Abstract
The use of breast density as an intermediate or predictive marker of breast cancer risk is limited by an incomplete understanding of the etiology of breast density. High blood levels of endogenous estrogens and androgens are associated with increased risk of breast cancer among postmenopausal women. We sought to examine whether these hormones are also associated with breast density. The Wisconsin Breast Density Study enrolled 257 postmenopausal women, ages 55–70 years, with no history of postmenopausal hormone use, from mammography clinics in Madison, Wisconsin. Subjects provided a blood sample for sex hormone analysis, and breast density was measured from subjects' screening mammograms using a computer-assisted thresholding method. Numerous sex hormones were associated with breast density in age-adjusted analyses. However, further adjustment for body mass index and other potentially confounding factors substantially attenuated or eliminated these associations. In the fully adjusted model, there remained a positive association between percent breast density and serum progesterone (P = 0.03), with percent density rising from 11.9% (95% CI: 9.8, 14.1%) among women in the lowest quartile of serum progesterone to 15.4% (12.9, 18.2%) among women in the highest quartile. There was also a positive association between sex hormone binding globulin and percent breast density (P = 0.06). In contrast, there were no independent associations between percent breast density and estradiol (total, free, or bioavailable), estrone, estrone sulfate, or testosterone (total, free, or bioavailable). These results suggest that breast density has a hormonal etiology; however, it may differ in important ways from that of breast cancer risk.
Similar content being viewed by others
Introduction
Mammographic breast density is one of the strongest known risk factors for breast cancer [1–4]. A recent meta-analysis estimated that women with density in 75% or more of the mammogram had a 4.6-fold increase in breast cancer risk compared to women with density in less than 5% [5]. Breast density is also associated with many of the same factors that are associated with breast cancer risk, including parity, age at first birth, and use of postmenopausal hormones [2, 4, 6].
These characteristics have led many to consider the use of mammographic breast density as an intermediate marker of breast cancer risk [7–9]. The use of breast density as a surrogate endpoint could enable studies of breast cancer risk that are smaller, less expensive, and of shorter duration [10]. However, certain features of breast density challenge this framework. Body mass index (BMI), a known breast cancer risk factor, is inversely associated with breast density [11, 12]. Additionally, recent evidence suggests that breast density does not mediate the relations between body mass index or postmenopausal hormone use and breast cancer risk [13, 14]. This suggests that the influence of certain risk factors on breast cancer risk may operate through biological pathways independent of breast density.
Most established breast cancer risk factors are believed to influence breast cancer risk through sex hormone pathways [15, 16]. High circulating sex hormone levels have consistently been associated with elevated breast cancer risk [17–19]. Menstrual, reproductive, and lifestyle risk factors have all been associated with increased estrogen exposure and changes in estrogen metabolism [20–22]. While postmenopausal hormone use has been associated with increased breast density [23, 24], the relation between circulating endogenous sex hormone levels and breast density is unclear [8]. To improve our understanding of the etiology of breast density, we examined the relation between circulating endogenous sex hormones and breast density in a population of postmenopausal women. Since exogenous hormone use could obscure this relation, the study was restricted to women who had never used postmenopausal hormones.
Materials and Methods
The Wisconsin Breast Density Study is a cross-sectional study of postmenopausal women receiving a screening mammogram in Madison, WI. This study was approved by the University of Wisconsin Health Sciences Institutional Review Board. All subjects provided written informed consent.
Study Population
Eligible participants for this study were postmenopausal women, aged 55–70 years, attending the UW Health West-Madison Clinic or UW Health Breast Center to receive a screening mammogram. Postmenopausal status was defined as having no menstrual cycles within the past 12 months. Women who reported a previous diagnosis of breast cancer, breast implants, or having ever used postmenopausal hormone therapy were not eligible for participation in the study. All participants were included in study analyses regardless of the results of their screening mammogram.
A letter of invitation for this research study was sent through the mail to women aged 55–70 years who were due for their annual mammogram at the UW Health West-Madison Clinic or UW Health Breast Center. In the letter, women were informed of the study and provided with the contact information for the University of Wisconsin Office of Clinical Trials (UW OCT) research specialist coordinating recruitment. Additionally, pamphlets inviting women to participate were provided at check-in to all women attending the screening mammography clinics whose electronic medical record data did not meet any of the exclusion criteria. During the screening mammogram, the technician inquired with each potentially eligible woman to determine if she was interested in participating in the study and whether she met the eligibility criteria. For interested and eligible women, a research specialist then provided a written description of the general nature of study and the study requirements, confirmed that the woman met the eligibility criteria, and answered any questions. Signed informed consent and Health Insurance Portability and Accountability Act forms were obtained by the research specialist. As a recruitment incentive, participants were offered $25 which was paid upon completing the study.
A total of 268 subjects were recruited between June 25, 2008 and July 3, 2009. During the recruitment period, 7,611 women attended the clinics for screening mammograms. Of these, 3,201 (42.1%) were between the ages of 55 and 70 years. Of these age-eligible women, 1,302 (40.7%) were deemed potentially eligible based on a review of their electronic medical record. Of these, 268 were enrolled (20.6%). The number of women who were truly eligible is unknown; many women may have determined that they were ineligible after receiving the pamphlet (e.g., if they were premenopausal or had previously taken postmenopausal hormones not included in their UW Health medical record).
Data Collection
Following the subject's mammogram and consent to participate in the study, a questionnaire was administered to the subject and a blood sample was obtained.
Questionnaire
The questionnaire included items known or suspected to be associated with breast cancer or mammographic density, including age, height, weight, age at menarche, age at first pregnancy, parity, age at menopause, first degree family history of breast cancer, alcohol consumption, physical activity, lactation history, smoking, and education level. Alcohol consumption was ascertained as the number of bottles or cans of beer, glasses of wine, and drinks of hard liquor consumed per day, week, or month. Physical activity was assessed as the average number of hours per week spent doing physically vigorous activities that cause large increases in heart rate or breathing, such as participating in sports activities, climbing stairs, heavy gardening, or lifting/carrying heavy objects. To assess smoking history, women reported whether they had smoked more than 100 cigarettes in their lifetime. For those reporting more than 100 cigarettes, we recorded the age she started smoking, the age she stopped (if applicable), and the average number of cigarettes or packs of cigarettes she smoked per day over the entire time she was smoking.
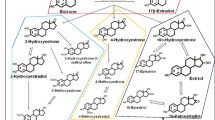
Blood Analyses
A trained phlebotemist from the UW OCT obtained a 30-mL whole blood sample from the participant via venipuncture, collected in three uncoated glass 10-mL red top vacutainer tubes (no anticoagulant; Fisher Scientific, Pittsburgh, Pennsylvania). Blood samples were allowed to clot for 30 min, then spun down in a centrifuge at 2,500 rpm for 20 min. Serum was aliquoted in 2-mL aliquots frozen at −70°C. Sex hormone analyses were conducted by Dr. Frank Stanczyk at the Reproductive Endocrine Research Laboratory at the University of Southern California. Progesterone, testosterone, estrone, and estradiol were quantified by validated, previously described radioimmunoassays (RIAs) [25–27]. Estrone sulfate was measured by direct RIA using a commercial kit (Beckman Coulter Diagnostic Systems Laboratories, Webster, Texas). Sex hormone binding globulin (SHBG) was quantified by direct chemiluminescent immunoassay using the Immulite analyzer (Siemens Medical Solutions Diagnostics, Malvern, Pennsylvania). The inter-assay coefficients of variation ranged between 7% and 12%. The assay sensitivities for progesterone, testosterone, estrone, estradiol, SHBG, and estrone sulfate are 0.02 ng/ml, 1.5 ng/dL, 4 pg/ml, 2 pg/ml, 1 nM, and 0.025 ng/ml, respectively. Free and bioavailable (non-SHBG-bound) testosterone and estradiol were calculated using the measured total testosterone and estradiol levels, SHBG concentrations, and an average assumed concentration for albumin [28, 29]. This method has been found to have high validity, with Pearson's correlation coefficients ≥ 0.80 between free testosterone or free estradiol values calculated using this method and the values measured by dialysis-based methods [30].
Mammographic Density
Participants underwent their normally scheduled screening mammogram. All women received a digital mammogram conducted on either a Senographe 2000D (GE Medical Systems) or a Clearview CSm2 CR (Fujifilm Corporation) machine. Digital copies of the craniocaudal view of the left breast were obtained for the quantitative analysis of mammographic breast density using a computer-assisted thresholding method. “Cumulus” software [31] was used to measure percent breast density as a continuous variable. All density measurements were done by the same reader (EJAB), who was blinded in respect to serum hormone levels and all identifying information. A 10% sample was read twice for quality control purposes. Reliability for the continuous density measure was assessed by the intraclass correlation coefficient [32]. We found excellent reliability, with intraclass correlation coefficients of 0.98, 0.99, and 0.92 for percent density, total breast area, and dense area, respectively. Lower 95% confidence limits for these measures were 0.96, 0.99, and 0.86, respectively.
Statistical Analyses
Three women had insufficient serum available for hormone analyses. There were eight women (all under 60 years old) with estradiol levels greater than 35 pg/mL, suggesting that they were not truly postmenopausal. Exclusion of these 11 women left a total of 257 samples available for analysis. Testosterone levels were missing for three women and certain covariates were missing data for a small fraction of subjects (see Table 1). Multiple imputation was used to impute missing testosterone levels and covariate data. Ten imputations were conducted using the Markov Chain Monte Carlo method [33]. The imputation model contained percent breast density and all variables listed in Tables 1 and 2, except for free and bioavailable estradiol/testosterone values, as these are derived from total estradiol/testosterone and SHBG values. For subsequent analyses, each model was fit separately to the ten imputed datasets and their results combined for statistical inferences using the methods of Rubin [34].
Spearman correlation coefficients were calculated to assess the association between each serum sex hormone and body mass index. Multivariable linear regression was used to assess the association between serum sex hormone levels and the square root of percent breast density (measured continuously), while adjusting for age, body mass index, and other variables. Percent density was square root transformed to improve the normality of the data, as the distribution of percent density was positively skewed. Potential confounders which were considered included all variables listed in Table 1. A reverse stepwise procedure was used to select variables for inclusion in the final model. Beginning with a full multivariable model including all potential confounders listed in Table 1, covariates were sequentially removed based on the largest P value. All remaining covariates significantly associated with percent density at the P < 0.10 level were selected for inclusion in the final multivariable model. These included age, body mass index, parity, vigorous physical activity, pack years of smoking, and family history of breast cancer. These covariates were parameterized in the models as displayed in Table 1, with the exception of age and body mass index which were included as continuous variables. In separate models, adjusted least-squares mean levels of square root percent density were calculated according to quartiles of each sex hormone level [35]. These mean values were reverse transformed for display purposes. Tests of trends across hormone quartile groups were conducted by inclusion of hormone quartile as an ordinal term in the regression models. Wald tests for effect modification by body mass index (measured continuously) and interactions between hormones were conducted by including cross-product interaction terms in the regression models. All statistical analyses were performed using SAS Statistical Software (Version 9; SAS Institute, Inc., Cary, North Carolina).
Results
Selected characteristics of the study subjects are shown in Table 1. The mean age of participants was 60.7 years (standard deviation, 4.4). Eighty-one percent of the participants reported a natural menopause, whereas 15% reported a surgical menopause (3% reported other causes). Approximately 32% of participants were overweight (25 ≤ BMI < 30 kg/m2) and 37% were obese (BMI ≥ 30 kg/m2). Median percent breast density among the study subjects was 11.3% (mean 15.6, standard deviation 13.1, range 0.4–71.2). Age, BMI, parity, pack years of smoking, and a family history of breast cancer were inversely associated with percent density in the multivariable-adjusted model.
The distribution of sex hormone concentrations is displayed in Table 2. Given the strong association between BMI and breast density, we examined the correlation of each hormone with BMI. There were strong positive correlations between BMI and total, free, and bioavailable estradiol (r = 0.49–0.57), and a strong negative correlation between BMI and SHBG (r = −0.54). Moderate positive correlations were observed for estrone, estrone sulfate, and free and bioavailable testosterone (r = 0.18–0.37) and a moderate inverse correlation for progesterone (r = −0.18). There was no correlation between total testosterone and BMI (r = 0.01).
Table 3 displays the relation between each hormone and percent breast density. In age-adjusted analyses, breast density was lower among women with higher estradiol, free estradiol, bioavailable estradiol, estrone, free testosterone, and bioavailable testosterone levels (P < 0.05). Breast density was higher among women with higher progesterone and SHBG levels (P < 0.001). Additional adjustment for BMI largely attenuated these associations, with progesterone the only hormone which remained significantly associated with percent density (P = 0.007). Further adjustment for other potential confounders had a relatively minor effect on the regression coefficients. In the final multivariable-adjusted model, mean percent density was 15.4% among women in the highest quartile of progesterone, compared to 11.9% among women in the lowest quartile. This positive association did not appear to vary by body mass index (P interaction = 0.92). There was also a positive association between SHBG and percent density in the multivariable-adjusted model, though it was of borderline statistical significance (P = 0.06). There was no clear pattern in percent density when women were categorized by quartile of SHBG (P trend = 0.98).
Since combined progesterone and estrogen hormone therapy is known to raise breast cancer risk, we examined the potential interaction between progesterone and estrogen levels in their association with breast density. Breast density was most elevated among women with high progesterone and low total or free estradiol levels (Table 4). There was no statistically significant interaction between progesterone and total or free estradiol (P interaction > 0.8). Within each quartile of total or free estradiol concentration, the magnitude and direction of the association between progesterone and breast density was similar.
Discussion
We found that all examined hormones, with the exception of total testosterone and estrone sulfate, were associated with percent breast density in our cohort of postmenopausal women with no history of postmenopausal hormone use. These associations were largely eliminated after adjusting for body mass index and other confounding variables. However, after full adjustment, there remained a positive association between progesterone and percent breast density, and the suggestion of a positive association between percent breast density and SHBG. These findings provide evidence that breast density is related to endogenous hormone levels, though this etiology may differ in important ways from that of breast cancer.
Our observations of age-adjusted associations between circulating sex hormones and percent breast density in postmenopausal women are similar to those reported by the majority of previous studies [36–39]. However, as is typically observed [8], body mass index was strongly associated with both breast density and most sex hormones in our study population. We found that further adjustment for body mass index substantially attenuated or eliminated most of the associations between sex hormones and breast density. These results are consistent with the findings of a recent review by Becker and Kaaks [8] of eight previous studies in postmenopausal women, which reported that the majority of studies have observed no relation between percent density and serum estrogens, testosterone, estrone, and estrone sulfate after adjustment for BMI.
Relatively few studies have examined the relation between progesterone and breast density. Whereas three studies reported a null association [36, 37, 39], Greendale et al. [40] found a positive association, with an absolute difference in percent breast density of about 5 percentage points between the lowest and highest quintiles of progesterone. We observed a difference of about 3.5 percentage points between the lowest and highest quartiles, and about 4.5 percentage points between the lowest and highest quintiles. Each of the previous studies included former users of postmenopausal hormones, which may potentially account for variation in their findings. Multiple lines of evidence suggest that progesterone may promote breast epithelial cell proliferation and carcinogenesis. Proliferative activity in normal breast tissue is highest in the luteal phase of the menstrual cycle when progesterone levels are highest [20]. In vitro studies have reported a variety of effects of progestins on mammary cells [41], including increased cell proliferation in cultured cells from mouse mammary tumors [42]. Finally, the Women's Health Initiative randomized trials have demonstrated that addition of progestin to estrogen in postmenopausal hormone formulations is associated with elevated breast cancer risk [43], whereas estrogen alone was not associated with increased risk [44]. Few studies have directly examined the relation between circulating progesterones and breast cancer risk in postmenopausal women. In the Nurses' Health Study, baseline progesterone levels were not associated with breast cancer risk among postmenopausal women in a nested case–control study [18].
A number of previous studies have reported a positive association between SHBG and percent breast density after adjusting for BMI [36, 38–40, 45], though null relations have also been reported [37, 46, 47]. We observed a borderline significant positive association between percent breast density and SHBG. Notably, however, there did not appear to be a clear dose–response pattern in percent density according to quartile of SHBG. Additionally, there was no relation between bioavailable (non-SHBG bound) estradiol or testosterone and breast density. Thus, the mechanism by which SHBG may influence breast density is unclear.
A number of limitations should be considered in the interpretation of this study. Since all women were recruited at screening mammography clinics in Madison, Wisconsin, the generalizability of the results may be limited. Ninety-seven percent (N = 249) of subjects reported white race. A single blood draw for each subject was used for the measurement of sex hormone levels. The hormone level at the time of enrollment in the study may not be representative of long-term exposure to that hormone. However, the Nurses Health Study has found intraclass correlation coefficients of 0.7–0.8 for most sex hormones measured up to 3 years apart on the same women [48]. Single measures of sex hormone levels in postmenopausal women have been adequate to reveal an association with breast cancer risk [17]. Further, a single measurement is likely more representative of long-term hormone levels among women, such as those in our study, who have never used postmenopausal hormones. Nonetheless, misclassification due to a single measure would tend to bias our results towards a null finding. Thus, this is unlikely to explain the positive association we observed between progesterone and breast density. Our study has a relatively small sample size, and power was insufficient to rule out potential interactions or detect small differences in breast density according to sex hormone levels. However, the power of the study was maximized by using a continuous measure of breast density with high reliability, and there was sufficient power to detect clinically significant differences in breast density. Furthermore, to increase our sensitivity to differences in endogenous hormone levels, the study population was restricted to women who had never used postmenopausal hormones.
Multiple imputations were used to impute the small numbers of missing testosterone and covariate data. Sensitivity analyses in which subjects with missing testosterone values were excluded revealed a negligible impact upon the results.
Our results suggest that the hormonal etiology of breast density may differ from that of breast cancer. Increased levels of circulating estrogens and androgens have consistently been associated with elevated breast cancer risk [17]. For instance, women in the highest quartile of total or free estradiol levels have a twofold increased risk of breast cancer compared to women in the lowest quartile [17]. Yet, our data adds further evidence that circulating endogenous androgens and estrogens are not strongly related to breast density. Interestingly, Tamimi et al. [49] recently reported that the association between circulating sex hormone levels and breast cancer risk was not attenuated by adjustment for mammographic breast density, suggesting that they are independent risk factors. Thus, it appears that breast density may not be an appropriate surrogate marker for studying breast cancer risk factors that operate through estrogen or androgen pathways.
In summary, our results indicate that the age-adjusted associations between most circulating sex hormones and breast density are eliminated after adjustment for BMI and other potential confounders. After adjustment for BMI, only progesterone and SHBG were associated with mammographic breast density among our population of postmenopausal women who had never used postmenopausal hormones. Continued research will be necessary to understand the biological mechanisms through which sex hormones and breast density influence breast cancer risk. As progesterone was the only hormone associated with breast density in this study, our results suggest that increased attention to this hormone in particular is warranted.
References
Boyd NF, Guo H, Martin LJ et al (2007) Mammographic density and the risk and detection of breast cancer. N Engl J Med 356(3):227–236
Vacek PM, Geller BM (2004) A prospective study of breast cancer risk using routine mammographic breast density measurements. Cancer Epidemiol Biomark Prev 13(5):715–722
Vachon CM, van Gils CH, Sellers TA et al (2007) Mammographic density, breast cancer risk and risk prediction. Breast Cancer Res 9(6):217
Boyd NF, Martin LJ, Bronskill M et al (2010) Breast tissue composition and susceptibility to breast cancer. J Natl Cancer Inst 102(16):1224–1237
McCormack VA, dos Santos Silva I (2006) Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomark Prev 15(6):1159–1169
Boyd NF, Lockwood GA, Byng JW, Tritchler DL, Yaffe MJ (1998) Mammographic densities and breast cancer risk. Cancer Epidemiol Biomark Prev 7(12):1133–1144
Boyd NF, Rommens JM, Vogt K et al (2005) Mammographic breast density as an intermediate phenotype for breast cancer. Lancet Oncol 6(10):798–808
Becker S, Kaaks R (2009) Exogenous and endogenous hormones, mammographic density and breast cancer risk: can mammographic density be considered an intermediate marker of risk? Recent Results Cancer Res 181:135–157
Martin LJ, Melnichouk O, Guo H et al (2010) Family history, mammographic density, and risk of breast cancer. Cancer Epidemiol Biomark Prev 19(2):456–463
Schatzkin A, Gail M (2002) The promise and peril of surrogate end points in cancer research. Nat Rev Cancer 2(1):19–27
Brisson J, Morrison AS, Kopans DB et al (1984) Height and weight, mammographic features of breast tissue, and breast cancer risk. Am J Epidemiol 119(3):371–381
Boyd NF, Lockwood GA, Byng JW et al (1998) The relationship of anthropometric measures to radiological features of the breast in premenopausal women. Br J Cancer 78(9):1233–1238
Boyd NF, Martin LJ, Li Q et al (2006) Mammographic density as a surrogate marker for the effects of hormone therapy on risk of breast cancer. Cancer Epidemiol Biomark Prev 15(5):961–966
Boyd NF, Martin LJ, Sun L et al (2006) Body size, mammographic density, and breast cancer risk. Cancer Epidemiol Biomark Prev 15(11):2086–2092
Key TJ, Verkasalo PK, Banks E (2001) Epidemiology of breast cancer. Lancet Oncol 2(3):133–140
Russo J, Hu YF, Yang X, Russo IH (2000) Developmental, cellular, and molecular basis of human breast cancer. J Natl Cancer Inst Monogr 27:17–37
Endogenous Hormones and Breast Cancer Collaborative Group (2002) Endogenous sex hormones and breast cancer in postmenopausal women: reanalysis of nine prospective studies. J Natl Cancer Inst 94(8):606–616
Missmer SA, Eliassen AH, Barbieri RL, Hankinson SE (2004) Endogenous estrogen, androgen, and progesterone concentrations and breast cancer risk among postmenopausal women. J Natl Cancer Inst 96(24):1856–1865
Kaaks R, Rinaldi S, Key TJ et al (2005) Postmenopausal serum androgens, oestrogens and breast cancer risk: the European prospective investigation into cancer and nutrition. Endocr Relat Cancer 12(4):1071–1082
Pike MC, Spicer DV, Dahmoush L, Press MF (1993) Estrogens, progestogens, normal breast cell proliferation, and breast cancer risk. Epidemiol Rev 15(1):17–35
Hankinson SE, Colditz GA, Willett WC (2004) Towards an integrated model for breast cancer etiology: the lifelong interplay of genes, lifestyle, and hormones. Breast Cancer Res 6(5):213–218
Dumitrescu RG, Cotarla I (2005) Understanding breast cancer risk—where do we stand in 2005? J Cell Mol Med 9(1):208–221
Greendale GA, Reboussin BA, Slone S et al (2003) Postmenopausal hormone therapy and change in mammographic density. J Natl Cancer Inst 95(1):30–37
Vachon CM, Sellers TA, Vierkant RA, Wu FF, Brandt KR (2002) Case-control study of increased mammographic breast density response to hormone replacement therapy. Cancer Epidemiol Biomark Prev 11(11):1382–1388
Goebelsmann U, Bernstein GS, Gale JA et al (1979) Serum gonadotropin, testosterone, estradiol and estrone levels prior to and following bilateral vasectomy. In: Lepow IH, Crozier R (eds) Vasectomy: immunologic and pathophysiologic effects in animals and man. Academic, New York
Goebelsmann U, Horton R, Mestman JH et al (1973) Male pseudohermaphroditism due to testicular 17b-hydroxysteroid dehydrogenase deficiency. J Clin Endocrinol Metab 36(5):867–879
Scott JZ, Stanczyk FZ, Goebelsmann U, Mishell DR Jr (1978) A double-antibody radioimmunoassay for serum progesterone using progesterone-3-(0-carboxymethyl)oximino-[125I]-iodohistamine as radioligand. Steroids 31(3):393–405
Sodergard R, Backstrom T, Shanbhag V, Carstensen H (1982) Calculation of free and bound fractions of testosterone and estradiol-17 beta to human plasma proteins at body temperature. J Steroid Biochem 16(6):801–810
Vermeulen A, Verdonck L, Kaufman JM (1999) A critical evaluation of simple methods for the estimation of free testosterone in serum. J Clin Endocrinol Metab 84(10):3666–3672
Rinaldi S, Geay A, Dechaud H et al (2002) Validity of free testosterone and free estradiol determinations in serum samples from postmenopausal women by theoretical calculations. Cancer Epidemiol Biomark Prev 11(10 Pt 1):1065–1071
Byng JW, Boyd NF, Fishell E, Jong RA, Yaffe MJ (1994) The quantitative analysis of mammographic densities. Phys Med Biol 39(10):1629–1638
Armstrong BK, White E, Saracci R (1992) Principles of exposure measurement in epidemiology, vol 21. Oxford University Press, Oxford, New York
Schafer JL (1997) Analysis of incomplete multivariate data. Chapman and Hall, New York
Rubin DB (1987) Multiple imputation for nonresponse in surveys. John Wiley & Sons, New York
SAS Institute Inc. (2009) Construction of least squares means. In: SAS/STAT 9.2 User's Guide. 2nd edn. Cary, NC: SAS Institute Inc. 2528–2531
Boyd NF, Stone J, Martin LJ et al (2002) The association of breast mitogens with mammographic densities. Br J Cancer 87(8):876–882
Tamimi RM, Hankinson SE, Colditz GA, Byrne C (2005) Endogenous sex hormone levels and mammographic density among postmenopausal women. Cancer Epidemiol Biomark Prev 14(11 Pt 1):2641–2647
Verheus M, Peeters PH, van Noord PA et al (2007) No relationship between circulating levels of sex steroids and mammographic breast density: the Prospect-EPIC cohort. Breast Cancer Res 9(4):R53
Warren R, Skinner J, Sala E et al (2006) Associations among mammographic density, circulating sex hormones, and polymorphisms in sex hormone metabolism genes in postmenopausal women. Cancer Epidemiol Biomark Prev 15(8):1502–1508
Greendale GA, Palla SL, Ursin G et al (2005) The association of endogenous sex steroids and sex steroid binding proteins with mammographic density: results from the postmenopausal estrogen/progestin interventions mammographic density study. Am J Epidemiol 162(9):826–834
Lanari C, Molinolo AA (2002) Progesterone receptors—animal models and cell signalling in breast cancer. Diverse activation pathways for the progesterone receptor: possible implications for breast biology and cancer. Breast Cancer Res 4(6):240–243
Lamb C, Simian M, Molinolo A, Pazos P, Lanari C (1999) Regulation of cell growth of a progestin-dependent murine mammary carcinoma in vitro: progesterone receptor involvement in serum or growth factor-induced cell proliferation. J Steroid Biochem Mol Biol 70(4–6):133–142
Chlebowski RT, Hendrix SL, Langer RD et al (2003) Influence of estrogen plus progestin on breast cancer and mammography in healthy postmenopausal women: the women's health initiative randomized trial. JAMA 289(24):3243–3253
Anderson GL, Limacher M, Assaf AR et al (2004) Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the women's health initiative randomized controlled trial. JAMA 291(14):1701–1712
Bremnes Y, Ursin G, Bjurstam N et al (2007) Endogenous sex hormones, prolactin and mammographic density in postmenopausal Norwegian women. Int J Cancer 121(11):2506–2511
Aiello EJ, Tworoger SS, Yasui Y et al (2005) Associations among circulating sex hormones, insulin-like growth factor, lipids, and mammographic density in postmenopausal women. Cancer Epidemiol Biomark Prev 14(6):1411–1417
Johansson H, Gandini S, Bonanni B et al (2008) Relationships between circulating hormone levels, mammographic percent density and breast cancer risk factors in postmenopausal women. Breast Cancer Res Treat 108(1):57–67
Hankinson SE, Manson JE, Spiegelman D et al (1995) Reproducibility of plasma hormone levels in postmenopausal women over a 2–3-year period. Cancer Epidemiol Biomark Prev 4(6):649–654
Tamimi RM, Byrne C, Colditz GA, Hankinson SE (2007) Endogenous hormone levels, mammographic density, and subsequent risk of breast cancer in postmenopausal women. J Natl Cancer Inst 99(15):1178–1187
Acknowledgments
This work was supported by the Komen for the Cure Foundation (FAS0703857), the Department of Defense (BC062649), and the National Cancer Institute (CA139548, CA014520). Dr. Sprague is supported by a fellowship from the American Society of Preventive Oncology, Susan G. Komen for the Cure, and the Prevent Cancer Foundation. The authors would like to thank Kristi Klein and the staff of UW Health Clinics, Dr. Walter Peppler, Eva Baird, and Lori Wollett and staff of the UW OCT for their assistance in subject recruitment and data collection; Dr. Halcyon Skinner, Dr. Marty Kanarek, John Hampton, Tammy LeCaire, Tanya Watson, Matt Walsh, Jane Maney, and Cecilia Bellcross for study-related advice; Dr. Martin Yaffe and Chris Peressotti for assistance in breast density measurements; Dr. Karen Cruickshanks, Carla Schubert, and Scott Nash for assistance in sample storage; and Julie McGregor, Kathy Peck, and Dawn Fitzgibbons for study support.
Conflict of Interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sprague, B.L., Trentham-Dietz, A., Gangnon, R.E. et al. Circulating Sex Hormones and Mammographic Breast Density among Postmenopausal Women. HORM CANC 2, 62–72 (2011). https://doi.org/10.1007/s12672-010-0056-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12672-010-0056-0