Abstract
Aims
Diabetes can be an important cofactor in the development of penile inflammation. Here, we explored the association between penile inflammatory disorders and diabetes mellitus (DM), hypertension, and hyperlipidemia in the Taiwanese population, using a population-based data set.
Methods
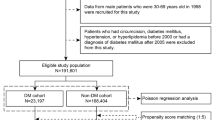
The research data in this study were obtained from Taiwan’s National Health Insurance Research Database between January 1997 and December 2010. We identified 12,819 patients who had a diagnosis of DM, and randomly matched 38,457 subjects as controls. The data were analyzed with Poisson regression analysis and with Cox regression with a frailty model after propensity score matching.
Results
DM (odd ratio (OR) = 1.43, p < 0.01), and age (OR = 0.71, p < 0.01), but not hyperlipidemia (OR = 0.96, p =0.36), or hypertension (OR = 1.09, p = 0.10) had an impact on the development of penile inflammatory disorders. DM was a risk factor associated with penile inflammatory disorder (HR = 1.42, 95% CI = 1.27~1.68, p < 0.01), whereas no statistical difference was noted between penile inflammation and hypertension (HR = 0.98, 95% CI = 0.89~1.09) and hyperlipidemia (HR = 1.03, 95% CI = 0.92~1.14).
Conclusions
T2DM and younger age, but not hypertension or hyperlipidemia, were associated with an increased risk of penile inflammatory disorders in men between 30 and 49 years of age. Our findings suggest the need for preemptive circumcision for selective men with diabetes may prevent diabetes-associated penile inflammatory disorders.


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to the license with Bureau of National Health Insurance, Taiwan (BNHI) and National Health Research Institutes, Taiwan, the administrators of National Health Insurance Research Database (NHIRD).
Abbreviations
- BXO:
-
balanitis xerotica obliterans
- CI:
-
confidence interval
- DM:
-
diabetes mellitus
- ED:
-
erectile dysfunction
- HR:
-
Hazard Ratio
- NHIRD:
-
National Health Insurance Research Database
- OR:
-
Odds RatioT2DM: type 2 diabetes mellitus.
References
Chen L, Magliano DJ, Zimmet PZ. The worldwide epidemiology of type 2 diabetes mellitus—present and future perspectives. Nat Rev Endocrinol. 2012;8:228–36. https://doi.org/10.1038/nrendo.2011.183.
Kautzky-Willer A, Harreiter J, Pacini G. Sex and gender differences in risk, pathophysiology and complications of type 2 diabetes mellitus. Endocr Rev. 2016;37(3):278–316. https://doi.org/10.1210/er.2015-1137.
Deshpande AD, Harris-Hayes M, Schootman M. Epidemiology of diabetes and diabetes-related complications. Phys Ther. 2008;88:1254–64. https://doi.org/10.2522/ptj.20080020.
Yoshimura N, Chancellor MB, Andersson KE, Christ GJ. Recent advances in understanding the biology of diabetes-associated bladder complications and novel therapy. BJU Int. 2005;95(6):733–8. https://doi.org/10.1111/j.1464-410X.2005.05392.x.
Gandhi J, Dagur G, Warren K, Smith NL, Khan SA. Genitourinary complications of diabetes mellitus: an overview of pathogenesis, evaluation, and management. Curr Diabetes Rev. 2017;13(5):498–518. https://doi.org/10.2174/1573399812666161019162747.
Fakjian N, Hunter S, Cole GW, et al. An argument for circumcision: prevention of Balanitis in the adult. Arch Dermatol. 1990;126:1046–7. https://doi.org/10.1001/archderm.1990.01670320070011.
Huang YC, Huang YK, Chen CS, Shindel AW, Wu CF, Lin JH, Chiu KH, Yang TH, Shi CS. Phimosis with preputial fissures as a predictor of undiagnosed type 2 diabetes in adults. Acta Derm Venereol. 2016;96:377–80. https://doi.org/10.2340/00015555-2244.
Drivsholm T, Olivarius NDF, Nielsen ABS, et al. Symptoms, signs and complications in newly diagnosed type 2 diabetic patients, and their relationship to glycaemia, blood pressure and weight. Diabetologia. 2005;48:210–4. https://doi.org/10.1007/s00125-004-1625-y.
Grandy S, Fox KM, Hardy E. Prevalence and recurrence of urinary tract and genital infections among adults with and without type 2 diabetes mellitus in the general population: a longitudinal cohort study. J Diabetes Res Clin Metab. 2013;2:8. https://doi.org/10.7243/2050-0866-2-5.
Hirji I, Andersson SW, Guo Z, Hammar N, Gomez-Caminero A. Incidence of genital infection among patients with type 2 diabetes in the UK General Practice Research Database. J Diabetes Complications. 2012;26:501–5. https://doi.org/10.1016/j.jdiacomp.2012.06.012.
National Health Insurance Research Database, Taiwan. http://nhird.nhri.org.tw/en/index.htm. Accessed 30 Nov 2020.
Therneau TM, Lumley T, Elizabeth A. The survival package. (2021). http://brieger.esalq.usp.br/CRAN/web/packages/survival/survival.pdf.
Ho DE, Imai K, King G, Stuart EA. Matching as nonparametric preprocessing for reducing model dependence in parametric causal Inference. Polit Anal. 2007;15:199–236. https://doi.org/10.1093/pan/mpl013.
Ho DE, Imai K, King G, et al. MatchIt: Nonparametric preprocessing for parametric causal inference. J Stat Softw. 2011;42(28). https://doi.org/10.18637/jss.v042.i08.
Depasquale I, Park AJ, Bracka A. The treatment of balanitis xerotica obliterans. BJU Int. 2000;86:459–65. https://doi.org/10.1046/j.1464-410x.2000.00772.x.
Ke CC, Chen CH, Chen JJ, et al. Balanoposthitis with a volcano-like appearance may be the first clinical presentation of undiagnosed diabetes mellitus. Incont Pelvic Floor Dysfunct. 2011;5:120-121. 10.6259%2fIPFD.2011.5.4.120.
Tandogdu Z, Cai T, Koves B, Wagenlehner F, Bjerklund-Johansen TE. Urinary tract infections in immunocompromised patients with diabetes, chronic kidney disease, and kidney transplant. Eur Urol Focus. 2016;2:394–9. https://doi.org/10.1016/j.euf.2016.08.006.
Hussain LA, Lehner T. Comparative investigation of Langerhans' cells and potential receptors for HIV in oral, genitourinary and rectal epithelia. Immunology. 1995;85:475–84 https://www.ncbi.nlm.nih.gov/pubmed/7558138.
Lisboa C, Ferreira A, Resende C, Rodrigues AG. Infectious balanoposthitis: management, clinical and laboratory features. Int J Dermatol. 2009;48:121–4. https://doi.org/10.1111/j.1365-4632.2009.03966.x.
Isomaa BO, Almgren P, Tuomi T, Forsén B̈, Lahti K, Nissén M, Taskinen MR, Groop L. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001;24:683–9. https://doi.org/10.2337/diacare.24.4.683.
Shariq OA., Hanson KT, McKenna, et al. Does metabolic syndrome increase the risk of postoperative complications in patients undergoing colorectal cancer surgery?. Dis Colon Rectum. 2019;62:849-858. https://journals.lww.com/dcrjournal/toc/2019/07000.
De Haas EC., Oosting SF, Lefrandt JD, et al The metabolic syndrome in cancer survivors. Lancet Oncol. 2010;11:193-203. 10.1016/S1470-2045(09)70287-6.
Lien CS, Lee SW, Chang CH, Chung CJ, Lin CL, Huang CP. Adult balanoposthitis patients have a higher risk of Type 2 diabetes mellitus: A nationwide population-based cohort study. Urol Sci. 2018;29:55–60. https://doi.org/10.1016/j.urols.2017.07.002.
Wang CC, Chancellor MB, Lin JM, Hsieh JH, Yu HJ. Type 2 diabetes but not metabolic syndrome is associated with an increased risk of lower urinary tract symptoms and erectile dysfunction in men aged< 45 years. BJU Int. 2010;105:1136–40. https://doi.org/10.1111/j.1464-410X.2009.08913.x.
La Vignera S, Condorelli RA, Cannarella R, et al. Urogenital infections in patients with diabetes mellitus: Beyond the conventional aspects. Int J Immunopathol Pharmacol. 2019;33:2058738419866582. https://doi.org/10.1177/2058738419866582.
Medina M, Castillo-Pino E. An introduction to the epidemiology and burden of urinary tract infections. Ther Adv Urol. 2019;11:1756287219832172. https://doi.org/10.1177/1756287219832172.
Acknowledgments
The authors thank En Chu Kong Hospital and Asia Eastern University of Science and Technology, for their assistance with this research project.
Author information
Authors and Affiliations
Contributions
CCW designed the study and wrote the study protocol. CCW, IW, and YHL were involved in the conception, design, analysis, and interpretation of the data, as well as the drafting and revision of the paper. All authors have approved the final version for publication and accept responsibility for all aspects of the work. CCW is the guarantor of this work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, CC., Wang, I. & Lai, YH. Type 2 diabetes mellitus increases the risk of penile inflammatory disorders in men aged between 30 and 49: a 5-year follow-up study. Int J Diabetes Dev Ctries 43, 267–273 (2023). https://doi.org/10.1007/s13410-022-01081-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-022-01081-4