Abstract
Although high body-mass index (BMI) is associated with increased risk of developing colorectal cancer (CRC), many CRC patients lose weight before diagnosis. BMI is often reported close to diagnosis, which may have led to underestimation or even reversal of direction of the BMI-CRC association. We aimed to assess if and to what extent potential bias from prediagnostic weight loss has been considered in available epidemiological evidence. We searched PubMed and Web of Science until May 2022 for systematic reviews and meta-analyses investigating the BMI-CRC association. Information on design aspects and results was extracted, including if and how the reviews handled prediagnostic weight loss as a potential source of bias. Additionally, we analyzed how individual cohort studies included in the latest systematic review handled the issue. Overall, 18 reviews were identified. None of them thoroughly considered or discussed prediagnostic weight loss as a potential source of bias. The majority (15/21) of cohorts included in the latest review did not exclude any initial years of follow-up from their main analysis. Although the majority of studies reported having conducted sensitivity analyses in which initial years of follow-up were excluded, results were reported very heterogeneously and mostly for additional exclusions of 1–2 years only. Where explicitly reported, effect estimates mostly increased with increasing length of exclusion. The impact of overweight and obesity on CRC risk may be larger than suggested by the existing epidemiological evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Overweight and obesity, commonly defined by a body-mass index (BMI) ≥ 25 to 30 kg/m2 and ≥ 30 kg/m2[1], respectively, are established risk factors for a variety of cancers including colorectal cancer (CRC) [2]. Recent reviews have indicated that overweight and obese individuals have about 18% and 32% greater risk of CRC compared to those with normal weight [3,4,5]. However, a large 2017 meta-analysis reported even stronger associations with colorectal adenomas, the precursors of most CRCs, with a risk increase by more than 40% for both overweight and obesity [6]. Furthermore, there is evidence that CRC patients may experience substantial weight loss in the preclinical phase prior to diagnosis [7], suggesting that the strength of the association of overweight and obesity with CRC risk may have been underestimated in epidemiological studies due to prediagnostic weight loss. In case–control studies, BMI is often reported for the time close to or shortly before diagnosis among cases. In such studies, prediagnostic weight loss may have led to underestimation or even reversal of direction of the BMI-CRC association [8, 9]. For example, Low et al. [8] showed that being overweight or obese at diagnosis is associated with a 31% reduction of early-onset CRC risk. In contrast to that, their post-hoc analyses suggested that the cases were more likely to have had a significant reduction in weight in the 5-year period before diagnosis. In cohort studies with BMI ascertained at baseline, underestimation of the BMI-CRC association may also be of concern as cancers diagnosed during the early years of follow-up may have been present in preclinical state already at enrollment and may have led to weight loss before enrollment. Mean sojourn time in preclinical state has been estimated to be around 3–6 years for CRC [10,11,12]. Tumor-associated weight loss due to preclinical CRC or its precursors may again have led to an underestimation of the BMI-CRC association unless the initial years of follow-up were excluded from the analysis.
This study aims to evaluate if and to what extent the association of overweight and obesity with CRC may have been underestimated in epidemiological studies by the aforementioned sources of bias. Therefore, we conducted an umbrella review and searched for reviews that investigated the BMI-CRC association and to examine if and how these reviews and the included studies in those reviews handled potential bias due to prediagnostic weight loss.
Methods
Our study protocol was registered with PROSPERO at inception (registration number: CRD42021256462). Changes made during the review were recorded in PROSPERO. We followed standardized methodology guidelines summarized in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)(Supplementary File 1) [13].
Search strategy and selection criteria
We systematically searched PubMed and Web of Science from inception through 9th May 2022 for systematic reviews and meta-analyses that investigated the association between overweight and obesity with risk of colorectal cancer using a predefined search algorithm. Search terms included ‘colorectal cancer’, ‘body-mass index’, ‘risk factor’ (or related terms), combined with ‘systematic review’, and ‘meta-analysis’ (or related terms, see Supplementary File 2 for the details of the algorithms used for both databases). The reference lists of identified studies were also searched for additional relevant studies. We excluded letters, editorials, comments, news, and articles published in languages other than English.
Studies were eligible for inclusion if they were a systematic review or a meta-analysis study, and if the primary exposure of interest was obesity or overweight (defined by BMI, (weight in kilograms) / (height in meters)2) and if the primary outcome was colorectal cancer or its anatomic subsites, rectal or colon cancer. Studies that exclusively used different measures of adiposity (e.g. waist-to-hip ratio, weight, weight gain, etc.) were not included.
Data extraction and evaluation of study quality
Data extraction was performed independently by two authors (MM and HL). Initial disagreements were resolved by consensus after further review and discussion. From each study, the following information was extracted: First author’s name, article title, publication year, number of included studies (grouped by study type), exposure definition, summary effect size estimates (most adjusted) and their 95% CIs, model type, and measures of heterogeneity (I2 statistic or Q-test’s p-value). Where possible, a combined effect estimate for colon and rectal cancer was extracted, otherwise, both effect size estimates were reported. The same was done for sex-specific/combined effect size estimates. However, to ensure comparability of summary estimates from different reviews and easier interpretation of forest plots, we performed a generic inverse-variance random-effects meta-analysis for studies that only reported sex- or site-specific estimates.
The methodological quality of each systematic review was independently assessed by two investigators (MM and HL) using AMSTAR-2 (A Measurement Tool to Assess Systematic Reviews) [14], and initial disagreements were again resolved by consensus after further review and discussion. AMSTAR-2 is a validated and reliable measurement tool consisting of 16 items and includes ratings for the quality of the search, reporting, transparency, and statistical analysis (Supplementary File 3). According to the suggestions in AMSTAR-2 guidelines, items 2, 4, 7, 9, 11, 13, and 15 were defined as critical domains, and items 1, 3, 5, 6, 8, 10, 12, 14, and 16 were defined as non-critical domains. The final rating criteria were defined as follows: high quality when one or no non-critical weaknesses were found, moderate when two or more non-critical weaknesses were found, low quality when one critical weakness with or without non-critical weaknesses was found, and critically low quality when two or more critical weaknesses with or without non-critical weaknesses were found.
Potential bias arising from prediagnostic weight loss was ascertained by two dichotomous (yes/no) items: ‘timing of BMI ascertainment’ was used as a criterion for case–control studies and was rated as ‘considered’ in the review/meta-analysis if the exact timing of BMI in each of the primary studies was reported, and if timing was considered in the analysis and estimation of the summary effects (through stratification/subgroup analysis/exclusion of studies with BMI ascertainment too close to diagnosis). ‘Consideration of sojourn time’ was used as a criterion for cohort studies and was rated as ‘considered’ in the reviews/meta-analyses if they presented summary analyses for cohorts in which at least the first 4 years of follow-up were excluded.
To further investigate how individual primary studies handled potential bias due to prediagnostic weight loss, we extracted the information from the individual studies included in the most recent systematic review, which only included cohort studies. The information we recorded was if and how many of the first years of follow-up were excluded in the main analyses or potential sensitivity analyses. From studies that expanded the exclusion of the first years of follow-up in sensitivity analysis, we recorded and compared hazard ratios and their 95% CIs from main and sensitivity analyses. All analyses and data visualization were conducted using R version 4.1.1.
Results
Characteristics of the included studies
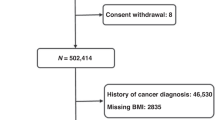
Overall, a total of 7,950 articles were retrieved from the systematic search in two databases. In the end, 18 publications met all inclusion criteria (Fig. 1) [2,3,4,5, 15,16,17,18,19,20,21,22,23,24,25,26,27,28].
Table 1 provides an overview of the characteristics of the included reviews. Of these 18 reviews, 13 (72%) included only cohort studies (prospective or retrospective), while the remaining 5 included both cohort and case–control studies. Summary estimates of relative risk were most commonly reported for the risk of obesity compared to normal weight according to the WHO definition (obesity: BMI ≥ 30 kg/m2; overweight: 25 kg/m2 ≤ BMI < 30 kg/m2; normal: 18.5 kg/m2 ≤ BMI < 25 kg/m2; underweight: BMI < 18.5 kg/m2) and for the risk associated with a 5 kg/m2 BMI increase. Three reviews reported results for ‘High versus Low BMI’ (based on included primary studies), one review reported relative risk per 8 kg/m2 increase in BMI, and another review reported results for an increase in BMI by one standard deviation.
We assessed the methodological quality of 17 reviews (1 publication was not a systematic review) using the AMSTAR-2 tool (Supplementary File 3). Almost all (16/17, 94%) of the assessed studies had two or more critical flaws [mostly in item 7, “Did the review authors provide a list of excluded studies and justify the exclusions?” (15/17, 88%), and item 13, “Did the review authors account for risk of bias in individual studies when interpreting/ discussing the results of the review?” (14/17, 82%)]. Therefore, most of the reviews had a critically low quality score, except Fang et al. 2018 [28], which had a moderate quality score. Timing of the BMI ascertainment and sojourn time consideration were analyzed separately. None of the included reviews fulfilled our predefined criteria. Of the two criteria for assessing the risk of bias due to timing of the BMI ascertainment, only Ning and colleagues (2010) [19] fulfilled the first criterion by reporting the exact time-point at which the BMI was recorded in the primary studies. Sojourn time was not analyzed nor discussed in any of the reviews.
Overview of summary results from systematic reviews and meta-analyses
Since the included reviews reported risk estimates for different definitions of exposure, we focused on the two most common definitions: WHO definition of obesity (BMI ≥ 30 kg/m2) in comparison to normal weight (BMI ≥ 18.5 kg/m2 and < 25.0 kg/m2), and 5 kg/m2 increments in BMI. Furthermore, due to expected differences between colon cancer and rectal cancer risk, site-specific results are presented separately for both outcomes. Summary results of the different meta-analyses are presented by forest plots. Due to the overlap of studies included in the meta-analyses, we refrained from summarizing the summary estimates of association by meta-analysis. Figure 2A shows the summary risk estimates for the association between obesity and CRC. Summary estimates of relative risk for both sexes and both sites combined ranged from 1.19 to 1.41, and were reported as 1.33 (95% CI 1.25 to 1.42) and 1.31 (95% CI 1.12 to 1.42) in the two most recent meta-analyses. Figure 2B shows the summary risk estimates for the association between 5 kg/m2 increments in BMI and CRC. Relative risks for both exposure definitions were consistently higher for men than for women, and for colon cancer than for rectal cancer in subgroup- and site-specific meta-analyses (Supplementary Figures S1 and S2).
Forest plot of the summary estimates from the reviews with meta-analyses in the umbrella review of the association between CRC risk and a) obesity (BMI ≥ 30 kg/m2) in comparison with normal weight (BMI ≥ 18.5 kg/m2 and BMI < 25.0 kg/m2); b) 5 kg/m2 increase in BMI BMI = body-mass index, CC = colon cancer, CI = confidence interval, CRC = colorectal cancer, F = female, M = male, RC = rectal cancer, RR = relative risk
More detailed assessment of the sojourn times in the most recent review of cohort studies
An overview of how individual cohort studies (those included in the most recent review by Zhang et al. 2021) [3] handled the issue of sojourn time is presented in Supplementary Table 1 and Fig. 3 [29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54]. In the main analysis, more than two-thirds of the studies (15/21, 71%) did not exclude any of the first years of follow-up, 5 excluded the first year, and one excluded the first 4 years of follow-up. In the sensitivity analysis, two-thirds (14/21) did not exclude more than the first 2 years of follow-up. Hazard ratios from studies that have excluded more years in their sensitivity analysis than in their main analysis and have explicitly reported their estimates, are shown in Supplementary Table 2. The majority of the studies (12/15) extended their exclusion of the initial follow-up years by just 1 or 2 years. There was very high heterogeneity in the details of reporting. Some studies only stated that the results did not change significantly in the sensitivity analysis, and some reported only the estimates that reached statistical significance. On the other hand, few studies reported all of the results of their sensitivity analysis. In these studies, estimates from the sensitivity analyses were somewhat larger than the corresponding estimates in the main analyses in most cases.
Discussion
It is well established that overweight and obesity are important risk factors for many cancers, including CRC [2]. To the best of our knowledge, this is the first umbrella review to systematically investigate how previous systematic reviews and meta-analyses, as well as the primary studies included in the most recent systematic review, approached prediagnostic weight loss as a potential source of bias. Our analysis suggests that more rigorous attention to this potential source of bias may be needed to fully disclose the impact of overweight and obesity on CRC risk.
Sojourn time for CRC in the preclinical state has consistently been estimated to be about 3–6 years [10,11,12]. This prediagnostic period often goes along with weight loss [7, 55, 56]. Since most of the case–control studies ascertained BMI close to the time of diagnosis, such studies, and systematic reviews and meta-analyses that included them, are likely to have underestimated the relationship between overweight and obesity and CRC. In initial analyses, Low et al. (2020) showed that increased BMI was associated with a significant reduction in the odds for early-onset CRC (ORs: 0.69 (95% CI 0.55–0.87) and 0.69 (0.55–0.86) for overweight and obesity, respectively). While this study focused on early-onset CRC, there is no reason to assume this would be different for CRC at older ages. Post-hoc analyses showed that cases had a higher chance of experiencing considerable weight loss than controls (ORs: 2.23 (95% CI 1.76–2.83) for a weight loss ≥ 5 kg and 2.50 (1.65–3.78) for weight loss ≥ 10 kg). This means that the initial estimates are, as the authors explained, most likely strong underestimates of the true relationship between excess weight and CRC.
Although most of the reviews and meta-analyses identified in our umbrella review included only prospective cohort studies, the lack of or very limited exclusion of the initial years of follow-up, even in sensitivity analyses, in the original studies suggests that both the individual cohort studies and the meta-analyses again have underestimated the obesity-CRC association. In none of the systematic reviews was this major concern thoroughly addressed in the discussion.
A closer look at the primary studies included in the most recent systematic review and meta-analysis (Zhang et al. 2021) [3] reveals that, in the main analysis, 15 out of 21 studies (71%) did not implement any sort of exclusion of the first years of follow-up, and even where sensitivity analyses were reported, they rarely excluded more than the first one or 2 years of follow-up. Furthermore, even if conducted, such sensitivity analyses varied strongly in the details of reporting. For example, Bhaskaran et al. [43] and Song et al. [36] thoroughly reported the results of their sensitivity analyses. Most other studies only partially and selectively reported sensitivity analysis results, e.g. when a nonsignificant estimate between BMI and CRC risk reached statistical significance, while others simply stated that the results remained similar, without reporting the actual estimates. In most of the few studies that explicitly reported sensitivity analyses, the effect estimates increased, albeit mostly to a limited extent, possibly due to the short periods of exclusion. Concerns about bias due to prediagnostic weight loss are even more salient in meta-analyses which were consistently based on the results of the main analyses (with typically no or minimal exclusion of initial years of follow-up) rather than the results of the sensitivity analyses.
Most of the reviews/meta-analyses reported a positive association of BMI with CRC. For obesity, relative risk summary estimates for both sexes and both sites ranged from 19 to 41% increased CRC risk. However, a 2017 systematic review and meta-analysis of 168,201 subjects evaluating the association of investigator-measured body-mass index and colorectal adenomas, the precursors of most CRCs, revealed even strong estimates for both overweight and obesity: 44% (95% CI 30–61%) and 42% (95% CI 24–63%) increased risk compared to normal weight [6]. For a 5 kg/m2 increase in BMI, summary estimates in the reviews were in the range of 6% to 18% increased CRC risk (combined for both sexes and both sites). Summary estimates were significantly higher for CC than for RC. The World Cancer Research Fund (WCRF) and the American Institute for Cancer Research (AICR) Continuous Update Project 2018 report includes a particularly low summary estimate of 5% (95% CI 3–7%) increase in CRC risk per 5-unit BMI increment [57]. This report is widely regarded as a trusted and authoritative scientific resource due to its most rigorous methodology. Nevertheless, like all of the meta-analyses published in peer-reviewed journals identified in our umbrella review, this estimate is expected to be affected by lack of or very limited precautions against bias due to disease-related weight loss of the included cohort studies and may therefore likewise underestimate the BMI-CRC association.
The estimates of relative risk of CRC associated with overweight and obesity from epidemiological studies and their meta-analyses are commonly used to calculate the fraction of CRC cases in the population that is attributable to overweight and obesity. These so-called population-attributable fractions additionally depend on the prevalence of overweight and obesity in the population. Given the high and increasing prevalence of overweight and obesity, even modest increases in risk of CRC translate into relatively high shares of CRC cases statistically attributable to overweight and obesity. For example, in Germany, two-thirds of adult men (67%) and half of the women (53%) are overweight or obese (BMI ≥ 25 kg/m2), and about a quarter are obese (23% of men, 24% of women) [58]. Prevalences are even higher in the US, where, in 2018, 74% of all adults were either overweight or obese, and 42% were obese [59]. The estimated proportions of CRC cases due to overweight and obesity based on previous estimates of CRC risks from epidemiological studies were already as high as 13.2% for Germany [60]. The corresponding estimate for the US was 5.2%. However, it was based on the previously mentioned very low estimate by the WCRF-AICR [61]. It is expected that these estimates would be substantially higher when taking underestimation of risks due to prediagnostic weight loss into account.
Our study focused on the role of prediagnostic weight loss as a potential source of bias. Although probably being a particularly relevant source of bias, other sources of potential bias also require careful attention. These include, for example, the inaccuracy of weight measures, in particular in studies based on self-reported weight. In cohort studies, where weight is ascertained prior to disease manifestation, less than perfect weight ascertainment would most likely be nondifferential with respect to CRC risk, and therefore further attenuate observed BMI-CRC associations. Other potential sources of biases, such as imperfect control for confounding (despite major attempts of multivariate adjustments commonly made in epidemiological studies) may lead to either over- or underestimation of the BMI-CRC association.
A key strength of this paper is that it includes a comprehensive review of existing systematic reviews and meta-analyses investigating the relationship between BMI and CRC. Nonetheless, our analysis also has several limitations. Firstly, despite a comprehensive, systematic search in multiple databases, we cannot exclude having missed some systematic reviews. However, even if that should be the case, this would not invalidate our findings since we aimed to explore if and how reviews, in general, approached the prediagnostic weight loss problem. Secondly, although we thoroughly reviewed the individual studies included in the most recent systematic review and identified several studies that have, at least to some extent, addressed the issue of prediagnostic weight loss, heterogeneity in reporting of these studies precluded redoing the meta-analysis based on such sensitivity analyses. Thirdly, our study focused exclusively on BMI as an indicator of overweight and obesity. Future studies should also consider alternative indicators, such as waist-to-hip ratio, to investigate if their association with CRC risk might be affected by prediagnostic weight loss in a similar manner.
In conclusion, our umbrella review suggests that the association between overweight and obesity and CRC risk may be stronger than suggested by previous studies and meta-analyses which paid no or only limited attention to prediagnostic weight loss. Future studies should pay more thorough attention and adequately account for lifetime history of weight in order to fully disclose the impact of overweight and obesity on CRC risk. Even though prediagnostic weight loss may be of particular concern for CRC, it may also play an important role for other cancers and some non-cancer diseases whose association with overweight and obesity may also have been underestimated by previous research. Further research should therefore take care of prediagnostic weight loss in an even broader context. Most notably, however, our study underlines the need for enhanced efforts for more effective prevention of overweight and obesity, which have become more prevalent in many countries in the past decades, and which may be stronger risk factors for CRC and possibly also for other cancers and diseases than suggested by existing epidemiological studies.
Change history
17 January 2024
A Correction to this paper has been published: https://doi.org/10.1007/s10654-023-01092-3
Abbreviations
- AICR:
-
American Institute for Cancer Research
- BMI:
-
Body-mass index
- CC:
-
Colon cancer
- CI:
-
Confidence interval
- CRC:
-
Colorectal cancer
- OR:
-
Odds ratio
- RC:
-
Rectal cancer
- RR:
-
Relative risk
- WCRF:
-
World Cancer Research Fund
- WHO:
-
World Health Organization
References
World Health Organization. Obesity: preventing and managing the global epidemic. 2000. Available from: https://apps.who.int/iris/handle/10665/42330
Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. The Lancet. 2008;371:569–78.
Zhang C, Cheng Y, Luo D, Wang J, Liu J, Luo Y, et al. Association between cardiovascular risk factors and colorectal cancer: a systematic review and meta-analysis of prospective cohort studies. EClinicalMedicine. 2021;34:100794.
Lei X, Song S, Li X, Geng C, Wang C. Excessive body fat at a young age increases the risk of colorectal cancer: a systematic review and meta-analysis. Nutr Cancer Routledge. 2021;73:1601–12.
Garcia H, Song M. Early-life obesity and adulthood colorectal cancer risk: a meta-analysis. Rev Panam Salud Publica. 2019;43: e3.
Wong MC-s, Chan C-h, Cheung W, Fung D-h, Liang M, Huang JL-w, et al. Association between investigator-measured body-mass index and colorectal adenoma: a systematic review and meta-analysis of 168,201 subjects. Eur J Epidemiol. 2018;33(1):15–26. https://doi.org/10.1007/s10654-017-0336-x.
Nicholson BD, Thompson MJ, Hobbs FDR, Nguyen M, McLellan Julie, Green B, et al. Measured weight loss as a precursor to cancer diagnosis: retrospective cohort analysis of 43 302 primary care patients. J Cachexia Sarcopenia Muscle. 2022;13(5):2492–503. https://doi.org/10.1002/jcsm.13051.
Low EE, Demb J, Liu L, Earles A, Bustamante R, Williams CD, et al. Risk factors for early-onset colorectal cancer. Gastroenterology. 2020;159:492-501.e7.
Gausman V, Dornblaser D, Anand S, Hayes RB, O’Connell K, Du M, et al. Risk factors associated with early-onset colorectal cancer. Clin Gastroenterol Hepatol. 2020;18:2752-2759.e2.
Launoy G, Smith TC, Duffy SW, Bouvier V. Colorectal cancer mass-screening: estimation of faecal occult blood test sensitivity, taking into account cancer mean sojourn time. Int J Cancer. 1997;73:220–4.
Prevost TC, Launoy G, Duffy SW, Chen HH. Estimating sensitivity and sojourn time in screening for colorectal cancer: a comparison of statistical approaches. Am J Epidemiol. 1998;148:609–19.
Brenner H, Altenhofen L, Katalinic A, Lansdorp-Vogelaar I, Hoffmeister M. Sojourn time of preclinical colorectal cancer by sex and age: estimates from the German national screening colonoscopy database. Am J Epidemiol. 2011;174:1140–6.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Dai Z, Xu Y-C, Niu L. Obesity and colorectal cancer risk: a meta-analysis of cohort studies. World J Gastroenterol. 2007;13:4199–206.
Larsson SC, Wolk A. Obesity and colon and rectal cancer risk: a meta-analysis of prospective studies. Am J Clin Nutr. 2007;86:556–65.
Moghaddam AA, Woodward M, Huxley R. Obesity and risk of colorectal cancer: a meta-analysis of 31 studies with 70,000 events. Cancer Epidemiol Biomark Prev. 2007;16:2533–47.
Huxley RR, Ansary-Moghaddam A, Clifton P, Czernichow S, Parr CL, Woodward M. The impact of dietary and lifestyle risk factors on risk of colorectal cancer: a quantitative overview of the epidemiological evidence. Int J Cancer. 2009;125:171–80.
Ning Y, Wang L, Giovannucci EL. A quantitative analysis of body mass index and colorectal cancer: findings from 56 observational studies. Obes Rev. 2010;11:19–30.
Dobbins M, Decorby K, Choi BCK. The association between obesity and cancer risk: a meta-analysis of observational studies from 1985 to 2011. ISRN Prev Med. 2013;2013:680536.
Esposito K, Chiodini P, Capuano A, Bellastella G, Maiorino MI, Rafaniello C, et al. Colorectal cancer association with metabolic syndrome and its components: a systematic review with meta-analysis. Endocrine. 2013;44:634–47.
Johnson CM, Wei C, Ensor JE, Smolenski DJ, Amos CI, Levin B, et al. Meta-analyses of colorectal cancer risk factors. Cancer Causes Control. 2013;24:1207–22.
Ma Y, Yang Y, Wang F, Zhang P, Shi C, Zou Y, et al. Obesity and risk of colorectal cancer: a systematic review of prospective studies. PLoS One. 2013;8:e53916.
Robsahm TE, Aagnes B, Hjartåker A, Langseth H, Bray FI, Larsen IK. Body mass index, physical activity, and colorectal cancer by anatomical subsites: a systematic review and meta-analysis of cohort studies. Eur J Cancer Prev. 2013;22:492–505.
Wang J, Yang D-L, Chen Z-Z, Gou B-F. Associations of body mass index with cancer incidence among populations, genders, and menopausal status: a systematic review and meta-analysis. Cancer Epidemiol. 2016;42:1–8.
Freisling H, Arnold M, Soerjomataram I, O’Doherty MG, Ordóñez-Mena JM, Bamia C, et al. Comparison of general obesity and measures of body fat distribution in older adults in relation to cancer risk: meta-analysis of individual participant data of seven prospective cohorts in Europe. Br J Cancer. 2017;116:1486–97.
Abar L, Vieira AR, Aune D, Sobiecki JG, Vingeliene S, Polemiti E, et al. Height and body fatness and colorectal cancer risk: an update of the WCRF-AICR systematic review of published prospective studies. Eur J Nutr. 2018;57:1701–20.
Fang X, Wei J, He X, Lian J, Han D, An P, et al. Quantitative association between body mass index and the risk of cancer: a global meta-analysis of prospective cohort studies. Int J Cancer. 2018;143:1595–603.
Moore LL, Bradlee ML, Singer MR, Splansky GL, Proctor MH, Ellison RC, et al. BMI and waist circumference as predictors of lifetime colon cancer risk in Framingham study adults. Int J Obes. 2004;28:559–67.
Engeland A, Tretli S, Austad G, Bjørge T. Height and body mass index in relation to colorectal and gallbladder cancer in two million Norwegian men and women. Cancer Causes Control. 2005;16:987–96.
Oh SW, Yoon YS, Shin S-A. Effects of excess weight on cancer incidences depending on cancer sites and histologic findings among men: Korea National Health Insurance Corporation study. J Clin Oncol. 2005;23:4742–54.
Rapp K, Schroeder J, Klenk J, Stoehr S, Ulmer H, Concin H, et al. Obesity and incidence of cancer: a large cohort study of over 145,000 adults in Austria. Br J Cancer. 2005;93:1062–7.
Larsson SC, Rutegård J, Bergkvist L, Wolk A. Physical activity, obesity, and risk of colon and rectal cancer in a cohort of Swedish men. Eur J Cancer. 2006;42:2590–7.
Lukanova A, Björ O, Kaaks R, Lenner P, Lindahl B, Hallmans G, et al. Body mass index and cancer: results from the Northern Sweden health and disease cohort. Int J Cancer. 2006;118:458–66.
Reeves GK, Pirie K, Beral V, Green J, Spencer E, Bull D, et al. Cancer incidence and mortality in relation to body mass index in the Million Women Study: cohort study. BMJ. 2007;335:1134.
Song Y-M, Sung J, Ha M. Obesity and risk of cancer in postmenopausal Korean women. JCO Wolters Kluwer. 2008;26:3395–402.
Bassett JK, Severi G, English DR, Baglietto L, Krishnan K, Hopper JL, et al. Body size, weight change, and risk of colon cancer. Cancer Epidemiol Biomarkers Prev. 2010;19:2978–86.
Laake I, Thune I, Selmer R, Tretli S, Slattery ML, Veierød MB. A prospective study of body mass index, weight change, and risk of cancer in the proximal and distal colon. Cancer Epidemiol Biomarkers Prev. 2010;19:1511–22.
Doubeni CA, Major JM, Laiyemo AO, Schootman M, Zauber AG, Hollenbeck AR, et al. Contribution of behavioral risk factors and obesity to socioeconomic differences in colorectal cancer incidence. J Natl Cancer Inst. 2012;104:1353–62.
Matsuo K, Mizoue T, Tanaka K, Tsuji I, Sugawara Y, Sasazuki S, et al. Association between body mass index and the colorectal cancer risk in Japan: pooled analysis of population-based cohort studies in Japan. Ann Oncol. 2012;23:479–90.
Renehan AG, Flood A, Adams KF, Olden M, Hollenbeck AR, Cross AJ, et al. Body mass index at different adult ages, weight change, and colorectal cancer risk in the national institutes of health-AARP cohort. Am J Epidemiol. 2012;176:1130–40.
Li H, Yang G, Xiang Y-B, Gao J, Zhang X, Zheng W, et al. Body weight, fat distribution and colorectal cancer risk: a report from cohort studies of 134 255 Chinese men and women. Int J Obes (Lond). 2013;37:783–9.
Bhaskaran K, Douglas I, Forbes H, Santos-Silva I, Leon DA, Smeeth L. Body-mass index and risk of 22 specific cancers: a population-based cohort study of 524 million UK adults. Lancet. 2014;384:755–65.
Steins Bisschop CN, van Gils CH, Emaus MJ, Bueno-de-Mesquita HB, Monninkhof EM, Boeing H, et al. Weight change later in life and colon and rectal cancer risk in participants in the EPIC-PANACEA study. Am J Clin Nutr. 2014;99:139–47.
Han X, Stevens J, Truesdale KP, Bradshaw PT, Kucharska-Newton A, Prizment AE, et al. Body mass index at early adulthood, subsequent weight change and cancer incidence and mortality. Int J Cancer. 2014;135:2900–9.
Lu Y, Ness-Jensen E, Hveem K, Martling A. Metabolic predispositions and increased risk of colorectal adenocarcinoma by anatomical location: a large population-based cohort study in Norway. Am J Epidemiol. 2015;182:883–93.
Kantor ED, Udumyan R, Signorello LB, Giovannucci EL, Montgomery S, Fall K. Adolescent body mass index and erythrocyte sedimentation rate in relation to colorectal cancer risk. Gut. 2016;65:1289–95.
Hanyuda A, Cao Y, Hamada T, Nowak JA, Qian ZR, Masugi Y, et al. Body mass index and risk of colorectal carcinoma subtypes classified by tumor differentiation status. Eur J Epidemiol. 2017;32:393–407.
Levi Z, Kark JD, Katz LH, Twig G, Derazne E, Tzur D, et al. Adolescent body mass index and risk of colon and rectal cancer in a cohort of 1.79 million Israeli men and women: a population-based study. Cancer. 2017;123:4022–30.
Andreasson A, Hagström H, Sköldberg F, Önnerhag K, Carlsson AC, Schmidt PT, et al. The prediction of colorectal cancer using anthropometric measures: a Swedish population-based cohort study with 22 years of follow-up. United European Gastroenterol J. 2019;7:1250–60.
Bjørge T, Häggström C, Ghaderi S, Nagel G, Manjer J, Tretli S, et al. BMI and weight changes and risk of obesity-related cancers: a pooled European cohort study. Int J Epidemiol. 2019;48:1872–85.
Liu P-H, Wu K, Ng K, Zauber AG, Nguyen LH, Song M, et al. Association of obesity with risk of early-onset colorectal cancer among women. JAMA Oncol. 2019;5:37–44.
Noh H, Charvat H, Freisling H, Ólafsdóttir GH, Ólafsdóttir EJ, Tryggvadóttir L, et al. Cumulative exposure to premenopausal obesity and risk of postmenopausal cancer: a population-based study in Icelandic women. Int J Cancer. 2020;147:793–802.
Wang L, Jin G, Yu C, Lv J, Guo Y, Bian Z, et al. Cancer incidence in relation to body fatness among 0.5 million men and women: Findings from the China Kadoorie Biobank. Int J Cancer. 2020;146:987–98.
Bapuji SB, Sawatzky JA. Understanding weight loss in patients with colorectal cancer: a human response to illness. In Oncology nursing forum 2010 (Vol. 37, No. 3) pp 303–310
van Zutphen M, Geelen A, Boshuizen HC, Winkels RM, Geijsen AJMR, Wesselink E, et al. Pre-to-post diagnosis weight trajectories in colorectal cancer patients with non-metastatic disease. Support Care Cancer. 2019;27:1541–9.
World Cancer Research Fund/American Institute for Cancer Research. Continuous Update Project Expert Report 2018. Diet, nutrition, physical activity and colorectal cancer. Available from: Available at dietandcancerreport.org
Schienkiewitz A, Mensink G, Kuhnert R, Lange C. Overweight and obesity among adults in Germany. Robert Koch-Institut, Epidemiologie und Gesundheitsberichterstattung; 2017; Available from: https://edoc.rki.de/handle/176904/2663
National Center for Health Statistics. NHANES 2017–2018. 2020. Available from: https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.aspx?BeginYear=2017
Behrens G, Gredner T, Stock C, Leitzmann MF, Brenner H, Mons U. Cancers due to excess weight, low physical activity, and unhealthy diet. Dtsch Arztebl Int. 2018;115:578–85.
Islami F, Goding Sauer A, Miller KD, Siegel RL, Fedewa SA, Jacobs EJ, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA A Cancer J Clin. 2018;68:31–54.
Funding
Open Access funding enabled and organized by Projekt DEAL. None.
Author information
Authors and Affiliations
Contributions
Conception and design of the study: HB. Acquisition of data: MM and HL. Data analysis and interpretation: MM and HB. Drafting of the manuscript: MM and HB. All authors provided comments, revised the draft, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to the wrong Supplementary file 7 was originally published with this article; it has now been replaced with the correct file.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mandic, M., Li, H., Safizadeh, F. et al. Is the association of overweight and obesity with colorectal cancer underestimated? An umbrella review of systematic reviews and meta-analyses. Eur J Epidemiol 38, 135–144 (2023). https://doi.org/10.1007/s10654-022-00954-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-022-00954-6