Abstract
Currently colorectal cancer (CRC) is the third most prevalent cancer worldwide. Body mass index (BMI) is frequently used in CRC screening and risk assessment to quantitatively evaluate weight. However, the impact of BMI on clinical strategies for CRC has received little attention. Within the framework of the predictive, preventive, and personalized medicine (3PM/PPPM), we hypothesized that BMI stratification would affect the primary, secondary, and tertiary care options for CRC and we conducted a critical evidence-based review. BMI dynamically influences CRC outcomes, which helps avoiding adverse treatment effects. The outcome of surgical and radiation treatment is adversely affected by overweight (BMI ≥ 30) or underweight (BMI < 20). A number of interventions, such as enhanced recovery after surgery and robotic surgery, can be applied to CRC at all levels of BMI. BMI-controlling modalities such as exercise, diet control, nutritional therapy, and medications may be potentially beneficial for patients with CRC. Patients with overweight are advised to lose weight through diet, medication, and physical activity while patients suffering of underweight require more focus on nutrition. BMI assists patients with CRC in better managing their weight, which decreases the incidence of adverse prognostic events during treatment. BMI is accessible, noninvasive, and highly predictive of clinical outcomes in CRC. The cost–benefit of the PPPM paradigm in developing countries can be advanced, and the clinical benefit for patients can be improved with the promotion of BMI-based clinical strategy models for CRC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Objectives for the review
The significance of body mass index (BMI) in colorectal cancer (CRC) preventative screening has been well established in previous studies that focused on the effects of overweight (high BMI) and the screening and assessment of CRC risk using BMI [1,2,3]. Mainstream therapies such as radical surgery [4] and neoadjuvant chemotherapy [5] have been demonstrated to correlate with BMI. BMI may predict the outcome of treatment for CRC. However, a comprehensive review of these studies was not available to a personalized BMI-based clinical strategy for CRC. This paper discusses the role of BMI in the clinical management of CRC from the perspective of clinical treatment and weight management, thus promoting clinical strategies for CRC in the predictive, preventive, and personalized medicine (3PM/PPPM) paradigm.
State of the art
CRC, BMI, and PPPM
CRC is the third most diagnosed cancer worldwide and the second leading cause of cancer-related mortality [6]. Overweight is a high-risk factor for CRC and a major cause of death [7, 8]. The pathogenesis is mostly influenced by visceral abdominal fat and insulin storage [9]. As a simple means to quantify obesity by calculating height and weight, BMI is frequently used to screen for CRC morbidity and mortality [10]. It can be easily calculated by dividing the weight (kg) by the square of height (m). The application of BMI neither includes medical testing procedures, breaches patient privacy, nor endangers the patient’s body in any way. To meet the need for more multidimensional healthcare, the PPPM paradigm is widely used in the diagnosis and treatment of cancer [11, 12]. Under standardized medicine, BMI is often used only as a general stratification factor. PPPM considers BMI as an important node in multiple predictors, incorporating it into a wide range of diseases and health models, including cancer prediction [13].
BMI in CRC primary care: a proven marker
Obesity is a well-recognized risk factor for CRC, which has been confirmed by multiple epidemiological evidence [14]. Most studies suggest that obesity (high BMI) has a role in the emergence of CRC [15]. Morbidly obese individuals (BMI ≥ 30 kg/m2) have a higher risk of developing CRC (risk ratio [RR] = 1.93; 95% confidence interval [CI], 1.15–3.25)[6].Males may be more at risk than females [16], although maternal obesity (BMI ≥ 30 kg/m2) also increases the risk of CRC diagnosis in offspring (adjusted hazard ratio [aHR] = 2.51; 95% CI, 1.05–6.02) [17]. Insulin resistance, hyperinsulinemia, elevated leptin levels, and the development of an inflammatory microenvironment can promote the growth and proliferation of colon cancer cells [9, 10, 18]. Therefore, obesity-associated CRC is considered a subtype of CRC. The addition of BMI as a proven marker in CRC screening programs worldwide has been scientifically recommended [19]. Longitudinal studies have established screening methods that combine BMI with exposure time [20], implying that weight control may be effective in CRC prevention. The focus of this paper is put on how BMI can be introduced into secondary and tertiary care for CRC, a more developmental topic compared to primary care. Bariatric surgery, dietary modification, calorie restriction, and other types of weight control have the potential to reduce the risk of CRC. This will be reviewed in detail in the following section.
BMI in CRC secondary and tertiary care: ready for action
Individuals diagnosed with CRC are often offered standardized treatment based on guidelines aimed at preventing metastases, complications, and death, i.e., secondary and tertiary care for CRC. The PPPM paradigm seeks a higher quality of care, using more systems medicine, anthropometric, and even multicultural tools to define patients more precisely, with BMI being an important and fundamental factor. Excessive high or low BMI poses a significant impact on the prognosis and survival of patients with CRC receiving clinical treatment. High BMI is a determinant in the progression of CRC [21], while a low BMI is associated with an increased risk of death, a poorer prognosis, and malnutrition in patients with CRC [22, 23]. Notably, patients suffering from CRC with low or consistently declining BMI may be more susceptible to side effects or even death due to nutritional deficiencies or muscle loss [24, 25]. Weight management after diagnosis also affects treatment outcomes. Currently, the mainstream therapies for treating CRC include laparoscopy treatment, surgery, adjuvant chemotherapy, systemic therapy, and radiotherapy [26,27,28]. In the following paragraphs, we will discuss treatment modalities and weight management to investigate the impact of BMI on CRC receiving appropriate treatment.
BMI-based predictions in surgical treatment of CRC
Surgical treatment—open surgery and laproscopy
Open surgery and laparoscopic surgery are the two main categories for the surgical treatment of CRC. Usually, laparoscopic surgery is used to treat locally advanced, non-metastasis colon cancer that is resectable. Since the 1990s, it has been widely used due to its exceptional safety and efficacy [29]. For patients with stage II/III colon cancer, laparoscopic surgery is a reasonable selection, while patients with BMI ≥ 30 kg/m2 may need to carefully consider the surgical procedure [30]. As BMI increases, patients are more likely to switch from laparoscopic surgery to open surgery, with a subsequent increase in the incidence of surgical complications [31]. Patients with obesity have higher technical requirements for laparoscopic surgery than those without obesity [32]. Due to the thickening of the mesentery, laparoscopic surgery may result in vessel dissection and difficulty in ligation. Obesity also contributes to postoperative infections, which cause postoperative wound complications due to inadequate concentration of antibiotics in the tissues [33]. A pooled analysis of comparative studies also suggested that patients of CRC with a high BMI (≥ 30 kg/m2) may have poor perioperative outcomes, such as longer operative times and greater blood loss [34]. However, there is no difference in oncological outcomes between open surgery and laparoscopic surgery [35, 36]. Patients with obesity and high BMI need to carefully select for open surgical treatment options and laparoscopic surgery treatment. Furthermore, their postoperative recovery should be closely observed to take active care of the surgical wound, thus minimizing the adverse effects of postoperative complications.
Surgical treatment—emergency open surgery
Emergency open surgery is routinely performed in patients with surgical emergencies such as intestinal obstruction or perforation in CRC [37]. Since the obstruction of CRC often emerges in a more advanced stage of liver metastasis, and perforation usually develops in near tumors [38], the implementation of emergency surgery is inherently risky. Surgery-related stoma problems are common in patients with CRC with left-sided intestinal obstruction and high BMI (BMI ≥ 30.0 kg/m2), which is not conducive to prognostic care [39]. This result demonstrates that patients with CRC need more attention to their prognosis and better postoperative management after emergency surgery.
Surgical treatment—colostomy
Colostomy can also be employed in treating left-sided obstructive colon cancer, whereas patients with high BMI are at increased risk of parastomal hernias and early skin irritation [40]. If this treatment is chosen, special attention should be paid to post-operative recovery and prognosis for patients with high BMI.
Surgical treatment—robotic-assisted surgery
Robotic-assisted surgery is often used as a minimally invasive procedure for cases of colon cancer requiring total mesenteric resection. This kind of surgery is safer than traditional open surgery and as effective as laparoscopic surgery [41]. It is equally applicable to patients with BMI in various classification [42]. However, patients need to know that robotic surgery is more costly and requires a longer time to perform [43].
Surgical treatment—enhanced recovery after surgery
Enhanced recovery after surgery (ERAS) is a comprehensive intervention program in the perioperative period that reduces the stress of surgery and promotes rapid recovery through multidisciplinary collaboration between surgeons, anesthetists, and surgical nurses [44]. There is multiple evidence to support that ERAS can reduce the length of stay, reduce healthcare costs, and improve the quality of recovery in patients undergoing CRC surgery [45, 46]. There have been studies comparing the outcomes of laparoscopic CRC surgery with ERAS in patients with various BMI classifications and types of obesity. However, no significant differences between obesity subgroups demonstrated the generalizability of ERAS for CRC surgery [47].
Low BMI as a risk factor in the surgical treatment of CRC
In contrast, patients with CRC and excessively low BMI are more likely to die after surgical treatment due to impaired nutrition and immune deficiency [4]. Patients with low BMI (15–19.99 kg/m2) also have worse long-term survival than those with a normal BMI [48]. Therefore, nutritional support can be considered to improve immunity before surgical treatment, and the rehabilitation of the patient should be closely monitored after surgery.
Hepatic surgery for metastatic CRC
Hepatectomy is the most effective treatment option to cure or prolong the life of patients with CRC liver metastases. Patients with a BMI ≥ 28 kg/m2 are more likely to develop steatohepatitis because of steatosis [49]. Minimally invasive liver surgery is a preferable alternative for individuals with obesity and a higher BMI due to its increased safety and effectiveness compared to standard open resection or laparoscopic resection [50]. Skeletal muscle loss (SMI) can be used to predict complications because BMI does not accurately predict surgical complications following hepatectomy [51].
Cytoreductive surgery with hyperthermic intraoperative intraperitoneal chemotherapy
CRC is usually followed by peritoneal metastases and progresses to peritoneal carcinoma in certain cases [52]. Tumor cell reduction combined with intraoperative heat-infused intraperitoneal chemotherapy (CRS + HIPEC) is currently an efficient treatment for this disease. CRS is a surgical procedure that employs argon knife cautery to remove visible tumors from the abdominal cavity as completely as possible. HIPEC is a regional treatment of abdominal tumors combining abdominal heat and chemotherapy, which has enhanced pharmacokinetic advantages over conventional systemic therapy. In this treatment, an infusion heated to a certain temperature is mixed with chemotherapeutic agents and instilled into the abdominal cavity. There was no significant difference in the efficacy of this treatment between patients with high BMI and those with BMI, suggesting that it is suitable for both types of patients [53].
BMI-based predictions in adjuvant chemotherapy of CRC
High BMI in adjuvant chemotherapy of CRC
Adjuvant chemotherapy is frequently recommended for the recovery treatment of CRC up to 3 months following surgery. Fluorouracil-based single-agent regimens, such as oral capecitabine and folinic acid-modulated 5-fluorouracil regimen (5-FU), are among the clinically applicable adjuvant chemotherapy regimens and are among the clinically applicable adjuvant chemotherapy regimens. Oxaliplatin plus capecitabine (CapeOx regimen), oxaliplatin plus 5-FU plus leucovorin (mFOLFOX6) regimen, and 5-fluorouracil and levamisole (5FU-LEV) regimen are a few examples of different combination chemotherapy regimens. Adverse prognosis events after adjuvant chemotherapy, such as relapse and death, are more likely to occur in patients with high BMI (≥ 30 kg/m2) [54, 55]. More specifically, patients with a higher BMI may be more susceptible to the adverse effects of adjuvant chemotherapy, such as nausea, vomiting, and peripheral neuropathy [56], while taking 5-FU-based chemotherapy for metastatic CRC (mCRC). Male patients with extreme obesity had a 16% higher mortality rate than patients of normal weight, and they may have a worse prognosis than female patients, in particular, due to increased buildup of abdominal or central fat [57]. Those with a BMI > 35.0 kg/m2 demonstrated a considerably increased risk of CRC recurrence and even mortality following combination chemotherapy with 5-FU, 5-FU plus leucovorin/levamisole regimens [58]. Patients with a greater BMI who received the drugs 5-FU and oxaliplatin had a higher rate of cessation, depression symptoms, and less social support [59]. A higher BMI was linked to peripheral neuropathy in patients with CRC receiving the oxaliplatin regimen combined with chemotherapy [60].
Low BMI in adjuvant chemotherapy of CRC
A relapse following adjuvant chemotherapy is more common in patients with abnormally low BMI (< 20 kg/m2). Furthermore, compared to patients with normal BMI, they have a considerably shorter disease-free survival rate [57]. Acute pancreatitis is a rare consequence of CRC that can also occur in underweight patients [61]. Therefore, adjuvant chemotherapy regimens should be carefully planned for patients with abnormally high or low BMI. The adjuvant chemotherapy prognosis and side effects should also be carefully considered.
Systematic therapy and bevacizumab for metastatic CRC
The standard treatment for initially unresectable liver is mCRC hepatectomy. However, more patients are choosing systemic therapy instead [62]. The commonly used systemic regimens in clinical practice include mFOLFOX6 plus bevacizumab/cetuximab, CapeOx plus bevacizumab, FOLFIRI (5-fluorouracil, leucovorin, and irinotecan), and FOLFOXIRI (folinic acid, 5-fluorouracil, oxaliplatin and irinotecan). A previous study showed that mCRC patients with high BMI were more likely to develop steatosis and liver injury after liver resection following systemic therapy (including 5-FU, oxaliplatin, irinotecan, and the FOLFOXIRI regimen) [63]. Additionally, patients with mCRC may experience a decrease in BMI after systemic therapy, accompanied by the development of ongoing decreased SMI. The decrease may be caused by the cachexia of the advanced disease, and it cannot demonstrate that the decrease in BMI is beneficial to the prognosis of mCRC [64,65,66]. Patients with obesity should have their BMI constantly monitored, and a drop in BMI should be considered a predictor of disease regression.
Bevacizumab is the primarily targeted therapy for mCRC that inhibits tumor angiogenesis by blocking the EGFR/VEGF receptor pathway. Compared with patients with normal BMI, patients with BMI ≥ 25 kg/m2 may have a shorter tumor progression time because visceral fat can induce the accumulation of tumor factors [67]. Among patients receiving chemotherapy and bevacizumab-targeted therapy, those with excessively low or high BMI had a significantly shorter overall survival than normal individuals [68]. However, some research has concluded that BMI is not a predictor of prognosis for the addition of targeted therapy to chemotherapy [69]. More evidence needs to be analyzed to determine the relationship between CRC-targeted therapy and BMI.
Treatment for rectal cancer
Surgery, adjuvant chemotherapy, systemic therapy, and simultaneous radiotherapy are all used to treat rectal cancer. Similar to colon cancer, a higher BMI increases the risk of rectal cancer surgery and the operation difficulty [70, 71]. Moreover, continuous growth in BMI is associated with higher rates of post-operative complications and longer post-operative hospital stays [72, 73]. Patients with excessively low BMI (< 18.5 kg/m2) have a poorer early and long-term prognosis after rectal cancer surgery [74], leading to a higher risk of acute organ toxicity and even death [25].
Abdominoperineal resection
Abdominoperineal resection is a specific surgical treatment for rectal cancer, especially for patients with obesity and a high BMI. Male patients with obesity and rectal cancer are more likely than normal-weight male and female patients to experience a local recurrence. They might be unable to retain their sphincter due to pelvic stenosis and increasing obesity [75]. Furthermore, the overall survival rate of patients with obesity who undergo this procedure is lower [76]. Based on these results, the postoperative rehabilitation and prognosis of male patients with high BMI need to be closely observed.
Simultaneous radiotherapy
Simultaneous radiotherapy is the standard treatment for inoperable locally advanced rectal cancer. Commonly used treatment regimens are radiotherapy plus capecitabine or radiotherapy plus continuous infusion of 5-FU. Male patients with obesity and high BMI have more adipose tissue in the prostate-rectum junction, and the dose of radiotherapy to the rectal wall is compromised. Therefore, individualized radiotherapy protocols may be more suitable for these patients, such as increasing radiotherapy dose or intensifying systemic therapy [25].
However, extra attention is needed if a consistent trend of decreasing BMI is observed. The toxicity of radiotherapy may affect treatment efficacy and cause diarrhea, renal insufficiency, and radiation proctitis, leading to malnutrition in patients with a BMI loss ≥ 7% [22]. Compared to normal patients, patients with rectal cancer who has an excessively low BMI have a significantly lower overall survival rate [77, 78]. Apart from BMI changes, these patients may receive individualized dietary advice and manual nutritional support to evaluate spontaneous food intake, toxicity tolerance, and nutritional status [79]. The impact of BMI on other treatment options, such as systemic therapy and adjuvant chemotherapy, can be reviewed in the previous section on colon cancer.
BMI management strategy of CRC: comprehensive long-term efforts
According to Hu et al. [23], patients with CRC should avoid excessive weight loss and weight gain. Excessively high or low BMI seriously impacts the outcome and prognosis of CRC. Therefore, a fat reduction strategy should be formulated for patients with CRC and excessively high BMI ( ≥ 35 kg/m2) [80]. For patients with excessively low BMI (< 18.5 kg/m2), supplemental nutritional intake can be considered to increase their body weight [79], thus increasing their BMI to a more reasonable value. This part will focus on patients with CRC and excessively high or low BMI. Based on previous findings, a detailed discussion is provided to ameliorate BMI in patients with CRC by combining the current popular weight management methods (e.g., bariatric surgery, diet control, physical activity, and obesity pharmacotherapies).
BMI management approaches for CRC with excessively high BMI
Non-pharmacological therapy—bariatric surgery
As a long-term weight loss solution, bariatric surgery (BRS) can help with many obesity-related comorbidities. The common procedures are gastric bypass, gastric banding, or sleeve gastrectomy [81]. The role of BRS for CRC is focused on primary care. Practitioners aim to reduce the risk of various diseases, including CRC, by performing BRS on overweight individuals (mainly those with a BMI ≥ 35kg/m2). However, there are conflicting findings as to whether BRS reduces the risk of CRC. High-level evidence suggests that patients with obesity undergoing BRS had over 30% lower risk of colorectal cancer compared to patients with obesity not receiving BRS [82, 83]. BRS has a long-term and durable protective effect on CRC patients with high BMI. It can effectively prevent the development of CRC lesions and reduce postoperative complications through weight loss, facilitating the postoperative prognosis [84, 85]. Other studies have shown that BRS not only fails to reduce [86] but increases the short-term risk of CRC in populations under 50 years of age [87], particularly in the case of gastric bypass surgery [81]. This may be attributed to the inflammatory environment following BRS stimulating hyperproliferation of the intestinal mucosa. The treatment guidelines for CRC should be followed to improve the screening for various risk factors, such as age, sex, tumor stage, and the presence of metastases obstruction symptoms [88]. Based on current findings, BRS is an approach to prevent overweight-related diseases, but the impact on CRC risk remains inconclusive. For the time being, there is no evidence of benefit from BRS after CRC diagnosis. BRS is not recommended temporarily in the CRC population due to concerns about the effect on digestive tract function itself.
Non-pharmacological therapy—diet control
Overweight and obesity result from an imbalance between energy intake and expenditure. A case–control study also demonstrated that patients with CRC have a significantly higher total calorie intake than the normal population, leading to a high BMI in these patients [89]. Patients with CRC and higher BMI tend to favor an unbalanced diet of high fat and lack of fruits, vegetables, and dietary fiber. This unhealthy diet affects the visceral adipose tissue (VAT) profile and leads to altered metabolic pathways, promoting the development of CRC pathologies [90, 91]. Additionally, refined grains, alcohol, processed meats, and red meats are detrimental to the prognosis of patients with CRC [92]. Therefore, patients with high BMI require comprehensive dietary modification. A single-arm exploratory study conducted a diet-mediated weight loss intervention in 20 adults with high BMI. The results revealed that weight loss achieved through a low-energy dietary replacement diet could effectively reduce tumor-related markers in colon tissue and serum [93]. Dietary fibers can be supplemented by eating fruits and vegetables (e.g., onions, apples, berries, cucumbers, sweet potatoes, tomatoes, and peppers); carbohydrate can be supplemented with unrefined grains and legumes; milk and dairy products can provide vitamin B12, lectins, and calcium; and protein can be obtained from poultry, fish, and other low-fat meats [88, 89]. The lectins provided by legumes may have an adjuvant effect on CRC [94].
Non-pharmacological therapy—chronic caloric restriction
Chronic caloric restriction (CR) has been the major dietary intervention to reduce weight and prevent cancer. As an alternative to CR, intermittent fasting (IF) has become a major research focus in recent years, which is more frequently used in basic research such as animal studies [95,96,97]. Nevertheless, the use of IF in the clinical treatment of CRC is poorly studied. No data are available on the positive impact of IF without weight loss and the impact of changes in diet quality and physical activity patterns on the prognostic outcome of CRC [98]. It has been suggested that prolonged perioperative fasting in patients with CRC may lead to longer hospital stays [99]. The above studies suggest that IF can be used as an effective tool for patients with obesity and high BMI to reduce body fat and thus prevent CRC. Currently, IF is not recommended for patients with CRC and higher BMI under treatment. When IF was used before CRC diagnosis, it should not be continued during treatment, except as part of a clinical trial. Physicians should explain the risks and benefits of IF to patients if they wish to receive it during a long-term treatment [98].
Non-pharmacological therapy—physical activity
Current research indicates that a moderate participant in physical activity (PA) has a protective effect on patients with CRC and high BMI and may improve the prognosis of these patients [100]. Regular and moderate physical activity increases basal metabolism and improves tissue oxygenation. As a result, metabolic efficiency and capacity can be facilitated, ultimately reducing the volume of body fat and adipose tissue and mitigating the impact of obesity on patients with CRC [101]. PA reduces circulating insulin and inflammatory markers in CRC [102, 103] thus improving the prognosis of patients. However, some studies have also shown that PA does not ameliorate HRQoL (health-related quality of life) and fatigue after CRC surgery [104]. Short-term (two-week) home-based physical activity after surgery also has no effect on self-assessed physical recovery [105]. Lee et al. [106] noted that a six-week home-based, supervised, and mixed exercise intervention could improve physical activity levels and fitness in survivors of stage II to III CRC. Patients with CRC may suffer from chronic fatigue and cardiac function problems that limit the conduct of PA [107]. Therefore, a more detailed long-term PA schedule should be established to optimize the amount, type, and intensity of exercise. Ultimately, exercise guidelines that better meet the needs of patients can be developed, alleviating the impact of high BMI on the treatment received by patients with CRC.
Pharmacological interventions in BMI management
Based on the nature, action mode, efficacy, and side effects of obesity drugs, they can be classified into short-term and long-term anti-obesity drugs [108]. Short-term anti-obesity drugs include amphetamine, diethylpropion, and benzphetamine; long-term anti-obesity drugs include orlistat, lorcaserin, and liraglutide. Some anti-obesity drugs are addictive and easily abused, with various side effects such as dizziness, heart palpitations, and gastrointestinal adverse reactions. When patients with high BMI take anti-obesity drugs, the associated contraindications need to be confirmed, and the drug dose should be strictly controlled. In addition to these drugs, metformin [109] and berberine [110] can also affect weight reduction and have anti-tumor activity.
Metformin
Metformin is an oral hypoglycemic drug and an adjunct to the treatment of obesity. It lowers blood glucose in patients with obesity by reducing hepatic glucose production and stimulating glucose uptake by peripheral tissues (muscle and fat) [111] and contributes to the weight loss [109, 112]. Current evidence suggests that metformin has an adjuvant effect on the treatment of cancer, particularly CRC. Metformin reduces the risk of CRC [113], reducing serum inflammatory factors[103], and inhibits tumor growth through the AMPK/mTOR pathway, mTOR/AKT pathway, and LKB1/AMPK pathway, thus facilitating the prognosis of patients [114,115,116]. Metformin improves the overall survival of patients with CRC receiving adjuvant chemotherapy and alleviates side effects such as chronic peripheral neuropathy caused by chemotherapy drugs [117,118,119,120]. It also enhances the efficacy of radiotherapy to promote tumor regression in patients with CRC [121]. Recent evidence suggests that metformin may function as a potential radiosensitizer in clinical antitumor therapy. However, its action and molecular mechanisms need to be further investigated.
Currently, only a few studies examined CRC populations with high BMI. Miranda et al. [122] suggested that patients with CRC and a BMI ≥ 30 kg/m2 could significantly benefit from metformin combined with a 5-FU regimen. Refined subgrouping of BMI is still needed to clarify the prognostic impact of metformin on patients with CRC and high BMI. Most of the evidence implies that the overall impact of metformin on patients with CRC and high BMI is positive. It has a multifaceted therapeutic effect through weight loss and adjuvant cancer treatment, which requires to be refined with further clinical evidence.
Berberine
Berberine is a natural isoquinoline alkaloid derived from the genus Berberis [123]. Current evidence suggests that berberine has a weight loss effect on patients with obesity [110]. In addition, it has anti-cancer effects and can target CRC tumors involved in proliferation, invasion, angiogenesis, and metastasis [124, 125]. Chen et al. found that berberine inhibited inflammatory cancer transformation of CRC by modulating mitofusin-2 (MFN2) to reduce colitis exacerbated by obesity [126]. Nevertheless, no relevant clinical studies on CRC populations with high BMI have been conducted. In conclusion, berberine is a promising drug for treating CRC. Further comprehensive investigations are necessary to elucidate the effect of berberine on patients with CRC and high BMI.
BMI management approaches for CRC with excessively low BMI
Special consideration should be taken to patients with CRC and low BMI (< 18.5 kg/m2). An excessively low BMI or a sustained decrease in BMI can negatively affect the survival and prognosis of patients with CRC [57, 68], resulting in the occurrence of weight and nutritional loss, producing cachexia[127].
Oral nutritional supplements
Oral nutritional supplements (ONS) are commonly used in clinical practice to supplement the nutrition not available from the normal diet in patients at risk of malnutrition [128]. Administration of ONS reduces the incidence of skeletal mucle loss and sarcopenia and improves chemotherapy tolerance in patients at nutritional risk (expected reduction in BMI and SMI) after CRC surgery [129]. In addition, supplementation of vitamin D and Omega-3 fatty acids in the daily diet counteract the nutrient deficiencies of patients with low BMI and decrease the inflammatory status after chemotherapy [130].
Other suggestions
In order to closely monitor the nutritional status of these patients, individualized nutritional interventions, nutritional counseling and education, and manual nutritional support such as regular dietary outpatient visits should also be performed which is well in agreement with PPPM strategies and attitude towards better healthcare [131,132,133]. If a persistent decline in BMI is observed, it is necessary to identify other risk factors to determine the cause of the decline in BMI, including the muscle loss or malignancy of the disease [65].
Discussion on reviewed knowledge and data
This paper reviews the impact of BMI on the prognosis of various treatments for CRC, providing a comprehensive summary and evaluation of the current feasible methods for managing BMI in patients with CRC. The impact of different BMI levels on various treatments for CRC has been presented in Table 1 and Table 2. The current evidence indicates that BMI takes an important part in the progression and prognosis of the disease in patients with CRC.
BMI classification standard and ethnicity
According to the BMI classification by the World Health Organization (WHO), patients with underweight have a BMI < 18.5 kg/m2, patients with overweight range from 25.0 to 29.9 kg/m2, patients with obesity range from 30.0 to 35 kg/m2, patients with a BMI ≥ 35 kg/m2 are morbidly obese, and 18.5–24.9 kg/m2 is the most appropriate BMI range [134]. There are national and demographic differences in the BMI classification. Compared to European and American populations, there is a different association between BMI, body fat percentage, and health risks in Asian populations. The normal range of BMI for the Asian population is 18.5–22.9 kg/m2, and more than 25 kg/m2 is considered obese [135]. The ideal BMI range for Chinese people is 18.5–23.9 kg/m2 [136]. Clinicians should develop individualized weight management strategies based on the national and demographic characteristics of patients with CRC, thereby maintaining their BMI at the most reasonable level.
Obesity paradox
Notably, the obesity paradox exists in CRC [15, 23]. The term obesity paradox first appeared in a US study about percutaneous coronary intervention (PCI) [137]. It refers to the trend of a U-shaped relationship between BMI and the corresponding symptoms of patients. Among patients with CRC, those with obesity and high BMI have poorer survival rates. However, for patients with advanced CRC with a risk of malnutrition, maintaining a moderately high BMI (except for patients with morbid obesity and an excessive-high BMI) may be more helpful for their nutritional reserve and survival [23]. Aparicio et al. [138] also showed that patients with mCRC in the BMI range of 28–30 kg/m2 had a better prognosis than normal individuals. A possible explanation is that patients with overweight have greater lean muscle mass than normal one, which helps improve the condition. In summary, the obesity paradox of CRC is more applicable to patients who are overweight and mildly obese. For patients who are morbidly obese, it is still recommended to better manage their BMI in combination with the fat reduction measures [139].
Limitations of BMI and multi-factor assistance
BMI provides limited information and therefore relying on BMI alone is not sufficient. Based on the PPPM paradigm, a combination of factors such as gender, age, and ethnicity will help to better personalize healthcare. Some studies suggested that BMI is unrelated to the prognosis of CRC [140, 141]. The reason might be the delay in adjuvant chemotherapy and the specific combination chemotherapy of FOLFOXIRI plus bevacizumab and FOLFIRI/FOLFOX plus bevacizumab. This conclusion is not suitable for all patients with CRC. For women, abdominal obesity, high BMI at age 18, and subsequent weight gain are associated with a greater risk of CRC. While for men, weight gain in later years and overall obesity are important factors inducing CRC [2, 142]. Higher BMI is more likely to induce colorectal adenomas in black women [143].
Patients with CRC and low BMI (< 25 kg/m2) are susceptible to visceral obesity, which may have a negative impact on prognosis [144]. VAT and body composition on computed tomography (CT) should be combined with waist circumference (WC), waist-to-hip ratio, and other indicators for determining the degree of obesity. With these data, the authentic physical condition of patients can be comprehensively analyzed, allowing for appropriate clinical strategies [10].
An additional guiding direction for multifactorial assistance is to predict changes in BMI through simpler or more prospective representations. Models based on oculomics have been used to predict sarcopenia [145], which gives an idea for cross-sectional prediction. More usable predictive models based on genetic, multi-omic, and anthropometric associations may be formed in the future for PPPM.
Potential BMI-based integrated management approaches
From the evidence discussed above, we believe that BMI-based PPPM practice should be used throughout the full cycle of CRC care, from screening to postoperative recovery and systemic therapy (Fig. 1). It is possible to provide cost–benefit, which has been identified in the context of CRC screening [146]. Due to the limited evidence for the CRC population, practitioners and patients are advised to refer to the experience of BMI management in multi-cancer as well as chronic disease. The environmental applicability of PPPM practices for CRC would be considerably increased. We also consider multicultural factors to develop comprehensive programs to achieve the goal of personalized medicine. In full cycle CRC-BMI management, various types of complementary therapies with low side-effects, such as acupuncture [147, 148], Tai-Chi [149, 150], yoga [151, 152], Chinese herbal medicine [153, 154], and probiotics [155, 156], are recommended depending on the culture as well as the medical setting. Omega-3 fatty acids [157] are well evidenced and have potential to prevent cachexia. The vitamins [158,159,160] might also increase the survival rate. These factors align with PPPM advocacy [161]. The combination of physical activity and personalized nutrition should also receive attention, thus leading to the muscle gain rather than skeletal muscle loss which can be expected if no PA is exerted while. A well-balanced diet is given to patients with CRC [162]. Patients with CRC see a slight increase in BMI a few months following treatment (typically 6–24 months), a sign that tissue and functional status have recovered [163]. However, the recovery is subject to limited conditions, in which the BMI of patients should not be too high and there should be a limited intake of nutrients leading to poor tolerance of the treatment [23, 164]. In order to better determine the prognosis and recovery of patients, the BMI of patients with CRC should be regularly and continuously monitored.
BMI-based integrated management in the context of PPPM. According to the culture and medical level of the patient, the multi-cancer and obesity domains are used as an extension of the evidence to develop a PPPM for patients with CRC based on BMI. Abbreviation: BMI, body mass index; CRC, colorectal cancer; CHM, Chinese herbal medicine; PPPM, predictive, preventive, and personalized medicine
Conclusions and recommendations
BMI employs a straightforward formula that eliminates the need for invasive testing and improves the process of developing treatment strategies for patients with CRC. No biomarker can offer as simple and practical a measurement as BMI. In prior studies, BMI has been demonstrated to be useful in CRC primary care as a predictor consistent with the PPPM paradigm [13]. In this paper, we review the evidence for BMI in CRC secondary and tertiary care. We conclude that BMI can be considered as a full-cycle factor in the practice of PPPM for CRC. We provide Table 3 as a summary of the full text for quick overview and reference. BMI plays a powerful informative role in the development of personalized medicine protocols to the prevention of cancer cachexia. BMI surveillance reveal a poor prognosis and predicts progressive changes, which helps to avoid the risk of different therapies. From the PPPM perspective, BMI helps patients manage their weight and improve prognosis, allowing clinicians to design better personalized clinical strategies. The BMI-based PPPM paradigm is more effective and can be useful in a wide range of developing regions; moreover, it means that more patients can benefit from the PPPM. We recommend for further PPPM development and practical application, to include BMI as a monitoring factor in CRC care in wider range of regions.
The studies on the impact of BMI on different treatments for CRC are not comprehensive, and no studies have investigated the impact of immunotherapies such as Hartmann surgery, stenting, interventional treatments, and CAR-T. Basic research on the impact of BMI and patients with CRC is relatively sparse. Further exploration of the link between BMI and the impact of CRC treatment could also include molecular pathways and the impact of BMI on patients with CRC. In the future clinical practice, we advocate for a more comprehensive study of the interaction between BMI and cancer treatment in order to design better strategies for CRC within the PPPM paradigm.
To summarize our recommendations on the basis of our experience and reviewed knowledge we recommend:
-
Following individual BMI monitoring from the pre-diagnostic period to the treatment period of CRC.
-
Adopt BMI as a prognostic consideration for CRC patients in the absence of other sophisticated screening and modeling tools.
-
For patients with excessively high BMI, evidence-based avoidance of risky treatment options whenever possible and planned weight loss and diet control in conjunction with treatment.
-
For patients with low BMI, a combination of nutritional factors and treatment side effects should be considered.
-
Appropriate physical activity for CRC patients thus helping to improve BMI and other prognostic factors. Exercise approaches should be scientifically tailored and actively recommended when the patient’s physical condition permits.
-
The potential risks and benefits need to be fully explained to patients when BMI-related clinical strategies, such as intermittent fasting and metformin, for which the evidence is not yet sufficient, are used experimentally.
-
Progressive BMI decline after CRC diagnosis may indicate an increased risk. It is necessary to determine the cause in time.
-
BMI-based attitude within PPPM may be cost-effective and efficient, especially in developing regions.
-
More research that is needed to clarify the role of BMI and potentially other indexes and factors in emerging therapies for CRC.
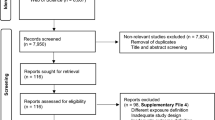
Data availability
The datasets involved in this study were extracted from publicly available papers published in the PubMed database. The datasets may be reused with the author’s permission.
Abbreviations
- 5-FU :
-
5-Fluorouracil
- 5FU-LEV :
-
5-Fluorouracil and levamisole
- AT :
-
Adipose tissue
- BMI :
-
Body mass index
- BRS :
-
Bariatric surgery
- CapeOx :
-
Oxaliplatin plus capecitabine
- CAR-T :
-
Chimeric antigen receptor T-cell immunotherapy
- CI :
-
Confidence interval
- CR :
-
Chronic caloric restriction
- CRA :
-
Colorectal adenoma
- CRC :
-
Colorectal cancer
- CRS + HIPEC :
-
Cytoreductive surgery with hyperthermic intraoperative intraperitoneal chemotherapy
- CT :
-
Computed tomography
- EGFR :
-
Epidermal growth factor receptor
- ERAS :
-
Enhanced recovery after surgery
- FOLFIRI :
-
5-Fluorouracil, leucovorin, and irinotecan
- FOLFOXIRI :
-
Folonic acid, 5-fluorouracil, oxaliplatin, and irinotecan
- HRQoL :
-
Health-related quality of life
- HRs :
-
Hazard ratios
- IF :
-
Intermittent fasting
- IGF :
-
Insulin-like growth factors
- IL :
-
Interleukin
- LSMI :
-
Linear skeletal muscle index
- mCRC :
-
Metastatic colorectal cancer
- MFN2 :
-
Mitofusin-2
- mFOLFOX6 :
-
5-Fluorouracil, leucovorin, and oxaliplatin
- ONS :
-
Oral nutritional supplement
- ORs :
-
Odd ratios
- PA :
-
Physical activity
- PPPM/3PM :
-
Predictive, preventive, and personalized medicine
- SIR :
-
Standardized incidence ratio
- SMI :
-
Skeletal muscle index
- T2D :
-
Type 2 diabetes
- TNF :
-
Tumor necrosis factor
- TZD :
-
Thiazolidinediones
- VAT :
-
Visceral adipose tissue
- VEGF :
-
Vascular endothelial growth factor
- WC :
-
Waist circumference
- WHO :
-
World Health Organization
References
Kantor ED, Udumyan R, Signorello LB, Giovannucci EL, Montgomery S, Fall K. Adolescent body mass index and erythrocyte sedimentation rate in relation to colorectal cancer risk. Gut. 2016;65:1289–95.
Liu P-H, Wu K, Ng K, Zauber AG, Nguyen LH, Song M, et al. Association of obesity with risk of early-onset colorectal cancer among women. JAMA Oncol. 2019;5:37.
Renfro LA, Loupakis F, Adams RA, Seymour MT, Heinemann V, Schmoll H-J, et al. Body mass index is prognostic in metastatic colorectal cancer: pooled analysis of patients from first-line clinical trials in the ARCAD database. J Clin Oncol. 2016;34:144–50.
Hede P, Sörensson MÅ, Polleryd P, Persson K, Hallgren T. Influence of BMI on short-term surgical outcome after colorectal cancer surgery: a study based on the Swedish national quality registry. Int J Colorectal Dis. 2015;30:1201–7.
Cabrera-Mulero A, Crujeiras AB, Izquierdo AG, Torres E, Ayers D, Casanueva FF, et al. Novel SFRP2 DNA methylation profile following neoadjuvant therapy in colorectal cancer patients with different grades of BMI. J Clin Med. 2019;8:1041.
Patel SG, Karlitz JJ, Yen T, Lieu CH, Boland CR. The rising tide of early-onset colorectal cancer: a comprehensive review of epidemiology, clinical features, biology, risk factors, prevention, and early detection. Lancet Gastroenterol Hepatol. 2022;7:262–74.
Bardou M, Barkun AN, Martel M. Obesity and colorectal cancer. Gut. 2013;62:933–47.
Murphy N, Jenab M, Gunter MJ. Adiposity and gastrointestinal cancers: epidemiology, mechanisms and future directions. Nat Rev Gastroenterol Hepatol. 2018;15:659–70.
Frezza EE. Influence of obesity on the risk of developing colon cancer. Gut. 2006;55:285–91.
Tandon K. Body mass index and colon cancer screening: the road ahead. WJG. 2015;21:1371.
Desiderio DM. Cancer diagnostics and treatment: are we ready to implement PPPM? EPMA J. 2010;1:365–7.
Grech G, Zhan X, Yoo BC, Bubnov R, Hagan S, Danesi R, et al. EPMA position paper in cancer: current overview and future perspectives. EPMA J. 2015;6:9.
Golubnitschaja O, Liskova A, Koklesova L, Samec M, Biringer K, Büsselberg D, et al. Caution, “normal” BMI: health risks associated with potentially masked individual underweight—EPMA Position Paper 2021. EPMA J. 2021;12:243–64.
Bardou M, Rouland A, Martel M, Loffroy R, Barkun AN, Chapelle N. Review article: obesity and colorectal cancer. Aliment Pharmacol Ther. 2022;56:407–18.
Li Y, Li C, Wu G, Yang W, Wang X, Duan L, et al. The obesity paradox in patients with colorectal cancer: a systematic review and meta-analysis. Nutr Rev. 2022;80:1755–68.
Seibert RG, Hanchate AD, Berz JP, Schroy PC. National disparities in colorectal cancer screening among obese adults. Am J Prev Med. 2017;53:e41–9.
Murphy CC, Cirillo PM, Krigbaum NY, Singal AG, Lee M, Zaki T, et al. Maternal obesity, pregnancy weight gain, and birth weight and risk of colorectal cancer. Gut. 2022;71:1332–9.
Hardwick J, Vandenbrink G, Vandeventer S, Peppelenbosch M. Leptin is a growth factor for human colon cancer cells. Gastroenterology. 2001;120:A493–A493.
Hultcrantz R. Aspects of colorectal cancer screening, methods, age and gender. J Intern Med. 2021;289:493–507.
Li X, Jansen L, Chang-Claude J, Hoffmeister M, Brenner H. Risk of colorectal cancer associated with lifetime excess weight. JAMA Oncol. 2022;8:730–7.
Loosen SH, Roderburg C, Jördens MS, Fluegen G, Luedde T, Kostev K. Overweight and obesity determine the risk for gastrointestinal cancer in a sex-dependent manner: a retrospective cohort study of 287,357 outpatients in Germany. Cancers. 2022;14:931.
Lin J, Peng J, Qdaisat A, Li L, Chen G, Lu Z, et al. Severe weight loss during preoperative chemoradiotherapy compromises survival outcome for patients with locally advanced rectal cancer. J Cancer Res Clin Oncol. 2016;142:2551–60.
Hu C, Zhang Q, Jin X, Zhang L, Zhang Y, Zhu Q, et al. A paradox between preoperative overweight/obesity and change in weight during postoperative chemotherapy and its relationship to survival in stage II and III colorectal cancer patients. Clin Nutr. 2021;40:2410–9.
Li J-B, Luo S, Wong MCS, Li C, Feng L-F, Peng J-H, et al. Longitudinal associations between BMI change and the risks of colorectal cancer incidence, cancer-relate and all-cause mortality among 81,388 older adults: BMI change and the risks of colorectal cancer incidence and mortality. BMC Cancer. 2019;19:1082.
Diefenhardt M, Ludmir EB, Hofheinz R-D, Ghadimi M, Minsky BD, Fleischmann M, et al. Impact of body-mass index on treatment and outcome in locally advanced rectal cancer: a secondary, post-hoc analysis of the CAO/ARO/AIO-04 randomized phase III trial. Radiother Oncol. 2021;164:223–31.
Chinese Society of Clinical Oncology. Chinese Society of Clinical Oncology (CSCO) Guidelines of Colorectal Cancer 2022. Beijing: People’s Medical Publishing House; 2022.
Costas-Chavarri A, Nandakumar G, Temin S, Lopes G, Cervantes A, Cruz Correa M, et al. Treatment of patients with early-stage colorectal cancer: ASCO resource-stratified guideline. J Glob Oncol. 2019;5:1-19. https://doi.org/10.1200/JGO.18.00214.
National Comprehensive Cancer Network. NCCN clinical practice guidelines in Oncology-colon cancer(2021.Version 2). Fort Washington: National Comprehensive Cancer Network; 2021.
Allardyce RA, Bagshaw PF, Frampton CM, Frizelle FA, Hewett PJ, Rieger NA, et al. Australian and New Zealand study comparing laparoscopic and open surgeries for colon cancer in adults: organization and conduct. ANZ J Surg. 2008;78:840–7.
Bell S, Kong JC, Wale R, Staples M, Oliva K, Wilkins S, et al. The effect of increasing body mass index on laparoscopic surgery for colon and rectal cancer. Colorectal Dis. 2018;20:778–88.
Denost Q, Quintane L, Buscail E, Martenot M, Laurent C, Rullier E. Short- and long-term impact of body mass index on laparoscopic rectal cancer surgery: body mass index and laparoscopic rectal cancer surgery. Colorectal Dis. 2013;15:463–9.
Zhou Y, Wu L, Li X, Wu X, Li B. Outcome of laparoscopic colorectal surgery in obese and nonobese patients: a meta-analysis. Surg Endosc. 2012;26:783–9.
Toma O, Suntrup P, Stefanescu A, et al. Pharmacokinetics and tissue penetration of cefoxitin in obesity: implications for risk of surgical site infection. Anesth Analg. 2011;113:730–7.
He Y, Wang J, Bian H, Deng X, Wang Z. BMI as a predictor for perioperative outcome of laparoscopic colorectal surgery: a pooled analysis of comparative studies. Dis Colon Rectum. 2017;60:433–45.
Sammour T, Jones IT, Gibbs P, Chandra R, Steel MC, Shedda SM, et al. Comparing oncological outcomes of laparoscopic versus open surgery for colon cancer: analysis of a large prospective clinical database: analysis of a large prospective clinical database. J Surg Oncol. 2015;111:891–8.
Zhao L-Y. Laparoscopic vs open extended right hemicolectomy for colon cancer. World J Gastroenterol. 2014;20:7926.
Biondo S, Gálvez A, Ramírez E, Frago R, Kreisler E. Emergency surgery for obstructing and perforated colon cancer: patterns of recurrence and prognostic factors. Tech Coloproctol. 2019;23:1141–61.
Biondo S, Kreisler E, Millan M, Fraccalvieri D, Golda T, Ragué JM, et al. Differences in patient postoperative and long-term outcomes between obstructive and perforated colonic cancer. Am J Surg. 2008;195:427–32.
Genser L, Manceau G, Mege D, Bridoux V, Lakkis Z, Venara A, et al. 30-day postoperative morbidity of emergency surgery for obstructive right- and left-sided colon cancer in obese patients: a multicenter cohort study of the French Surgical Association. Dig Surg. 2020;37:111–8.
Mahjoubi B, Moghimi A, Mirzaei R, Bijari A. Evaluation of the end colostomy complications and the risk factors influencing them in Iranian patients. Colorectal Dis. 2005;7:582–7.
Chiu C-C, Hsu W-T, Choi JJ, Galm B, Lee MG, Chang C-N, et al. Comparison of outcome and cost between the open, laparoscopic, and robotic surgical treatments for colon cancer: a propensity score-matched analysis using nationwide hospital record database. Surg Endosc. 2019;33:3757–65.
Lagares-Garcia J, O’Connell A, Firilas A, Robinson CC, Dumas BP, Hagen ME. The influence of body mass index on clinical short-term outcomes in robotic colorectal surgery: robotic colorectal surgery and obesity. Int J Med Robotics Comput Assist Surg. 2016;12:680–5.
Ceccarelli G, Costa G, Ferraro V, De Rosa M, Rondelli F, Bugiantella W. Robotic or three-dimensional (3D) laparoscopy for right colectomy with complete mesocolic excision (CME) and intracorporeal anastomosis? A propensity score-matching study comparison. Surg Endosc. 2021;35:2039–48.
Scott MJ, Baldini G, Fearon KCH, Feldheiser A, Feldman LS, Gan TJ, et al. Enhanced recovery after surgery (ERAS) for gastrointestinal surgery, part 1: pathophysiological considerations. Acta Anaesthesiol Scand. 2015;59:1212–31.
Geltzeiler CB, Rotramel A, Wilson C, Deng L, Whiteford MH, Frankhouse J. Prospective study of colorectal enhanced recovery after surgery in a community hospital. JAMA Surg. 2014;149:955.
Wang C, Feng H, Zhu X, Song Z, Li Y, Shi Y, et al. Comparative effectiveness of enhanced recovery after surgery program combined with single-incision laparoscopic surgery in colorectal cancer surgery: a retrospective analysis. Front Oncol. 2022;11: 768299.
Pedrazzani C, Conti C, Zamboni GA, Chincarini M, Turri G, Valdegamberi A, et al. Impact of visceral obesity and sarcobesity on surgical outcomes and recovery after laparoscopic resection for colorectal cancer. Clin Nutr. 2020;39:3763–70.
Arkenbosch JHC, van Erning FN, Rutten HJ, Zimmerman D, de Wilt JHW, Beijer S. The association between body mass index and postoperative complications, 30-day mortality and long-term survival in Dutch patients with colorectal cancer. Eur J Surg Oncol. 2019;45:160–6.
Massani M, Capovilla G, Ruffolo C, et al. Blood transfusions and steatohepatitis are independent risk factors for complications following liver resection for colorectal cancer liver metastases. Mol Clin Oncol. 2017;7:529–38.
Rahimli M, Perrakis A, Schellerer V, Gumbs A, Lorenz E, Franz M, et al. Robotic and laparoscopic liver surgery for colorectal liver metastases: an experience from a German Academic Center. World J Surg Oncol. 2020;18:333.
Liu Y-W, Lu C-C, Chang C-D, Lee K-C, Chen HH, Yeh WS, et al. Prognostic value of sarcopenia in patients with colorectal liver metastases undergoing hepatic resection. Sci Rep. 2020;10:6459.
Melero JT, Ortega FG, Gonzalez AM, Carmona-Saez P, Garcia Puche JL, Sugarbaker PH, et al. Prognostic factor analysis of circulating tumor cells in peripheral blood of patients with peritoneal carcinomatosis of colon cancer origin treated with cytoreductive surgery plus an intraoperative hyperthermic intraperitoneal chemotherapy procedure (CRS + HIPEC). Surgery. 2016;159:728–35.
Votanopoulos KI, Swords DS, Swett KR, Randle RW, Shen P, Stewart JH, et al. Obesity and peritoneal surface disease: outcomes after cytoreductive surgery with hyperthermic intraperitoneal chemotherapy for appendiceal and colon primary tumors. Ann Surg Oncol. 2013;20:3899–904.
Meyerhardt JA, Catalano PJ, Haller DG, Mayer RJ, Benson AB, Macdonald JS, et al. Influence of body mass index on outcomes and treatment-related toxicity in patients with colon carcinoma. Cancer. 2003;98:484–95.
Meyerhardt JA, Niedzwiecki D, Hollis D, Saltz LB, Mayer RJ, Nelson H, et al. Impact of body mass index and weight change after treatment on cancer recurrence and survival in patients with stage III colon cancer: findings from Cancer and Leukemia Group B 89803. J Clin Oncol. 2008;26:4109–15.
Abdel-Rahman O. Effect of body mass index on 5-FU-based chemotherapy toxicity and efficacy among patients with metastatic colorectal cancer; a pooled analysis of 5 randomized trials. Clin Colorectal Cancer. 2019;18:e385–93.
Sinicrope FA, Foster NR, Yothers G, Benson A, Seitz JF, Labianca R, et al. Body mass index at diagnosis and survival among colon cancer patients enrolled in clinical trials of adjuvant chemotherapy: BMI and Colon Cancer Prognosis. Cancer. 2013;119:1528–36.
Dignam JJ, Polite BN, Yothers G, Raich P, Colangelo L, O’Connell MJ, et al. Body mass index and outcomes in patients who receive adjuvant chemotherapy for colon cancer. JNCI: J Nat Cancer Inst. 2006;98:1647–54.
Gomez D, Jimenez-Fonseca P, Fernández AM, Castellanos PC, Arbizu MV, Cabañes RM, et al. Impact of obesity on quality of life, psychological distress, and coping on patients with colon cancer. Oncologist. 2021;26:e874–82.
Shahriari-Ahmadi A, Fahimi A, Payandeh M, Sadeghi M. Prevalence of oxaliplatin-induced chronic neuropathy and influencing factors in patients with colorectal cancer in Iran. Asian Pac J Cancer Prev. 2015;16:7603–6.
Zhao Y, Ji Y, Han Z, Shao L, Li Y, Zhao L. The clinical analysis of acute pancreatitis in colorectal cancer patients undergoing chemotherapy after operation. Onco Targets Ther. 2015;8:2527–33.
Chibaudel B, Tournigand C, Bonnetain F, Richa H, Benetkiewicz M, André T, et al. Therapeutic strategy in unresectable metastatic colorectal cancer: an updated review. Ther Adv Med Oncol. 2015;7:153–69.
Makowiec F, Möhrle S, Neeff H, Drognitz O, Illerhaus G, Opitz OG, et al. Chemotherapy, liver injury, and postoperative complications in colorectal liver metastases. J Gastrointest Surg. 2011;15:153–64.
Kurk SA, Peeters PHM, Dorresteijn B, Jong PA, Jourdan M, Creemers GM, et al. Loss of skeletal muscle index and survival in patients with metastatic colorectal cancer: secondary analysis of the phase 3 CAIRO3 trial. Cancer Med. 2020;9:1033–43.
Kurk S, Peeters P, Stellato R, Dorresteijn B, Jong P, Jourdan M, et al. Skeletal muscle mass loss and dose-limiting toxicities in metastatic colorectal cancer patients. J Cachexia Sarcopenia Muscle. 2019;10:803–13.
Kurk SA, Stellato RK, Peeters PHM, Dorresteijn B, Jourdan M, Oskam MJ, et al. Trajectory of body mass and skeletal muscle indices and disease progression in metastatic colorectal cancer patients. Am J Clin Nutr. 2019;110:1395–403.
Faruk Aykan N, Yildiz I, Sen F, Kilic L, Keskin S, Ciftci R, et al. Effect of increased body mass index (BMI) on time to tumour progression (TTP) in unresectable metastatic colorectal cancer (mCRC) patients treated with bevacizumab-based therapy. Med Oncol. 2013;30:679.
Patel GS, Ullah S, Beeke C, Hakendorf P, Padbury R, Price TJ, et al. Association of BMI with overall survival in patients with mCRC who received chemotherapy versus EGFR and VEGF -targeted therapies. Cancer Med. 2015;4:1461–71.
Simkens LHJ, Koopman M, Mol L, Veldhuis GJ, Ten Bokkel HD, Muller EW, et al. Influence of body mass index on outcome in advanced colorectal cancer patients receiving chemotherapy with or without targeted therapy. Eur J Cancer. 2011;47:2560–7.
Ye C, Wang X, Sun Y, Deng Y, Huang Y, Chi P. A nomogram predicting the difficulty of laparoscopic surgery for rectal cancer. Surg Today. 2021;51:1835–42.
Piessen G, Cabral C, Benoist S, Penna C, Nordlinger B. Previous transanal full-thickness excision increases the morbidity of radical resection for rectal cancer: TAE and morbidity of radical resection. Colorectal Dis. 2012;14:445–52.
Zhang X, Wu Q, Gu C, Hu T, Bi L, Wang Z. The effect of increased body mass index values on surgical outcomes after radical resection for low rectal cancer. Surg Today. 2019;49:401–9.
Baird DLH, Simillis C, Pellino G, Kontovounisios C, Rasheed S, Tekkis PP. The obesity paradox in beyond total mesorectal excision surgery for locally advanced and recurrent rectal cancer. Updates Surg. 2019;71:313–21.
Gebauer B, Meyer F, Ptok H, Steinert R, Otto R, Lippert H, et al. Impact of body mass index on early postoperative and long-term outcome after rectal cancer surgery. Visc Med. 2017;33:373–82.
Meyerhardt JA, Tepper JE, Niedzwiecki D, Hollis DR, McCollum AD, Brady D, et al. Impact of body mass index on outcomes and treatment-related toxicity in patients with stage II and III rectal cancer: findings from intergroup trial 0114. J Clin Oncol. 2004;22:648–57.
Sun Y, Xu Z, Lin H, Lu X, Huang Y, Huang S, et al. Impact of body mass index on treatment outcome of neoadjuvant chemoradiotherapy in locally advanced rectal cancer. Eur J Surg Oncol (EJSO). 2017;43:1828–34.
Liu H, Wei R, Li C, Zhao Z, Guan X, Yang M, et al. BMI may be a prognostic factor for local advanced rectal cancer patients treated with long-term neoadjuvant chemoradiotherapy. Cancer Manag Res. 2020;12:10321–32.
Bong JW, Ju Y, Seo J, Lee JA, Kang SH, Lee SI, et al. Clinical characteristics of rectal cancer patients with neoadjuvant chemoradiotherapy: a nationwide population-based cohort study in South Korea. Ann Surg Treat Res. 2021;100:282.
Yamano T, Tomita N, Sato T, Hayakawa K, Kamikonya N, Matoba S, et al. Influence of chemoradiotherapy on nutritional status in locally advanced rectal cancer: prospective multicenter study. Nutrition. 2020;77: 110807.
Wahl TS, Patel FC, Goss LE, Chu DI, Grams J, Morris MS. The obese colorectal surgery patient: surgical site infection and outcomes. Dis Colon Rectum. 2018;61:938–45.
Mackenzie H, Markar SR, Askari A, Faiz O, Hull M, Purkayastha S, et al. Obesity surgery and risk of cancer. Br J Surg. 2018;105:1650–7.
Almazeedi S, El-Abd R, Al-Khamis A, Albatineh AN, Al-Sabah S. Role of bariatric surgery in reducing the risk of colorectal cancer: a meta-analysis. Br J Surg. 2020;107:348–54.
Bailly L, Fabre R, Pradier C, Iannelli A. Colorectal cancer risk following bariatric surgery in a nationwide study of French individuals with obesity. JAMA Surg. 2020;155:395–402.
Kwak M, Mehaffey JH, Hawkins RB, Hedrick TL, Slingluff CL, Schirmer B, et al. Bariatric surgery is independently associated with a decrease in the development of colorectal lesions. Surgery. 2019;166:322–6.
Hussan H, Stanich PP, Gray DM, Krishna SG, Porter K, Conwell DL, et al. Prior bariatric surgery is linked to improved colorectal cancer surgery outcomes and costs: a propensity-matched analysis. OBES SURG. 2017;27:1047–55.
Taube M, Peltonen M, Sjöholm K, Palmqvist R, Andersson-Assarsson JC, Jacobson P, et al. Long-term incidence of colorectal cancer after bariatric surgery or usual care in the Swedish Obese Subjects study. PLoS ONE. 2021;16: e0248550.
Hussan H, Patel A, Akinyeye S, Porter K, Ahnen D, Lieberman D. Bariatric surgery is associated with a recent temporal increase in colorectal cancer resections, most pronounced in adults below 50 years of age. Obes Surg. 2020;30:4867–76.
Bruno DS, Berger NA. Impact of bariatric surgery on cancer risk reduction. Ann Transl Med. 2020;8:S13–S13.
Mafiana RN, Al Lawati AS, Waly MI, Al Farsi Y, Al Kindi M, Al MM. Association between dietary and lifestyle indices and colorectal cancer in oman: a case-control study. Asian Pac J Cancer Prev. 2018;19:3117–22.
Roslan NH, Makpol S, Mohd Yusof YA. A review on dietary intervention in obesity associated colon cancer. Asian Pac J Cancer Prev. 2019;20:1309–19.
Scazzocchio B, Varì R, Silenzi A, Giammarioli S, Masotti A, Baldassarre A, et al. Dietary habits affect fatty acid composition of visceral adipose tissue in subjects with colorectal cancer or obesity. Eur J Nutr. 2020;59:1463–72.
World Cancer Reasearch Fund International. Colorectal cancer statistics. Global Cancer Observatory. 2022. http://www.wcrf.org/int/cancer-facts-figures/data-specific-cancers/colorectal-cancer-statistics. Accessed 22 March 2022.
Beeken RJ, Croker H, Heinrich M, Obichere A, Finer N, Murphy N, et al. The impact of diet-induced weight loss on biomarkers for colorectal cancer: an exploratory study (INTERCEPT). Obesity (Silver Spring). 2017;25:S95-101.
Dan X, Ng TB, Wong JH, Chan YS, Cheung RCF, Chan WY. A hemagglutinin isolated from Northeast China black beans induced mitochondrial dysfunction and apoptosis in colorectal cancer cells. Biochim Biophys Acta. 2016;1863:2201–11.
Elgendy M, Cirò M, Hosseini A, Weiszmann J, Mazzarella L, Ferrari E, et al. Combination of hypoglycemia and metformin impairs tumor metabolic plasticity and growth by modulating the PP2A-GSK3β-MCL-1 axis. Cancer Cell. 2019;35:798-815.e5.
Mindikoglu AL, Abdulsada MM, Jain A, Jalal PK, Devaraj S, Wilhelm ZR, et al. Intermittent fasting from dawn to sunset for four consecutive weeks induces anticancer serum proteome response and improves metabolic syndrome. Sci Rep. 2020;10:18341.
Weng M-L, Chen W-K, Chen X-Y, Lu H, Sun Z-R, Yu Q, et al. Fasting inhibits aerobic glycolysis and proliferation in colorectal cancer via the Fdft1-mediated AKT/mTOR/HIF1α pathway suppression. Nat Commun. 2020;11:1869.
Clifton KK, Ma CX, Fontana L, Peterson LL. Intermittent fasting in the prevention and treatment of cancer. CA A Cancer J Clin. 2021;71:527–46.
das Virgens IPA, de Carvalho ALM, Nagashima YG, Silva FM, Fayh APT. Is perioperative fasting associated with complications, length of hospital stay and mortality among gastric and colorectal cancer patients? A cohort study. Sao Paulo Med J. 2020;138:407–13.
Baade PD, Meng X, Youl PH, Aitken JF, Dunn J, Chambers SK. The impact of body mass index and physical activity on mortality among patients with colorectal cancer in Queensland Australia. Cancer Epidemiol Biomarkers Prev. 2011;20:1410–20.
Oruç Z, Kaplan MA. Effect of exercise on colorectal cancer prevention and treatment. WJGO. 2019;11:348–66.
Lee MK, Kim J-Y, Kim D-I, Kang D-W, Park J-H, Ahn K-Y, et al. Effect of home-based exercise intervention on fasting insulin and Adipocytokines in colorectal cancer survivors: a randomized controlled trial. Metabolism. 2017;76:23–31.
Brown JC, Zhang S, Ligibel JA, Irwin ML, Jones LW, Campbell N, et al. Effect of exercise or metformin on biomarkers of inflammation in breast and colorectal cancer: a randomized trial. Cancer Prev Res (Phila). 2020;13:1055–62.
Machado P, Morgado M, Raposo J, Mendes M, Silva CG, Morais N. Effectiveness of exercise training on cancer-related fatigue in colorectal cancer survivors: a systematic review and meta-analysis of randomized controlled trials. Support Care Cancer. 2022;30:5601–3.
Onerup A, Andersson J, Angenete E, Bock D, Börjesson M, Ehrencrona C, et al. Effect of short-term homebased pre- and postoperative exercise on recovery after colorectal cancer surgery (PHYSSURG-C): a randomized clinical trial. Ann Surg. 2022;275:448–55.
Lee MK, Kim NK, Jeon JY. Effect of the 6-week home-based exercise program on physical activity level and physical fitness in colorectal cancer survivors: a randomized controlled pilot study. PLoS One. 2018;13: e0196220.
Cramer L, Hildebrandt B, Kung T, Wichmann K, Springer J, Doehner W, et al. Cardiovascular function and predictors of exercise capacity in patients with colorectal cancer. J Am Coll Cardiol. 2014;64:1310–9.
Dragano NRV, Fernø J, Diéguez C, López M, Milbank E. Recent updates on obesity treatments: available drugs and future directions. Neuroscience. 2020;437:215–39.
Glueck CJ, Fontaine RN, Wang P, Subbiah MTR, Weber K, Illig E, et al. Metformin reduces weight, centripetal obesity, insulin, leptin, and low-density lipoprotein cholesterol in nondiabetic, morbidly obese subjects with body mass index greater than 30. Metabolism. 2001;50:856–61.
Ilyas Z, Perna S, Al-thawadi S, Alalwan TA, Riva A, Petrangolini G, et al. The effect of Berberine on weight loss in order to prevent obesity: a systematic review. Biomed Pharmacother. 2020;127: 110137.
Buse JB, Wexler DJ, Tsapas A, Rossing P, Mingrone G, Mathieu C, et al. 2019 Update to: Management of Hyperglycemia in Type 2 Diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2020;43:487–93.
Fontbonne A, Charles MA, Juhan-Vague I, Bard J-M, Andre P, Isnard F, et al. The effect of metformin on the metabolic abnormalities associated with upper-body fat distribution. BIGPRO Study Group Diabetes Care. 1996;19:920–6.
Sehdev A, Shih Y-CT, Vekhter B, Bissonnette MB, Olopade OI, Polite BN. Metformin for primary colorectal cancer prevention in patients with diabetes: a case-control study in a US population: Metformin and Colorectal Cancer. Cancer. 2015;121:1071–8.
Deng M, Lei S, Huang D, Wang H, Xia S, Xu E, et al. Suppressive effects of metformin on colorectal adenoma incidence and malignant progression. Pathol - Res Pract. 2020;216: 152775.
Coyle C, Cafferty FH, Vale C, Langley RE. Metformin as an adjuvant treatment for cancer: a systematic review and meta-analysis. Ann Oncol. 2016;27:2184–95.
Jiang S, Lu Q. A new contribution for an old drug: Prospect of metformin in colorectal oncotherapy. J Cancer Res Ther. 2021;17:1608–17.
Bragagnoli AC, Araujo RLC, Ferraz MW, dos Santos LV, Abdalla KC, Comar F, et al. Metformin plus lrinotecan in patients with refractory colorectal cancer: a phase 2 clinical trial. Br J Cancer. 2021;124:1072–8.
Henderson D, Frieson D, Zuber J, Solomon SS. Metformin has positive therapeutic effects in colon cancer and lung cancer. Am J Med Sci. 2017;354:246–51.
Kaltenmeier C, Morocco B, Yazdani H, Reitz K, Meyer K, Molinari M, et al. Impact of metformin use on survival in patients undergoing liver resection for colorectal cancer metastases. Am Surg. 2021;87:1766–74.
El-fatatry BM, Ibrahim OM, Hussien FZ, Mostafa TM. Role of metformin in oxaliplatin-induced peripheral neuropathy in patients with stage III colorectal cancer: randomized, controlled study. Int J Colorectal Dis. 2018;33:1675–83.
Fernandes JM, Jandrey EHF, Koyama FC, Leite KRM, Camargo AA, Costa ÉT, et al. Metformin as an alternative radiosensitizing agent to 5-fluorouracil during neoadjuvant treatment for rectal cancer. Dis Colon Rectum. 2020;63:918–26.
Miranda VC, Braghiroli MI, Faria LD, Bariani G, Alex A, Bezerra Neto JE, et al. Phase 2 trial of metformin combined with 5-fluorouracil in patients with refractory metastatic colorectal cancer. Clin Colorectal Cancer. 2016;15:321-328.e1.
Dai W, Mu L, Cui Y, Li Y, Chen P, Xie H, et al. Berberine promotes apoptosis of colorectal cancer via regulation of the long non-coding RNA (lncRNA) cancer susceptibility candidate 2 (CASC2)/AU-binding factor 1 (AUF1)/B-cell CLL/lymphoma 2 (Bcl-2) axis. Med Sci Monit. 2019;25:730–8.
Wang Y, Wang Y, Ai L, Zhang H, Li G, Wang Z, et al. Linear skeletal muscle index and muscle attenuation may be new prognostic factors in colorectal carcinoma treated by radical resection. Front Oncol. 2022;12: 839899.
Nie Q, Peng WW, Wang Y, Zhong L, Zhang X, Zeng L. β-catenin correlates with the progression of colon cancers and berberine inhibits the proliferation of colon cancer cells by regulating the β-catenin signaling pathway. Gene. 2022;818: 146207.
Chen Y, Zheng Y, Wen S, Liu F. Regulation of MFN2 by berberine alleviates obesity exacerbated colitis. Biochem Biophys Res Commun. 2020;531:250–5.
Páramo-Zunzunegui J, Ramos-Carrasco A, Alonso-García M, Cuberes-Montserrat R, Rodríguez-Caravaca G, Durán-Poveda M. Altered preoperative nutritional status in colorectal cancer: a not so infrequent issue. J Nutr Metab. 2020;2020:5049194.
Cederholm T, Barazzoni R, Austin P, Ballmer P, Biolo G, Bischoff SC, et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr. 2017;36:49–64.
Tan S, Meng Q, Jiang Y, Zhuang Q, Xi Q, Xu J, et al. Impact of oral nutritional supplements in post-discharge patients at nutritional risk following colorectal cancer surgery: a randomised clinical trial. Clin Nutr. 2021;40:47–53.
Haidari F, Abiri B, Iravani M, Ahmadi-Angali K, Vafa M. Randomized study of the effect of vitamin D and Omega-3 fatty acids cosupplementation as adjuvant chemotherapy on inflammation and nutritional status in colorectal cancer patients. J Diet Suppl. 2020;17:384–400.
Ravasco P, Monteiro-Grillo I, Camilo M. Individualized nutrition intervention is of major benefit to colorectal cancer patients: long-term follow-up of a randomized controlled trial of nutritional therapy. Am J Clin Nutr. 2012;96:1346–53.
Maunsell R, Sodergren S, Hopkinson J, Shaw C, Foster C, Wheelwright S. Nutritional care in colorectal cancer—what is the state of play? Colorectal Dis. 2021;23:3227–33.
de Freitas JS, de Oliveira Pedron ÉL, de Lima e Silva Aliprandi J, Laurentino GC, Gatti AL, Forones NM, et al. The effect of chemotherapy on dietary intake and nutritional status in patients with colorectal neoplasms and the importance of nutritional counseling. Support Care Cancer. 2022;30:3885–91.
Nishida C, Mucavele P. Monitoring the rapidly emerging public health problem of overweight and obesity: the WHO Global Database on Body Mass Index. SCN News. 2004;29:5–12.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63.
Zhou B, Coorperative Meta-Analysis Group Of Working Group On Obesity In China. Prospective study for cut-off points of body mass index in Chinese adults. Zhonghua Liu Xing Bing Xue Za Zhi. 2002;23:431–4.
Gruberg L, Weissman NJ, Waksman R, Fuchs S, Deible R, Pinnow EE, et al. The impact of obesity on the short-term andlong-term outcomes after percutaneous coronary intervention: the obesity paradox? J Am Coll Cardiol. 2002;39:578–84.
Aparicio T, Ducreux M, Faroux R, Barbier E, Manfredi S, Lecomte T, et al. Overweight is associated to a better prognosis in metastatic colorectal cancer: a pooled analysis of FFCD trials. Eur J Cancer. 2018;98:1–9.
Yang Z, Wei X, Pan Y, Min Z, Xu J, Yu B. Colon cancer combined with obesity indicates improved survival- research on relevant mechanism. Aging. 2020;12:23778–94.
Ding PQ, Batra A, Xu Y, McKinnon GP, Cheung WY. Obesity and its impact on outcomes in patients with stage III colon cancer receiving adjuvant chemotherapy. Clin Colorectal Cancer. 2020;19:209–18. https://doi.org/10.1016/j.clcc.2022.02.003.
Dell’Aquila E, Rossini D, Galletti A, Stellato M, Boccaccino A, Conca V, et al. Prognostic and predictive role of body mass index (BMI) in metastatic colorectal cancer (mCRC): a pooled analisys of tribe and tribe-2 studies by GONO. Clinical Colorectal Cancer. 2022;S153300282200024X.
Ortega LS, Bradbury KE, Cross AJ, Morris JS, Gunter MJ, Murphy N. A Prospective investigation of body size, body fat composition and colorectal cancer risk in the UK Biobank. Sci Rep. 2017;7:17807.
Dash C, Yu J, Nomura S, Lu J, Rosenberg L, Palmer JR, et al. Obesity is an initiator of colon adenomas but not a promoter of colorectal cancer in the Black Women’s Health Study. Cancer Causes Control. 2020;31:291–302.
Kasi PM, Zafar SY, Grothey A. Is obesity an advantage in patients with colorectal cancer? Expert Rev Gastroenterol Hepatol. 2015;9:1339–42.
Kim BR, Yoo TK, Kim HK, Ryu IH, Kim JK, Lee IS, et al. Oculomics for sarcopenia prediction: a machine learning approach toward predictive, preventive, and personalized medicine. EPMA Journal. 2022;13:367–82.
Yeoh A, Mannalithara A, Ladabaum U. Cost-effectiveness of earlier or more intensive colorectal cancer screening in overweight and obese patients. Clin Gastroenterol Hepatol. 2022;S1542–3565(22):00726–31. https://doi.org/10.1016/j.cgh.2022.07.028.
Liu Y, May BH, Zhang AL, Guo X, Lu C, Xue CC, et al. Acupuncture and related therapies for treatment of postoperative ileus in colorectal cancer: a systematic review and meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med. 2018;2018:3178472.
Dai L, Wang M, Zhang K-P, Wang L, Zheng H-M, Li C-B, et al. Modified acupuncture therapy, long-term acupoint stimulation versus sham control for weight control: a multicenter, randomized controlled trial. Front Endocrinol (Lausanne). 2022;13: 952373.
Winters-Stone K. Tai Ji Quan for the aging cancer survivor: mitigating the accelerated development of disability, falls, and cardiovascular disease from cancer treatment. J Sport Health Sci. 2014;3:52–7.
Siu PM, Yu AP, Chin EC, Yu DS, Hui SS, Woo J, et al. Effects of tai chi or conventional exercise on central obesity in middle-aged and older adults : a three-group randomized controlled trial. Ann Intern Med. 2021;174:1050–7.
Gothe NP, Erlenbach E. Feasibility of a yoga, aerobic and stretching-toning exercise program for adult cancer survivors: the STAYFit trial. J Cancer Surviv. 2022;16:1107–16.
Jakicic JM, Davis KK, Rogers RJ, Sherman SA, Barr S, Marcin ML, et al. Feasibility of integration of yoga in a behavioral weight loss intervention: a randomized trial. Obesity (Silver Spring). 2021;29:512–20.
Liu S-S, Shi Q, Li H-J, Yang W, Han S-S, Zong S-Q, et al. Right- and left-sided colorectal cancers respond differently to traditional Chinese medicine. World J Gastroenterol. 2017;23:7618–25.
Zhang C, Sheng J, Xie W, Luo X, Xue Y, Xu G-L, et al. Mechanism and basis of traditional Chinese medicine against obesity: prevention and treatment strategies. Front Pharmacol. 2021;12: 615895.
Araújo MM, Montalvão-Sousa TM, Teixeira P da C, Figueiredo ACMG, Botelho PB. The effect of probiotics on postsurgical complications in patients with colorectal cancer: a systematic review and meta-analysis. Nutr Rev. 2022;nuac069. https://doi.org/10.1093/nutrit/nuac069.
Dikeocha IJ, Al-Kabsi AM, Eid EEM, Hussin S, Alshawsh MA. Probiotics supplementation in patients with colorectal cancer: a systematic review of randomized controlled trials. Nutr Rev. 2021;80:22–49.
Aldoori J, Cockbain AJ, Toogood GJ, Hull MA. Omega-3 polyunsaturated fatty acids: moving towards precision use for prevention and treatment of colorectal cancer. Gut. 2022;71:822–37.
Banjari I, Kožić S. Dietary intake of vitamin B12 in relation to diet and lifestyle characteristics in a population at high risk for colorectal cancer. Cent Eur J Public Health. 2018;26:253–9.
Koole JL, Bours MJL, Geijsen AJMR, Gigic B, Ulvik A, Kok DE, et al. Circulating B-vitamin biomarkers and B-vitamin supplement use in relation to quality of life in patients with colorectal cancer: results from the FOCUS consortium. Am J Clin Nutr. 2021;113:1468–81.
Wesselink E, Bours MJL, de Wilt JHW, Aquarius M, Breukink SO, Hansson B, et al. Chemotherapy and vitamin D supplement use are determinants of serum 25-hydroxyvitamin D levels during the first six months after colorectal cancer diagnosis. J Steroid Biochem Mol Biol. 2020;199: 105577.
Golubnitschaja O, Baban B, Boniolo G, Wang W, Bubnov R, Kapalla M, et al. Medicine in the early twenty-first century: paradigm and anticipation - EPMA position paper 2016. EPMA J. 2016;7:23.
Aquila G, Re Cecconi AD, Brault JJ, Corli O, Piccirillo R. Nutraceuticals and exercise against muscle wasting during cancer cachexia. Cells. 2020;9:2536.
Kenkhuis M-F, van Roekel EH, Koole JL, Breedveld-Peters JJL, Breukink SO, Janssen-Heijnen MLG, et al. Increases in adipose tissue and muscle function are longitudinally associated with better quality of life in colorectal cancer survivors. Sci Rep. 2021;11:12440.
Karabulut S, Dogan I, Usul Afsar C, Karabulut M, Karaman S, Ferhatoglu F, et al. Does nutritional status affect treatment tolarability, response and survival in metastatic colorectal cancer patients? Results of a prospective multicenter study. J Oncol Pharm Pract. 2021;27:1357–63.
Acknowledgements
The authors thank all the study participants for their contributions. We would also like to thank Prof. Huan-gan Wu for his assistance in writing this manuscript. We are particularly grateful to the anonymous reviewers for their contribution to the optimization of this manuscript. We thank KetengEdit (www.ketengedit.com) for English language editing service.
Funding
This work was supported by Shanghai Clinical Research Center for Acupuncture and Moxibustion (20MC1920500) and the National Natural Science Foundation of China (82174501) (81973955) (82004474).
Author information
Authors and Affiliations
Contributions
Lu-Yi Wu contributed to the study’s conception and design. Li-Ming Chen and Yun-Jia Gu contributed equally to this manuscript. They performed the literature search, wrote the first draft of the manuscript, and designed the first set of figures. Hong-Xiao Xu and Mu-En Gu edited the manuscript and provided corrections. Lu-Yi Wu and Mu-En Gu acquired funding. Jing Li and Lu-Yi Wu read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
All the authors had complete access to the manuscript and agreed to submit it for publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gu, YJ., Chen, LM., Gu, ME. et al. Body mass index–based predictions and personalized clinical strategies for colorectal cancer in the context of PPPM. EPMA Journal 13, 615–632 (2022). https://doi.org/10.1007/s13167-022-00306-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13167-022-00306-0