 7.36, respectively. The improvement in the DSM-IV ADHD RS score and the SDS total score during the open-label dose optimization phase, as analyzed by the treatment received in the dose confirmation phase, is shown in Figs. 3 and 4, respectively. The improvement was similar across all treatment groups allocated in the dose confirmation phase.
Improvement in DSM-IV ADHD RS total score from baseline during the open-label dose optimization phase by treatment group in the dose confirmation phase. 1LOCF using the final visit for each patient with data in the open-label dose optimization phase. 2The optimal dose by Week 14 is as shown in Table 2; P values refer to the two-sided P value based on the difference between the MPH-LA group and placebo. DSM-IV ADHD RS Diagnostic and Statistical Manual of Mental Disorders, fourth edition, Attention Deficit Hyperactive Disorder Rating Scale, LOCF last observation carried forward, LS least squares, MPH-LA methylphenidate modified release long acting,
Improvement in SDS total score from baseline during the open-label dose optimization phase by treatment group in the dose confirmation phase. 1LOCF using the final visit for each patient with data in the open-label dose optimization phase. 2The optimal dose by Week 14 is as shown in Table 2; P values refer to the two-sided P value based on the difference between the MPH-LA group and placebo. LOCF last observation carried forward, MPH-LA methylphenidate modified release long acting, SDS Sheehan Disability Scale
The proportion of patients rated 1 or 2 (very much improved or much improved) on the CGI-I scale was 81 % at the end of the dose optimization phase (Week 14 of the study) for all MPH-LA patients. The proportion of patients with improvement on the CGI-S scale at the end of the dose optimization phase was 91.7 % for all MPH-LA patients. Analysis by the treatment received in the dose confirmation phase for the CGI-I scale and CGI-S scales are shown in Figs. 5 and 6, respectively. As observed for DSM-IV ADHD RS and SDS, improvement as measured by CGI-I or CGI-S was similar across all treatment groups as allocated in the dose confirmation phase.
Proportion of patients with improvement on the CGI-I scale (much improved or very much improved) in the open-label dose optimization phase by treatment group in the dose confirmation phase (LOCF). 1LOCF using the final visit for each patient with data in the open-label dose optimization phase. 2The optimal dose by Week 14 is as shown in Table 2; P values refer to the two-sided P value based on the difference between MPH-LA group and placebo. CGI-I Clinical Global Impression–Improvement Scale, LOCF last observation carried forward, MPH-LA methylphenidate modified release long acting
Proportion of patients with improvement on the CGI-S scale in the open-label dose optimization phase by treatment group in the dose confirmation phase (LOCF). 1LOCF using the final visit for each patient with data in the open-label dose optimization phase. Improvement was defined as a decrease on the CGI-S scale. 2The optimal dose by Week 14 is as shown in Table 2; P values refer to the two-sided P value based on the difference between the MPH-LA group and placebo. CGI-S Clinical Global Improvement–Severity Scale, LOCF last observation carried forward, MPH-LA methylphenidate modified release long acting
The patients who received placebo in the dose confirmation phase, when optimized to their individual dose of MPH-LA 40–80 mg/day in the open-label dose optimization phase, showed similar responses in both symptom and functional scales as compared with patients who received MPH-LA in the dose confirmation phase (Figs. 3, 4, 5, and 6).
4 Discussion
The present study confirmed that MPH-LA in the dose range of 40–80 mg/day was well-tolerated and was necessary to optimally treat adult ADHD patients. Furthermore, our data indicates that short-term pre-treatment with a certain dose of MPH-LA does not predict the dose level in an open-label optimization setting. By the end of the open-label dose optimization phase, which allowed titration to each patient’s individual optimal dose, of the total 489 patients (83.7 %) who completed this phase (and entered the maintenance of effect phase), the number of patients who reached an optimal dose of 40, 60, or 80 mg/day was similar. This indicates that all three dose levels of MPH-LA are necessary in a real-life clinical setting, so as to optimally treat adult patients with ADHD. It is also of interest to note that in each of the randomized patients receiving MPH-LA 40, 60, or 80 mg/day in the 9-week dose confirmation phase, only one-third of patients in each group required the same dose at the end of the 5-week dose optimization phase. The remainder of the patients needed either a higher or lower optimal dose.
These data also indicate that MPH-LA will allow flexible dosing to individualize the dose based on patient need. Our study findings are comparable with those reported by Adler et al. using a flexible dose range of osmotic-release oral system (OROS) methylphenidate (36–108 mg/day), wherein adult ADHD patients initiating therapy at 36 mg/day with weekly increments of 18 mg/day showed good safety and tolerability outcomes [8, 9]. In their study, the protocol was designed to reach the minimal effective dose rather than optimizing the dose. In the current study, as opposed to the Adler et al. study, MPH-LA was titrated to an optimal dose balancing efficacy with safety.
The overall incidence of AEs observed in the open-label dose optimization phase in the current study was 65.2 % and the most common AEs reported were headache, decreased appetite, dry mouth, nasopharyngitis, nausea, and insomnia. Use of immediate-release formulations of stimulants including methylphenidate are associated with rebound symptoms upon wearing off [10, 11]. In our study, the formulation used was a long-acting modified-release capsule designed to deliver a bimodal release of the drug to mimic a twice a day dosing regimen. Sudden reduction in the dose of MPH-LA from 40, 60, or 80 mg to 20 mg was not associated with rebound symptoms. The safety and tolerability observed in this study are similar to those reported in children and are consistent with the known effects of methylphenidate or other stimulant medications [12, 13].
Although the current phase of the study was not designed to evaluate efficacy of MPH-LA, patients continued to show improvement in ADHD symptom control and reduction in functional impairment as measured by DSM-IV ADHD RS and SDS. Furthermore, in both the clinician-rated scales, CGI-I and CGI-S, a higher proportion of patients showed improvement than in observations during the dose confirmation phase. These results are consistent with other short-term dose optimization studies evaluating efficacy of methylphenidate in adults with ADHD [2, 9, 14, 15]. The present study is of particular interest as improved symptomatic effects were observed upon dose optimization, and clinical optimization of dosing did not depend on the prior fixed MPH-LA dose in the initial phase.
4.1 Limitations
A limitation was that the open-label dose optimization phase of the study was not designed to evaluate the efficacy of the optimal dose of MPH-LA. The protocol using increments of 20 mg/day to achieve optimal dose of 40, 60, or 80 mg/day by Week 13 or 14 (Week 4 and 5 of the open-label dose optimization phase) required maintenance of the optimal dose in an individual patient only for 1 week prior to Week 14. Thus, it was unable to measure the efficacy parameters by optimal dose obtained at the end of this phase, and data shown are by treatment received in the dose confirmation phase.
4.2 Research in Context
Although studies in a pediatric population report consistent response rates of 70–80 % (if swapping non-responders to another stimulant, the response rate was increased up to 90 %), there is considerable variation in response rates to methylphenidate in adults [4, 16]. Thus, many guidelines recommend the ‘start low and go slow’ approach (e.g., NICE guidelines; European Consensus) or individually adjusted optimization based on response and tolerability. In the present study, we used the same strategy of optimal dosing in individual patients to identify the safe dose that was effective.
5 Conclusions
In clinical practice, dose individualization with methylphenidate is necessary to achieve the optimal balance of efficacy and safety. The present study confirms that a dose range of 40–80 mg/day of MPH-LA was necessary to effectively individualize/optimize patient treatment for adult ADHD by achieving appropriate symptom control and reduction in functional impairment. All the three MPH-LA doses (40, 60, and 80 mg) were well-tolerated by adult ADHD patients in this study.
References
National Institute of Clinical Excellence (NICE). Attention deficit hyperactivity disorder: diagnosis and management of ADHD in children, young people and adults. NICE. 2008. http://publications.nice.org.uk/attention-deficit-hyperactivity-disorder-cg72.
Medori R, Ramos-Quiroga JA, Casas M, et al. A randomized, placebo-controlled trial of three fixed dosages of prolonged-release OROS methylphenidate in adults with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2008;63:981–9.
Spencer TJ, Adler LA, McGough JJ, et al. Efficacy and safety of dexmethylphenidate extended-release capsules in adults with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2007;61:1380–7.
Wilens TE, Morrison NR, Prince J. An update on the pharmacotherapy of attention-deficit/hyperactivity disorder in adults. Expert Rev Neurother. 2011;11:1443–65.
Vitiello B, Severe JB, Greenhill LL, et al. Methylphenidate dosage for children with ADHD over time under controlled conditions: lessons from the MTA. J Am Acad Child Adolesc Psychiatry. 2001;40:188–96.
Kooij SJ, Bejerot S, Blackwell A, et al. European consensus statement on diagnosis and treatment of adult ADHD: The European Network Adult ADHD. BMC Psychiatry. 2010;10:67.
Huss M, Ginsberg Y, Tvedten T, Arngrim T, Philipsen A, Carter K, et al. Methylphenidate hydrochloride modified-release in adults with attention deficit hyperactivity disorder: a randomized double-blind placebo-controlled trial. Adv Ther. 2014;31(1):44–65.
Adler LA, Orman C, Starr HL, et al. Long-term safety of OROS methylphenidate in adults with attention-deficit/hyperactivity disorder: an open-label, dose-titration, 1-year study. J Clin Psychopharmacol. 2011;31:108–14.
Adler LA, Zimmerman B, Starr HL, et al. Efficacy and safety of OROS methylphenidate in adults with attention-deficit/hyperactivity disorder: a randomized, placebo-controlled, double-blind, parallel group, dose-escalation study. J Clin Psychopharmacol. 2009;29:239–47.
Kooij JJ, Burger H, Boonstra AM, et al. Efficacy and safety of methylphenidate in 45 adults with attention-deficit/hyperactivity disorder. A randomized placebo-controlled double-blind cross-over trial. Psychol Med. 2004;34:973–82.
Garland EJ. Pharmacotherapy of adolescent attention deficit hyperactivity disorder: challenges, choices and caveats. J Psychopharmacol. 1998;12:385–95.
Schulz E, Fleischhaker C, Hennighausen K, et al. A double-blind, randomized, placebo/active controlled crossover evaluation of the efficacy and safety of Ritalin (R) LA in children with attention-deficit/hyperactivity disorder in a laboratory classroom setting. J Child Adolesc Psychopharmacol. 2010;20:377–85.
Adler LA, Spencer T, McGough JJ, et al. Long-term effectiveness and safety of dexmethylphenidate extended-release capsules in adult ADHD. J Atten Disord. 2009;12:449–59.
Biederman J, Mick E, Surman C, et al. A randomized, placebo-controlled trial of OROS methylphenidate in adults with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2006;59:829–35.
Rosler M, Fischer R, Ammer R, et al. A randomised, placebo-controlled, 24-week, study of low-dose extended-release methylphenidate in adults with attention-deficit/hyperactivity disorder. Eur Arch Psychiatry Clin Neurosci. 2009;259:120–9.
Wilens TE, Spencer TJ. The stimulants revisited. Child Adolesc Psychiatr Clin N Am. 2000;9:573–603, viii.
Acknowledgments
This study was sponsored by Novartis Pharma AG. The authors thank the patients for their participation and contribution to this study, as well as the investigators and the entire study team. Michael Huss was responsible for the study design, provided medical advice on the data interpretation, and guided the writer during the development of the draft manuscript. Ylva Ginsberg, Torben Arngrim, and Alexandra Philipsen contributed to data collection and data interpretation. Katherine Carter was the trial head employed by Novartis Pharmaceutical Corporation and was accountable for the delivery of the trial, study design, data collection, data analysis, and data interpretation. Chien-Wei Chen contributed to statistical methods of the study protocol and data analysis and interpretation. Preetam Gandhi contributed to study conduct, data analyses and interpretation, and provided direction during development of the manuscript. Vinod Kumar contributed to the design of the study, helped conduct the study, and contributed to data analysis and data interpretation.
The authors would like to thank Sai Krishnaveni Chevooru, PhD of Novartis Healthcare Pvt. Ltd. for developing the first draft of the manuscript that was prepared under the guidance of the lead author. All authors edited the manuscript for intellectual content and approved the final version submitted for publication. The authors also acknowledge the contributions of Praveen Duhan, MD and Kanaka Sridharan, MS, R.Ph. for providing valuable feedback and review during the development of the manuscript. Michael Huss is the guarantor for this article and takes responsibility for the integrity of the work as a whole.
Conflict of interest
Michael Huss has served as an advisory board member for Eli Lilly, Engelhardt Arzneimittel, Janssen-Cilag, Medice, Novartis, Shire, and Steiner Arzneimittel, and as a consultant for Engelhardt Arzneimittel, Medice, and Steiner Arzneimittel. He has received honoraria from Eli Lilly, Engelhardt Arzneimittel, Janssen-Cilag, Medice, Novartis, and Shire. He has received unrestricted grants for investigator-initiated trials from Eli Lilly, Medice, Engelhardt Arzneimittel, and Steiner Arzneimittel. Ylva Ginsberg has served as a consultant and speaker for Janssen-Cilag and Novartis and as a speaker for Lundbeck, Eli Lilly, and HB Pharma. She has also been a principal investigator of two international multicenter trials initiated by Janssen-Cilag, and she was the coordinating investigator of a methylphenidate trial conducted in adult prison inmates with ADHD, funded by the Swedish Ministry of Health and Social Affairs. Torben Arngrim has been involved in clinical trials conducted by Janssen-Cilag and Novartis. He has received speaker fees from Janssen-Cilag, Novartis, Eli Lilly, and HB Pharma, and has served as an advisory board member for Novartis and Shire. Alexandra Philipsen has received speaker fees and/or travel grants from Eli Lilly, Janssen-Cilag, Medice, Novartis, and Shire, and has been involved in clinical trials conducted by Eli Lilly, Janssen-Cilag, Medice, and Novartis. She has served as an advisory board member for Eli Lilly, Janssen-Cilag, Medice, Novartis, and Shire. She is the coordinating investigator of a multicenter trial on the treatment of adult ADHD (Current Controlled Trials ISRCTN54096201, funded by the Federal Ministry of Education and Research 01GV0606). Katherine Carter, Chien-Wei Chen, Preetam Gandhi, and Vinod Kumar are employees of Novartis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Huss, M., Ginsberg, Y., Arngrim, T. et al. Open-Label Dose Optimization of Methylphenidate Modified Release Long Acting (MPH-LA): A Post Hoc Analysis of Real-Life Titration from a 40-Week Randomized Trial. Clin Drug Investig 34, 639–649 (2014). https://doi.org/10.1007/s40261-014-0213-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-014-0213-2