Abstract
Purpose
It has been reported clinically that rupture or dissections in thoracic aortic aneurysms (TAA) often occur due to hypertension which may be modelled with sudden increase of peripheral resistance, inducing acute changes of blood volumes in the aorta. There is clinical evidence that more compliant aneurysms are less prone to rupture as they can sustain such changes of volume. The aim of the current paper is to verify this paradigm by evaluating computationally the role played by the variation of peripheral resistance and the impact of aortic stiffness onto peak wall stress in ascending TAA.
Methods
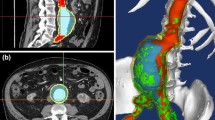
Fluid–structure interaction (FSI) analyses were performed using patient-specific geometries and boundary conditions derived from 4D MRI datasets acquired on a patient. Blood was assumed incompressible and was treated as a non-Newtonian fluid using the Carreau model while the wall mechanical properties were obtained from the bulge inflation tests carried out in vitro after surgical repair. The Navier–Stokes equations were solved in ANSYS Fluent. The Arbitrary Lagrangian–Eulerian formulation was used to account for the wall deformations. At the interface between the solid domain and the fluid domain, the fluid pressure was transferred to the wall and the displacement of the wall was transferred to the fluid. The two systems were connected by the System Coupling component which controls the solver execution of fluid and solid simulations in ANSYS. Fluid and solid domains were solved sequentially starting from the fluid simulations.
Results
Distributions of blood flow, wall shear stress and wall stress were evaluated in the ascending thoracic aorta using the FSI analyses. We always observed a significant flow eccentricity in the simulations, in very good agreement with velocity profiles measured using 4D MRI. The results also showed significant increase of peak wall stress due to the increase of peripheral resistance and aortic stiffness. In the worst case scenario, the largest peripheral resistance (1010 kg s m−4) and stiffness (10 MPa) resulted in a maximal principal stress equal to 702 kPa, whereas it was only 77 kPa in normal conditions.
Conclusions
This is the first time that the risk of rupture of an aTAA is quantified in case of the combined effects of hypertension and aortic stiffness increase. Our findings suggest that a stiffer TAA may have the most altered distribution of wall stress and an acute change of peripheral vascular resistance could significantly increase the risk of rupture for a stiffer aneurysm.







Similar content being viewed by others
References
Alford, P. W., and L. A. Taber. Computational study of growth and remodelling in the aortic arch. Comput. Methods Biomech. Biomed. Eng. 11(5):525–538, 2008. https://doi.org/10.1080/10255840801930710.
ANSYS® Academic Research, Release 17.2, Help System, Overview of Flow Solvers Theory Guide, ANSYS, Inc.
Azadani, A. N., S. Chitsaz, A. Mannion, A. Mookhoek, A. Wisneski, J. M. Guccione, et al. Biomechanical properties of human ascending thoracic aortic aneurysms. Ann. Thorac. Surg. 96(1):50–58, 2013. https://doi.org/10.1016/j.athoracsur.2013.03.094.
Burk, J., P. Blanke, Z. Stankovic, A. Barker, M. Russe, J. Geiger, et al. Evaluation of 3D blood flow patterns and wall shear stress in the normal and dilated thoracic aorta using flow-sensitive 4D CMR. J. Cardiovasc. Magn. Reson. 14:84, 2012. https://doi.org/10.1186/1532-429X-14-84.
Callaghan, F. M., J. Karkouri, K. Broadhouse, M. Evin, D. F. Fletcher, and S. M. Grieve. Thoracic aortic aneurysm: 4D flow MRI and computational fluid dynamics model. Comput. Methods Biomech. Biomed. Eng. 18(Suppl 1):1894–1895, 2015. https://doi.org/10.1080/10255842.2015.1069559.
Chau, K. H., and J. A. Elefteriades. Natural history of thoracic aortic aneurysms: size matters, plus moving beyond size. Prog. Cardiovasc. Dis. 56(1):74–80, 2013. https://doi.org/10.1016/j.pcad.2013.05.007.
Cheng, Z., E. Kidher, O. A. Jarral, D. P. O’Regan, N. B. Wood, T. Athanasiou, et al. Assessment of hemodynamic conditions in the aorta following root replacement with composite valve-conduit graft. Ann. Biomed. Eng. 44(5):1392–1404, 2016. https://doi.org/10.1007/s10439-015-1453-x.
Childs, H., L. Ma, M. Ma, J. Clarke, M. Cocker, J. Green, et al. Comparison of long and short axis quantification of left ventricular volume parameters by cardiovascular magnetic resonance, with ex vivo validation. J. Cardiovasc. Magn. Reson. 13:40, 2011. https://doi.org/10.1186/1532-429X-13-40.
Choudhury, N., O. Bouchot, L. Rouleau, D. Tremblay, R. Cartier, J. Butany, et al. Local mechanical and structural properties of healthy and diseased human ascending aorta tissue. Cardiovasc. Pathol. 18(2):83–91, 2009. https://doi.org/10.1016/j.carpath.2008.01.001.
Condemi, F., S. Campisi, M. Viallon, T. Troalen, G. Xuexin, A. J. Barker, et al. Fluid- and Biomechanical Analysis of Ascending Thoracic Aorta Aneurysm with Concomitant Aortic Insufficiency. Ann. Biomed. Eng. 45(12):2921–2932, 2017. https://doi.org/10.1007/s10439-017-1913-6.
Crosetto, P., P. Reymond, S. Deparis, D. Kontaxakis, N. Stergiopulos, and A. Quarteroni. Fluid–structure interaction simulation of aortic blood flow. Comput. Fluids 43(1):46–57, 2011. https://doi.org/10.1016/j.compfluid.2010.11.032.
Davis, F. M., Y. Luo, S. Avril, A. Duprey, and J. Lu. Local mechanical properties of human ascending thoracic aneurysms. J. Mech. Behav. Biomed. Mater. 61:235–249, 2016. https://doi.org/10.1016/j.jmbbm.2016.03.025.
Duprey, A., O. Trabelsi, M. Vola, J. P. Favre, and S. Avril. Biaxial rupture properties of ascending thoracic aortic aneurysms. Acta Biomater. 42:273–285, 2016. https://doi.org/10.1016/j.actbio.2016.06.028.
Gallo, D., G. De Santis, F. Negri, D. Tresoldi, R. Ponzini, D. Massai, et al. On the use of in vivo measured flow rates as boundary conditions for image-based hemodynamic models of the human aorta: implications for indicators of abnormal flow. Ann. Biomed. Eng. 40(3):729–741, 2012. https://doi.org/10.1007/s10439-011-0431-1.
Garcia-Herrera, C. M., J. M. Atienza, F. J. Rojo, E. Claes, G. V. Guinea, D. J. Celentano, et al. Mechanical behaviour and rupture of normal and pathological human ascending aortic wall. Med. Biol. Eng. Comput. 50(6):559–566, 2012. https://doi.org/10.1007/s11517-012-0876-x.
Hatzaras, I., M. Tranquilli, M. Coady, P. M. Barrett, J. Bible, and J. A. Elefteriades. Weight lifting and aortic dissection: more evidence for a connection. Cardiology 107(2):103–106, 2007. https://doi.org/10.1159/000094530.
Hornick, M., R. Moomiaie, H. Mojibian, B. Ziganshin, Z. Almuwaqqat, E. S. Lee, et al. ‘Bovine’ aortic arch—a marker for thoracic aortic disease. Cardiology 123(2):116–124, 2012. https://doi.org/10.1159/000342071.
Howard, D. P., A. Banerjee, J. F. Fairhead, J. Perkins, L. E. Silver, P. M. Rothwell, et al. Population-based study of incidence and outcome of acute aortic dissection and premorbid risk factor control: 10-year results from the Oxford Vascular Study. Circulation 127(20):2031–2037, 2013. https://doi.org/10.1161/CIRCULATIONAHA.112.000483.
Humphrey, J. D., M. A. Schwartz, G. Tellides, and D. M. Milewicz. Role of mechanotransduction in vascular biology: focus on thoracic aortic aneurysms and dissections. Circ. Res. 116(8):1448–1461, 2015. https://doi.org/10.1161/CIRCRESAHA.114.304936.
Iliopoulos, D. C., R. P. Deveja, E. P. Kritharis, D. Perrea, G. D. Sionis, K. Toutouzas, et al. Regional and directional variations in the mechanical properties of ascending thoracic aortic aneurysms. Med. Eng. Phys. 31(1):1–9, 2009. https://doi.org/10.1016/j.medengphy.2008.03.002.
Iliopoulos, D. C., E. P. Kritharis, A. T. Giagini, S. A. Papadodima, and D. P. Sokolis. Ascending thoracic aortic aneurysms are associated with compositional remodeling and vessel stiffening but not weakening in age-matched subjects. J. Thorac. Cardiovasc. Surg. 137(1):101–109, 2009. https://doi.org/10.1016/j.jtcvs.2008.07.023.
Isselbacher, E. M. Thoracic and abdominal aortic aneurysms. Circulation 111(6):816–828, 2005. https://doi.org/10.1161/01.CIR.0000154569.08857.7A.
Joldes, G. R., K. Miller, A. Wittek, and B. Doyle. A simple, effective and clinically applicable method to compute abdominal aortic aneurysm wall stress. J. Mech. Behav. Biomed. Mater. 58:139–148, 2016. https://doi.org/10.1016/j.jmbbm.2015.07.029.
Jondeau, G., and C. Boileau. Genetics of thoracic aortic aneurysms. Curr. Atheroscler. Rep. 14(3):219–226, 2012. https://doi.org/10.1007/s11883-012-0241-4.
Khanafer, K., and R. Berguer. Fluid–structure interaction analysis of turbulent pulsatile flow within a layered aortic wall as related to aortic dissection. J. Biomech. 42(16):2642–2648, 2009. https://doi.org/10.1016/j.jbiomech.2009.08.010.
Khanafer, K., A. Duprey, M. Zainal, M. Schlicht, D. Williams, and R. Berguer. Determination of the elastic modulus of ascending thoracic aortic aneurysm at different ranges of pressure using uniaxial tensile testing. J. Thorac. Cardiovasc. Surg. 142(3):682–686, 2011. https://doi.org/10.1016/j.jtcvs.2010.09.068.
Lantz, J., J. Renner, and M. Karlsson. Wall shear stress in a subject specific human aorta—influence of fluid–structure interction. Int. J. Appl. Mech. 03(04):759–778, 2011. https://doi.org/10.1142/s1758825111001226.
Les, A. S., S. C. Shadden, C. A. Figueroa, J. M. Park, M. M. Tedesco, R. J. Herfkens, et al. Quantification of hemodynamics in abdominal aortic aneurysms during rest and exercise using magnetic resonance imaging and computational fluid dynamics. Ann. Biomed. Eng. 38(4):1288–1313, 2010. https://doi.org/10.1007/s10439-010-9949-x.
Leung, J. H., A. R. Wright, N. Cheshire, J. Crane, S. A. Thom, A. D. Hughes, et al. Fluid structure interaction of patient specific abdominal aortic aneurysms: a comparison with solid stress models. BioMed. Eng. Online 5(1):33, 2006. https://doi.org/10.1186/1475-925X-5-33.
Martin, C., W. Sun, T. Pham, and J. Elefteriades. Predictive biomechanical analysis of ascending aortic aneurysm rupture potential. Acta Biomater. 9(12):9392–9400, 2013. https://doi.org/10.1016/j.actbio.2013.07.044.
Martufi, G., T. C. Gasser, J. J. Appoo, and E. S. Di Martino. Mechano-biology in the thoracic aortic aneurysm: a review and case study. Biomech. Model. Mechanobiol. 13(5):917–928, 2014. https://doi.org/10.1007/s10237-014-0557-9.
Michel, J. B., G. Jondeau, and D. M. Milewicz. From genetics to response to injury: vascular smooth muscle cells in aneurysms and dissections of the ascending aorta. Cardiovasc. Res. 114(4):578–589, 2018. https://doi.org/10.1093/cvr/cvy006.
Morbiducci, U., D. Gallo, D. Massai, F. Consolo, R. Ponzini, L. Antiga, et al. Outflow conditions for image-based hemodynamic models of the carotid bifurcation: implications for indicators of abnormal flow. J. Biomech. Eng. 132(9):091005, 2010. https://doi.org/10.1115/1.4001886.
Mousavi, S. J., and S. Avril. Patient-specific stress analyses in the ascending thoracic aorta using a finite-element implementation of the constrained mixture theory. Biomech. Model. Mechanobiol. 16(5):1765–1777, 2017. https://doi.org/10.1007/s10237-017-0918-2.
Mousavi, S. J., S. Farzaneh, and S. Avril. Computational predictions of damage propagation preceding dissection of ascending thoracic aortic aneurysms. Int. J. Numer. Methods biomed. Eng. 34(4):e2944, 2018. https://doi.org/10.1002/cnm.2944.
Nathan, D. P., C. Xu, J. H. Gorman, 3rd, R. M. Fairman, J. E. Bavaria, R. C. Gorman, et al. Pathogenesis of acute aortic dissection: a finite element stress analysis. Ann. Thorac. Surg. 91(2):458–463, 2011. https://doi.org/10.1016/j.athoracsur.2010.10.042.
Nordon, I., R. Brar, J. Taylor, R. Hinchliffe, I. M. Loftus, and M. M. Thompson. Evidence from cross-sectional imaging indicates abdominal but not thoracic aortic aneurysms are local manifestations of a systemic dilating diathesis. J. Vasc. Surg. 50(1):171e1–176e1, 2009. https://doi.org/10.1016/j.jvs.2009.03.007.
Pasta, S., A. Rinaudo, A. Luca, M. Pilato, C. Scardulla, T. G. Gleason, et al. Difference in hemodynamic and wall stress of ascending thoracic aortic aneurysms with bicuspid and tricuspid aortic valve. J. Biomech. 46(10):1729–1738, 2013. https://doi.org/10.1016/j.jbiomech.2013.03.029.
Phillippi, J. A., S. Pasta, and D. A. Vorp. Biomechanics and Pathobiology of Aortic Aneurysms. Biomechanics and Mechanobiology of Aneurysms. Studies in Mechanobiology: Tissue Engineering and Biomaterials, pp. 67–118, 2011.
Pirola, S., Z. Cheng, O. A. Jarral, D. P. O’Regan, J. R. Pepper, T. Athanasiou, et al. On the choice of outlet boundary conditions for patient-specific analysis of aortic flow using computational fluid dynamics. J. Biomech. 60:15–21, 2017. https://doi.org/10.1016/j.jbiomech.2017.06.005.
Qiao, A.-K., W.-Y. Fu, and Y.-J. Liu. Study on hemodynamics in patient-specific thoracic aortic aneurysm. Theoret. Appl. Mech. Lett. 1(1):014001, 2011. https://doi.org/10.1063/2.1101401.
Ramanath, V. S., J. K. Oh, T. M. Sundt, III, and K. A. Eagle. Acute aortic syndromes and thoracic aortic aneurysm. Mayo Clin. Proc. 84(5):465–481, 2009. https://doi.org/10.1016/S0025-6196(11)60566-1.
Redheuil, A., W. C. Yu, E. Mousseaux, A. A. Harouni, N. Kachenoura, C. O. Wu, et al. Age-related changes in aortic arch geometry: relationship with proximal aortic function and left ventricular mass and remodeling. J. Am. Coll. Cardiol. 58(12):1262–1270, 2011. https://doi.org/10.1016/j.jacc.2011.06.012.
Robertson, A. M., A. Sequeira, and R. G. Owens. Rheological models for blood. In: Cardiovascular Mathematics: Modeling and Simulation of the Circulatory System, edited by L. Formaggia, A. Quarteroni, and A. Veneziani. Milano: Springer Milan, 2009, pp. 211–241.
Romo, A., P. Badel, A. Duprey, J. P. Favre, and S. Avril. In vitro analysis of localized aneurysm rupture. J. Biomech. 47(3):607–616, 2014. https://doi.org/10.1016/j.jbiomech.2013.12.012.
Shang, E. K., D. P. Nathan, S. R. Sprinkle, R. M. Fairman, J. E. Bavaria, R. C. Gorman, et al. Impact of wall thickness and saccular geometry on the computational wall stress of descending thoracic aortic aneurysms. Circulation 128(11 Suppl 1):S157–S162, 2013. https://doi.org/10.1161/CIRCULATIONAHA.112.000200.
Sigovan, M., M. D. Hope, P. Dyverfeldt, and D. Saloner. Comparison of four-dimensional flow parameters for quantification of flow eccentricity in the ascending aorta. J. Magn. Reson. Imaging 34(5):1226–1230, 2011. https://doi.org/10.1002/jmri.22800.
Strecker, C., A. Harloff, W. Wallis, and M. Markl. Flow-sensitive 4D MRI of the thoracic aorta: comparison of image quality, quantitative flow, and wall parameters at 1.5 T and 3 T. J Magn Reson Imaging. J. Magn. Reson. Imaging 36(5):1097–1103, 2012. https://doi.org/10.1002/jmri.23735.
Tezduyar, T. E., S. Sathe, T. Cragin, B. Nanna, B. S. Conklin, J. Pausewang, et al. Modelling of fluid–structure interactions with the space–time finite elements: arterial fluid mechanics. Int. J. Numer. Methods 54(6–8):901–922, 2007. https://doi.org/10.1002/fld.1443.
Trabelsi, O., F. M. Davis, J. F. Rodriguez-Matas, A. Duprey, and S. Avril. Patient specific stress and rupture analysis of ascending thoracic aneurysms. J. Biomech. 48(10):1836–1843, 2015. https://doi.org/10.1016/j.jbiomech.2015.04.035.
Trabelsi, O., A. Duprey, J. P. Favre, and S. Avril. Predictive models with patient specific material properties for the biomechanical behavior of ascending thoracic aneurysms. Ann. Biomed. Eng. 44(1):84–98, 2016. https://doi.org/10.1007/s10439-015-1374-8.
Tromp, G., H. Kuivaniemi, I. Hinterseher, and D. J. Carey. Novel genetic mechanisms for aortic aneurysms. Curr. Atheroscler. Rep. 12(4):259–266, 2010. https://doi.org/10.1007/s11883-010-0111-x.
Tse, K. M., P. Chiu, H. P. Lee, and P. Ho. Investigation of hemodynamics in the development of dissecting aneurysm within patient-specific dissecting aneurismal aortas using computational fluid dynamics (CFD) simulations. J. Biomech. 44(5):827–836, 2011. https://doi.org/10.1016/j.jbiomech.2010.12.014.
Valen-Sendstad, K., and D. A. Steinman. Mind the gap: impact of computational fluid dynamics solution strategy on prediction of intracranial aneurysm hemodynamics and rupture status indicators. AJNR Am. J. Neuroradiol. 35(3):536–543, 2014. https://doi.org/10.3174/ajnr.A3793.
Vikrant, S., and S. C. Tiwari. Essential hypertension—pathogenesis and pathophysiology. J. Indian Acad. Clin. Med. 2:140–161, 2001.
Vorp, D. A. Biomechanics of abdominal aortic aneurysm. J. Biomech. 40(9):1887–1902, 2007. https://doi.org/10.1016/j.jbiomech.2006.09.003.
Vorp, D. A., B. J. Schiro, M. P. Ehrlich, T. S. Juvonen, M. A. Ergin, and B. P. Griffith. Effect of aneurysm on the tensile strength and biomechanical behavior of the ascending thoracic aorta. Ann. Thorac. Surg. 75(4):1210–1214, 2003.
Wagenseil, J. E. Bio-chemo-mechanics of thoracic aortic aneurysms. Curr. Opin. Biomed. Eng. 5:50–57, 2018. https://doi.org/10.1016/j.cobme.2018.01.002.
Wilson, K. A., A. J. Lee, A. J. Lee, P. R. Hoskins, F. G. Fowkes, C. V. Ruckley, et al. The relationship between aortic wall distensibility and rupture of infrarenal abdominal aortic aneurysm. J. Vasc. Surg. 37(1):112–117, 2003. https://doi.org/10.1067/mva.2003.40.
Acknowledgments
We thank Dr Morbiducci and Dr Gallo from Polytechnic of Turin (Italy) who provided insight and expertise that greatly assisted the model development. We are also grateful to Ansys, Inc. for providing Ansys-Fluent (ANSYS® Academic Research, Release 17.2). This research was supported by the European Research Council (ERC grant biolochanics, grant number 647067).
Funding
This research was supported by the European Research Council (ERC grant biolochanics, grant number 647067, grant holder: SA).
Conflict of interest
All the authors declare they have no conflict of interest.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments. The study was approved by the Institutional Review Board of the University Hospital Center of Saint-Étienne (France). After informed consent, a 59-year-old man was enrolled. The patient was scanned on a 3T MRI scanner (Siemens Magnetom Prisma) without contrast agent using a 4D flow phase contrast protocol and sequence.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editors Dr. David A. Steinman, Dr. Francesco Migliavacca, and Dr. Ajit P. Yoganathan oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Campobasso, R., Condemi, F., Viallon, M. et al. Evaluation of Peak Wall Stress in an Ascending Thoracic Aortic Aneurysm Using FSI Simulations: Effects of Aortic Stiffness and Peripheral Resistance. Cardiovasc Eng Tech 9, 707–722 (2018). https://doi.org/10.1007/s13239-018-00385-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-018-00385-z