Abstract
While proton beam therapy (PBT) can offer increased sparing of healthy tissue, it is associated with large capital costs and as such, has limited availability. Furthermore, it has not been well established whether PBT has significant clinical advantages over conventional volumetric modulated arc therapy (VMAT) for all tumour types. PBT can potentially offer improved clinical outcomes for base of skull chordoma (BOSCh) patients compared with photon (X-ray) therapy, however the cost-effectiveness of these treatments is unclear. In this study, the cost-effectiveness of PBT in the treatment of BOSCh patients is assessed, based on an analysis of comparative radiotherapy treatment plans using a radiobiological Markov model. Seven BOSCh patients had treatment plans for the delivery of intensity modulated proton therapy and VMAT retrospectively analysed. The patient outcome (in terms of tumour local control and normal tissue complications) after receiving each treatment was estimated with a radiobiological Markov model. In addition, the model estimated the cost of both the primary treatment and treating any resultant adverse events. The incremental cost-effectiveness ratio (ICER) was obtained for each patient. PBT was found to be cost-effective for 5 patients and cost-saving for 2. The mean ICER was AUD$1,990 per quality adjusted life year gained. Variation of model parameters resulted in the proton treatments remaining cost-effective for these patients. Based on this cohort, PBT is a cost-effective treatment for patients with BOSCh. This supports the inclusion of PBT for BOSCh in the Medicare Services Advisory Committee 1455 application.

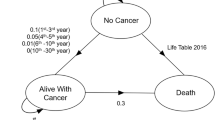
Adapted from Austin et al. [8]
Similar content being viewed by others
References
Tasman Radiation Oncology Group (TROG) (2012) The assessment of new radiation oncology technologies and treatments (ANROTAT) project final report. TROG, Newcastle
Fletcher CD, Unni KK, Mertens F (2002) Pathology and genetics of tumours of soft tissue and bone. IARC, Lyon
Amichetti M, Cianchetti M, Amelio D, Enrici RM, Minniti G (2009) Proton therapy in chordoma of the base of the skull: a systematic review. Neurosurg Rev 32:403
Mailhot Vega R, Kim J, Hollander A et al (2015) Cost effectiveness of proton versus photon radiation therapy with respect to the risk of growth hormone deficiency in children. Cancer 121:1694–1702
Peeters A, Grutters JP, Pijls-Johannesma M et al (2010) How costly is particle therapy? Cost analysis of external beam radiotherapy with carbon-ions, protons and photons. Radiother Oncol 95:45–53
Jäkel O, Land B, Combs SE, Schulz-Ertner D, Debus J (2007) On the cost-effectiveness of carbon ion radiation therapy for skull base chordoma. Radiother Oncol 83:133–138
Lundkvist J, Ekman M, Ericsson SR, Jönsson B, Glimelius B (2005) Cost-effectiveness of proton radiation in the treatment of childhood medulloblastoma. Cancer 103:793–801
Austin AM, Douglass MJ, Nguyen GT, Penfold SN (2017) A radiobiological Markov simulation tool for aiding decision making in proton therapy referral. Physica Med 44:72–82
Fagundes MA, Hug EB, Liebsch NJ, Daly W, Efird J, Munzenrider JE (1995) Radiation therapy for chordomas of the base of skull and cervical spine: patterns of failure and outcome after relapse. Int J Radiat Oncol Biol Phys 33:579–584
ABS (2016) Life tables, states, territories and Australia, 2013-2015. ABS, Canberra
Schneider U, Sumila M, Robotka J (2011) Site-specific dose-response relationships for cancer induction from the combined Japanese A-bomb and Hodgkin cohorts for doses relevant to radiotherapy. Theor Biol Med Model 8:27
AIHW (2017) Cancer in Australia. Cancer series no. 101. AIHW, Canberra
Lee TF, Yeh SA, Chao PJ et al (2015) Normal tissue complication probability modeling for cochlea constraints to avoid causing tinnitus after head-and-neck intensity-modulated radiation therapy. Radiat Oncol 10:194
De Marzi L, Feuvret L, Boulé T et al (2015) Use of gEUD for predicting ear and pituitary gland damage following proton and photon radiation therapy. Br J Radiol 88:20140413
Ramaekers BL, Joore MA, Grutters JP et al (2011) The impact of late treatment-toxicity on generic health-related quality of life in head and neck cancer patients after radiotherapy. Oral Oncol 47:768–774
Tengs TO, Wallace A (2000) One thousand health-related quality-of-life estimates. Med Care 38:583–637
Refaie AE, Davis A, Kayan A, Baskill J, Lovell E, Owen V (2004) A questionnaire study of the quality of life and quality of family life of individuals complaining of tinnitus pre-and postattendance at a tinnitus clinic. Int J Audiol 43:410–416
Busschbach J, Wolffenbuttel B, Annemans L, Meerding W, Kołtowska-Häggström M (2011) Deriving reference values and utilities for the QoL-AGHDA in adult GHD. Eur J Health Econ 12:243–252
Kemp R, Ramiscal R, Fodero L, Reardon O, Lyon S, Scuteri J (2017) Assesment of proton beam therapy (unpublished): Commonwealth of Australia. ACT, Canberra
Bates N, Callander E, Lindsay D, Watt K (2018) Labour force participation and the cost of lost productivity due to cancer in Australia. BMC Public Health 18:375
Bennett G, Dealey C, Posnett J (2004) The cost of pressure ulcers in the UK. Age Ageing 33:230–235
Maes IH, Cima RF, Vlaeyen JW, Anteunis LJ, Joore MA (2013) Tinnitus: a cost study. Ear Hear 34:508–514
Taylor H, Pezzullo M, Keeffe J (2006) The economic impact and cost of visual impairment in Australia. Br J Ophthalmol 90:272–275
Bonomi A, Palmer C, Ajax M, Peeples P, Jackson S (1999) Cost of managing mucositis and xerostomia in head and neck cancer patinets undergoing chemoradiothearpy or radiation. Value Health 2:197
Medicare Benefits Scheme Item number 42702. http://www9.health.gov.au/mbs/fullDisplay.cfm?type=item&q=42702&qt=item. Accessed 14 Feb 2019
NICE (2012) Methods for the development of NICE public health guidance—incorporating health economics, 3rd edn. https://www.nice.org.uk/process/pmg4/chapter/incorporating-health-economics. Accessed 14 Dec 2019
Lievens Y, Pijls-Johannesma M (2013) Health economic controversy and cost-effectiveness of proton therapy. Semin Radiat Oncol 23:134–141
Langendijk JA, Lambin P, De Ruysscher D, Widder J, Bos M, Verheij M (2013) Selection of patients for radiotherapy with protons aiming at reduction of side effects: the model-based approach. Radiother Oncol 107:267–273
Chung CS, Yock TI, Nelson K, Xu Y, Keating NL, Tarbell NJ (2013) Incidence of second malignancies among patients treated with proton versus photon radiation. Int J Radiat Oncol Biol Phys 87:46–52
Acknowledgements
The authors wish to thank Peter Rhodes for the early development of the project. The first author acknowledges the support of an Australian Government Research Training Program Scholarship. The third author acknowledges the support of ACEMS (ARC Centre of Excellence for Mathematical and Statistical Frontiers).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Scott Penfold has worked part-time for a developer of a proton therapy centre. The other authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Royal Adelaide Hospital Research Ethics Committee No. 150322) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Austin, A.M., Douglass, M.J.J., Nguyen, G.T. et al. Cost-effectiveness of proton therapy in treating base of skull chordoma. Australas Phys Eng Sci Med 42, 1091–1098 (2019). https://doi.org/10.1007/s13246-019-00810-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13246-019-00810-0