Abstract
Purpose
This review provides a focused and comprehensive update on established and emerging evidence in acute renal replacement therapy (RRT) for critically ill patients with acute kidney injury (AKI).
Principal findings
There have been considerable technological innovations in the methods and techniques for provision of extracorporeal RRT in critical illness. These have greatly expanded our capability to provide both renal and non-renal life-sustaining organ support for critically ill patients. Recent data suggest earlier initiation of RRT in AKI may confer an advantage for survival and renal recovery. Two large trials have recently shown no added benefit to augmented RRT dose delivery in AKI. Observational data have also suggested that fluid accumulation in critically ill patients with AKI is associated with worse clinical outcome. However, several fundamental clinical questions remain to be answered, including issues regarding the time to ideally initiate/discontinue RRT, the role of high-volume hemofiltration or other blood purification techniques in sepsis, and extracorporeal support for combined liver-kidney failure. Extracorporeal support with RRT in sepsis, rhabdomyolysis, and liver failure are discussed, along with strategies for drug dosing and management of RRT in sodium disorders.
Conclusions
We anticipate that this field will continue to expand to promote research and innovation, hopefully for the benefit of sick critically ill patients.
Résumé
Objectif
Cette synthèse propose une mise à jour complète et spécifique des données probantes établies et nouvelles concernant la suppléance rénale chez les patients gravement malades souffrant d’insuffisance rénale aiguë (IRA).
Constatations principales
Il y a eu d’importantes innovations technologiques au niveau des méthodes et des techniques qui permettent de procurer une suppléance rénale extracorporelle dans les cas de maladie grave. Ces innovations ont considérablement accru notre capacité de fournir une suppléance systémique de maintien de la vie à la fois au niveau des reins et d’autres organes aux patients gravement malades. Des données récentes suggèrent qu’une amorce plus précoce de la suppléance rénale chez les patients souffrant d’IRA pourrait être bénéfique en termes de survie et de récupération rénale. Deux études d’envergure ont récemment démontré qu’il n’y avait pas de bienfait supplémentaire à augmenter la dose de suppléance rénale dans les cas d’IRA. Des données observationnelles ont également suggéré que l’accumulation liquidienne chez les patients gravement malades souffrant d’IRA était associée à un pronostic moins favorable. Toutefois, plusieurs questions cliniques fondamentales demeurent encore sans réponse, notamment les questions concernant le moment idéal où amorcer/interrompre la suppléance rénale, le rôle de l’hémofiltration à volume élevé ou d’autres techniques d’épuration du sang dans les cas de sepsis, ou encore l’assistance extracorporelle lors d’insuffisance rénale et hépatique associées. Nous discutons de l’assistance extracorporelle avec suppléance rénale dans le sepsis, la rhabdomyolyse et l’insuffisance hépatique, ainsi que diverses stratégies pour la posologie des médicaments et la prise en charge de la suppléance rénale lors de troubles électrolytiques sodiques.
Conclusion
Nous prévoyons que ce domaine continuera de s’étendre afin de favoriser la recherche et l’innovation, pour le bienfait des patients gravement malades.
Similar content being viewed by others
Acute kidney injury (AKI) is encountered commonly in hospitalized patients, particularly in critical care and perioperative settings. These patients may be exposed to multiple acute kidney insults that precipitate more severe AKI.1 Observational data suggest that up to 70% of these patients require initiation of renal replacement therapy (RRT). Severe AKI in these settings has been associated independently with high morbidity, mortality, and resource use. Intensivists and anesthesiologists are often the key care providers for these patients. Accordingly, up-to-date knowledge of the principles of prescription and delivery of renal support in these patients is essential.
This article, the second of a two part series, was partnered with contributors at the 2010 Acute Kidney Injury and Renal Support in Critical Illness Symposium held on April 16, 2010 in Edmonton Canada. The aim of this review is to provide a focused and comprehensive update on recent and emerging evidence on RRT and extracorporeal kidney support for critically ill patients with AKI.
A primer on renal support physiology
The normal kidney plays an integral role in many physiologic processes, including fluid and electrolyte homeostasis, acid-base balance, and several endocrine pathways.2 While no currently available renal support modality can emulate natural kidney function, these therapies can partially replace three main functions: fluid removal, solute removal, and replenishment of bicarbonate buffer.
Aside from peritoneal dialysis, all renal support modalities entail blood being pumped from a vascular access catheter through a filter, and back through another lumen in the same access device. The filter consists of hundreds of hollow fibres with small pores, thereby acting as a semi-permeable membrane.
Fluid removal is accomplished by applying a negative pressure to the outside of the fibres leading to net fluid movement out of the blood compartment (i.e., from inside the fibres). This process, referred to as ultrafiltration (UF), removes fluid, an ultrafiltrate, which is essentially identical to plasma in its composition of small solutes (i.e., electrolytes, urea, and creatinine). While there is some net loss of solutes (termed solvent drag), the plasma concentration of solutes remains essentially unchanged.
Removal of solute and replenishment of bicarbonate buffer can be accomplished by either hemodialysis or hemofiltration. In hemodialysis, an electrolyte solution (dialysate) bathes the hollow fibres of the filter allowing accumulated solutes to diffuse down their concentration gradients from blood to dialysate, while bicarbonate buffer moves from dialysate to blood. In order to maximize the concentration gradients between the two compartments, blood and dialysate are run in a countercurrent fashion. Removal of solutes depends on solute characteristics (i.e., molecular weight, charge, protein binding, volume of distribution), membrane characteristics (i.e., thickness, number of fibres, pore size, and number), and technical factors (i.e., blood flow and dialysate flow). In hemofiltration, solute removal and bicarbonate replacement are accomplished by removal of large amounts of isotonic plasma, while replacing it with a balanced solution similar in composition to normal plasma. It can be understood as large volume UF with a physiologic fluid being returned in order to alter serum solute concentrations and avoid intravascular depletion. Hemofiltration reduces the influence of solute size on clearance, therefore improving removal of higher molecular weight substances, the clinical significance of which remains unclear.
While the nomenclature of the multiple modalities can be confusing, it is easily clarified by understanding the concepts outlined above. When prescribing renal support therapy, the clinician simply must choose a single modality (i.e., hemodialysis or hemofiltration) or combination (i.e., hemodiafiltration) and duration of therapy, which may vary from a two-hour session to a continuous period over 24 hr. When using hemodialysis, for example, a four- to six-hour therapy is described as “intermittent hemodialysis” (IHD); a six- to 12-hr therapy is known as “sustained low-efficiency dialysis” (SLED), and continuous therapy is called “continuous venovenous hemodialysis” (CVVHD). Although hemofiltration may be used in an intermittent fashion, it is primarily employed continuously either on its own in “continuous venovenous hemofiltration” (CVVH) or in combination with hemodialysis, known as “continuous venovenous hemodiafiltration” (CVVHDF) (Table 1).
Initiation of renal support
Approximately 70% of critically ill patients with severe AKI require RRT initiation, which represents an estimated 5% of all intensive care unit (ICU) admissions.1 The application of RRT represents a substantial escalation in the complexity of support.1 Yet, despite its extensive use in clinical practice, there remains no consensus on the optimal time and indications for RRT initiation.3,4 Indeed, surveillance has found marked variation in practice.5,6 The clinical decision regarding the time to initiate RRT is complex and can be influenced by numerous factors7 (Table 2).
There are several conventional “absolute” indications for RRT, whereby initiation would be considered “rescue” therapy in many circumstances (Table 3). These are not uncommonly encountered. Observational data show an estimated 50% of patients have their RRT started within 24 hr of ICU admission.8
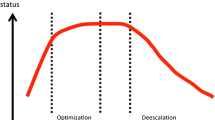
For patients without absolute indications, however, it remains uncertain whether “earlier” RRT initiation could translate into improved clinical outcomes. This question regarding the timing of RRT initiation has been evaluated in numerous observational studies and clinical trials, and the results of a pooled analysis of these data would imply that earlier initiation is associated with improved survival and renal recovery.8-15 Inferences from these data are limited, however, since most studies were small, single centre, retrospective, or secondary post-hoc analyses, and “early” and “late” RRT initiation were defined by dichotomizing around arbitrary thresholds of serum urea or urine output (UO). Importantly, many studies are not generalizable or applicable to present critical care environments. This relates, in part, to a paradigm shift in critical care to consider expanded indications for renal support, where initiation is not governed by absolute indications. Rather, RRT initiation integrates further aspects of an individual patient’s circumstances, such as relative onset and severity of AKI, existing renal reserve, non-renal organ dysfunction, and context-specific factors (Table 4). Recently, an algorithm that incorporates these features was proposed to aid in deciding when to initiate RRT while awaiting more definitive data from randomized trials7 (Figure).
Algorithm for RRT initiation in the adult critically ill patient (adapted from7 with permission). RRT = renal replacement therapy. 1. Absolute indications: serum urea ≥ 36 mmoL·L−1 or uremic complications; K+ ≥ 6 mmoL·L−1 and/or electrocardiogram abnormalities; Mg2+ ≥ 4 mmoL·L−1 and/or absent deep tendon reflexes; serum pH ≤ 7.15; urine output < 200 mL·12 hr−1 or anuria; diuretic-resistant organ edema (i.e., pulmonary edema). 2. Optimize resuscitation: Ensure intravascular volume repletion; adequate mean arterial pressure; adequate cardiac output; adequate oxygen carrying capacity. 3. Assess the patient: Evaluate acute kidney injury severity/trend; evaluate organ failure and illness severity/trend; assess response to initial resuscitation. 4. Are certain mitigating circumstances present? These include consideration of: diminished renal reserve; low probability of renal recovery; rapidly worsening acute kidney injury; rapidly worsening illness severity/organ failure; hypercatabolic state; refractory fluid overload/accumulation; refractory acidosis due to permissive hypercapnea; severe sepsis. 5. Are there potential non-renal indications? These may include: refractory fluid overload; refractory septic shock; acute liver failure; tumour lysis syndrome; severe electrolyte disturbance; dysthermia; myoglobinuric acute kidney injury; selected toxins
Discontinuation of renal support
There is limited data available regarding the ideal time to discontinue or “wean” patients from RRT. However, recent observational data have provided some pragmatic information to guide on this issue. In a secondary analysis of 529 critically ill patients receiving continuous renal replacement therapy (CRRT) from the BEST Kidney study, Uchino et al. reported that UO ≥ 426 mL·24 hr−1 preceding discontinuation and change in creatinine were the best predictors of weaning success-defined as not requiring CRRT re-initiation within seven days.16 However, the predictive ability of UO for successful RRT weaning was affected negatively by diuretic use. In a retrospective study of 304 postoperative patients receiving RRT, successful weaning from RRT-defined as RRT-free at 30 days-occurred in 30.9%.17 The following factors were independently associated with remaining RRT-free: age < 65 yr, shorter duration of RRT, lower sequential organ failure assessment (SOFA) score, and UO ≥ 100 mL·8 hr−1 on the day that RRT was discontinued. In view of these data, a pragmatic approach would be to wean RRT when spontaneous UO exceeds 400 mL·day−1 and/or when there is evidence of a declining SCr. Renal replacement therapy may then be discontinued without any specific weaning protocol. While not specifically supported by data, selected patients achieving only partial recovery may benefit from more prolonged RRT weaning, such as reduction in hemofiltration rate, reduced intermittent therapy, and/or isolated UF only.
Choice of RRT modality
Selection of the ideal RRT modality to support critically ill patients with AKI has long been debated.18 Several randomized trials have intended to establish the optimal RRT modality.19-28 Unfortunately, issues have been identified with these studies that potentially undermine their validity and, hence, weaken inferences that can be made. Specifically, several studies had limitations related to study design (i.e., exclusion of hemodynamically unstable patients, selection bias, no standardization of RRT dose or timing of initiation), conduct (i.e., improper randomization, differing baseline characteristics, high crossover rates), and quality (i.e., underpowered). Moreover, several systematic reviews have added uncertainty by reporting discordant conclusions.29-32
In general, perhaps due to these limitations, no overall differences in mortality or renal recovery were clearly established when pooled data were analyzed from these trials.29,31 However, two trials suggested greater complete recovery of kidney function for patients whose initial therapy was CRRT.22,26 This finding has recently been reinforced by observational data showing higher renal recovery to RRT independence for critically ill patients who initially received CRRT.33-35 Moreover, several trials have also shown a higher occurrence of hemodynamic intolerance in critically ill patients receiving IHD. These episodes of hemodynamic instability can result in an interruption in treatment, a need for fluid administration or an escalation in vasopressors, and they can compromise the intended goals of RRT (i.e., uremic control, volume homeostasis).19,21,27,36 Observational data have recently confirmed that achievement of fluid balance goals in critically ill patients with AKI is more likely for those prescribed CRRT rather than IHD.37 These data provide a compelling physiologic rationale for use of CRRT (and/or potentially SLED), at least initially, for critically ill patients characterized by severe AKI, high illness acuity, hemodynamic instability, and/or multi-organ organ dysfunction.
Finally, a retrospective study from a single centre model of RRT delivery proposed that the exclusive use of IHD rather than CRRT would translate into immediate cost savings. The proposal was based on estimated costing data and on the presumption of no survival advantage for either IHD or CRRT.38 However, this analysis assumed patients would receive only one type of therapy; whereas, in clinical practice, the RRT modality used is tailored to the specific clinical context and illness severity of the patient and could involve either CRRT or IHD over the course of an episode of critical illness.18 It remains important to use RRT that is the least resource intensive. However, realized cost differences between CRRT and IHD vary substantially due to different delivery models across regions.39 Moreover, the total costs of acute RRT are negligible relative to the costs of ICU/hospital admission associated with critical illness.
In summary, the debate regarding the RRT modality in critically ill patients with AKI that will optimize outcomes, reduce treatment-related complications, and conserve health resources has focused historically on the wrong issue. Instead, we contend that the issue to focus on should be the optimal time to prescribe a particular modality to meet the changing demands for a given patient. There is a wide spectrum of critically ill patients, and often their clinical course is not static. The ideal RRT modality must consider patient-specific (i.e., diagnosis, illness severity), clinician-specific (i.e., RRT prescribing service), and organizational factors (i.e., availability of RRT machines, nursing support).
Dose intensity of RRT
Determination of the optimal dose intensity for solute clearance for critically ill patients with AKI has long been a clinical priority. There has been a lack of consensus for what constitutes “optimal” intensity for translation into improved clinical outcomes. Early randomized trials clearly favoured a more intensive therapy40-42 whereas, more recent data have not shown a survival benefit with this approach.43,44 The source of this discrepancy is unclear; however, it may reflect differences in study design, in particular, the quality of reporting. Adequate reporting of quality indicators, including the method of randomization and allocation concealment, is a validated measure of the quality of trial conduct and is strongly related to internal validity. Earlier positive trials tended to be single-centre and lacked detailed descriptions of randomization and allocation concealment. Recently, two key studies have been published, i.e., the ATN Trial and the RENAL trial, that will inform practice due to their size, methodological rigor, multicentricity, and detailed data.36,45
The Department of Veterans Affairs/National Institutes of Health (VA/NIH) Acute Renal Failure Trial Network (ATN) study was a 27 centre, randomized clinical trial wherein 1,124 critically ill patients with AKI were enrolled and strategies providing either greater or lesser intensity of RRT were compared.36 In the more intensive strategy, IHD and SLED were provided daily (six days·week−1), and CVVHDF was provided at an effluent flow rate of 35 mL·kg−1·hr−1. In the less intensive strategy, IHD and SLED were provided every other day (three days·week−1), and CVVHDF was provided at an effluent flow rate of 20 mL·kg−1·hr−1. Renal support was provided as IHD when patients were hemodynamically stable and provided as either CVVHDF or SLED for hemodynamic instability. Within 60 days of randomization, 53.6% of patients in the more intensive arm had died compared with 51.6% of patients in the less intensive arm (odds ratio (OR) 1.09; 95% confidence interval (CI), 0.86-1.40; P = 0.47). There were no significant differences across all pre-specified subgroups, including sepsis. Renal recovery was not different between groups. Of the patients surviving to day 60, 74.6% in the more intensive arm were dialysis independent compared with 76.2% in the less intensive arm (P = 0.67). Only 15.7% and 16.4% of patients, respectively, were alive, dialysis independent, and discharged to home by day 60 (P = 0.75).
The Randomized Evaluation of Normal vs Augmented Level (RENAL) Replacement Therapy Study was a 35-centre randomized clinical trial of 1,508 critically ill patients with AKI wherein the effect of more intensive CVVHDF (40 mL·kg−1·hr−1) was compared with less intensive CVVHDF (20 mL·kg−1·hr−1) on 90-day all-cause mortality.45 Very few patients (< 10%) received IHD during the later phases of this trial. Mortality at day 90 was 44.7% in each group (OR 1.00; 95% CI, 0.81-1.23, P = 0.99). There were no significant differences in all pre-specified subgroups, including sepsis. Also, renal recovery was not different between groups (93.2% in the more intensive group vs 95.6% in the less intensive group; P = 0.14). A total of 49.8% and 51.6% of patients, respectively, were alive and dialysis independent by 90 days.
Both the ATN and RENAL trials found no added benefit in critically ill patients with AKI from a strategy of more intensive (high dose) RRT strategy compared with a less intensive RRT strategy. The more intensive strategy did not decrease mortality, accelerate recovery of kidney function, or alter the rate of non-renal organ failure. These findings do not imply that the dose of RRT is not important, but rather, the evidence would suggest there is no need to provide IHD for solute clearance more frequently than three times per week, so long as a target Kt/Vurea of 1.2-1.4 per treatment is achieved, and there is no need to provide CVVHDF with an effluent flow rate of > 20-25 mL·kg−1·hr−1, so long as time on therapy in maximized.
Fluid accumulation in AKI
Fluid balance is increasingly recognized as an important “biomarker” of critical illness.46 In a small retrospective study of 36 patients with septic shock, higher mortality was observed in those not achieving a negative fluid balance in at least one of the first three days after ICU admission.47 The impact of maintaining a neutral or negative fluid balance has been shown to improve outcomes in acute lung injury (ALI)48 pulmonary edema49 and is predictive of successful weaning from mechanical ventilation.50 In septic patients with AKI, continued resuscitation with additional fluid therapy did not lead to improvements in kidney function, but rather worsened gas exchange, despite apparent optimal hemodynamics, restoration of intravascular volume, and a high rate of diuretic use.51
Clinical studies in critically ill children with AKI have consistently identified fluid overload as an independent factor associated with mortality.52-56 Goldstein et al. evaluated 21 children with AKI and they found that a higher percent fluid overload (%FO) at the time of RRT initiation, controlling for illness severity, was independently associated with lower survival.54 This finding has been confirmed in additional studies in children with multi-organ failure.52,55,56 Recently, Sutherland et al. showed that risk of death increased by 3% for every 1% increase in %FO at RRT initiation.56 The formula used to calculate %FO was:
These data, at least in critically ill children, present a compelling argument for a potential survival benefit for earlier RRT initiation so as to prevent or attenuate fluid accumulation once initial goals of resuscitation have been accomplished.
Similar data in adult critically ill patients with septic AKI have indicated a negative effect of fluid accumulation on survival.57 In this study, a positive fluid balance (per L·24 hr−1) showed independent association with 60-day mortality (OR 1.21; 95% CI, 1.13-1.28; P < 0.001). While no data were available on fluid balance by timing of RRT initiation, patients receiving earlier RRT (< two days after ICU admission) had lower 60-day mortality (44.8% vs 64.6%, respectively; P < 0.01), despite greater illness severity and more oliguria. Recently, a secondary analysis of 542 critically ill patients with AKI from the PICARD study58 explored the association of fluid overload-defined as a %FO > 10% and mortality.37 Patients with fluid overload had higher illness severity; they were more likely postoperative, and they had lower serum creatinine and UO compared with patients who did not have fluid overload. Patients with fluid overload and AKI had significantly higher 60-day mortality (48% vs 35%, respectively; OR 3.1; 95% CI, 1.2-8.3). Moreover, in patients with severe AKI receiving RRT, the average fluid accumulation was significantly lower in survivors compared with non-survivors (8.8% vs 14.2%, respectively; P = 0.01) and the adjusted odds for death was higher for those with fluid overload (OR 2.1; 95% CI, 1.3-3.4).
These data, coupled with data from pediatric patients, provides a persuasive argument for the importance of close monitoring of fluid balance in critical illness, where obligatory fluid intake (i.e., medications, nutrition) may greatly exceed output (i.e., relative oliguria) leading to rapid fluid accumulation, particularly if compounded by AKI. To date, no specific randomized trial has assessed a strategy focused on attenuating fluid accumulation in AKI. However, randomized trials of conservative fluid management in ALI and in perioperative settings have found improved outcome, indirectly implying unnecessary fluid accumulation in AKI may also be an important and underappreciated determinant of outcome.
Drug dosing during renal support
Drug pharmacokinetics in AKI and critical illness are modified considerably due to altered bioavailability, reduced protein binding, increased volume of distribution, altered biotransformation, and reduced intrinsic clearance. Appropriate drug dosing is further complicated by a number of factors, including patients receiving multiple drugs that potentially interact with vital functions, lower tolerance for toxicity, evolving illness severity and organ dysfunction, and superimposed extracorporeal drug removal. The initiation of RRT can create challenges for estimating ideal drug dosing and removal; however, working knowledge of the principles influencing appropriate dosing adjustments is essential (Table 5). A number of drug classes may be affected, including (but not limited to) antimicrobials, antiepileptics, antiarrhythmics, immunosuppressives, vasoactives, and parenteral nutrition.
Importantly, RRT (more specifically CRRT) is most likely to enhance the clearance of drugs that are normally cleared by the kidney, are confined to the vascular compartment (i.e., low volume of distribution [Vd]), are not protein bound (large unbound fraction), and have a small molecular weight (below the cut-off or pore size of conventional hemofilters).
At the bedside, drug dosing for critically ill patients receiving CRRT should start by administration of a loading dose, dependent on the desired drug (plasma) and known Vd. Further maintenance doses should be adapted according to existing kidney function. Dose augmentation may be required if there is clinically important extracorporeal clearance (CL(EC)). There are proposed methods for estimating CL(EC) and appropriate drug dosing for patients receiving RRT, mostly focused on antimicrobials.59-62 One such method is based on calculation of the fractional CL(EC) of a drug related to total body clearance, accounting for CL from non-renal (NR) and residual renal function (R), represented by:
Any regional CL > 25%, whether EC or other, is likely clinically important and would necessitate dose adjustment.63
In general, there are several additional pragmatic steps for drug dosing in patients receiving CRRT. The first recommendation would be to consult the literature for existing data for a specific drug. While the literature is expanding, it is important to recognize that many studies are relatively small and show vast heterogeneity for methods of RRT application (i.e. mode, filter type, blood flow rate, UF rate).64 This variability may limit their generalizability; however, it may provide a starting point to guide drug dosing. Second, for drugs that have primary renal clearance, a bedside estimate of total creatinine clearance (sum of CL (EC) + CL(Cr)) can be performed to guide dosing, assuming no important drug secretion or reabsorption. The third recommendation, particularly with drugs with a narrow therapeutic index, is to utilize therapeutic drug monitoring (i.e., dilantin, vancomycin, aminoglycosides). Fourth, several drug classes may be administered based on their observed clinical response, as with sedatives, analgesics, or vasoactive medications. Finally, considering the complexity of drug dosing in these settings, the importance of integrating a critical care-specific pharmacist cannot be over emphasized. Drug dosing during RRT is complex and critical illness can be dynamic. Accordingly, dosing regimens should be individualized taking into consideration the aforementioned factors.
Extracorporeal blood purification in sepsis
For decades, there has been academic interest in the potential role of extracorporeal blood purification (EBP) in critically ill patients with severe sepsis/septic shock and AKI. There are plausible hypotheses to explain why EBP could improve outcomes in these patients. The “Peak Concentration” hypothesis is the concept of immuno-modulation and restoration of immuno-homeostasis through the non-selective reduction in the peaks of both pro- and anti-inflammatory mediators through EBP.65 Removal of these inflammatory mediators along with endotoxin from plasma could occur through high-volume hemofiltration (HVHF), UF using high flux and/or high-cutoff hemofilters, or through membrane adsorption with hemoperfusion or specialized hemofilters containing sorbents.65,66 For example, the addition of polycations to hemofilter membranes has been shown to significantly improve the adsorptive capacity of the hemofilters for inflammatory mediators and endotoxin.67
High-volume hemofiltration
High-volume hemofiltration has been used in critically ill patients with AKI, septic shock, septic AKI, and rhabdomyolysis. High-volume hemofiltration is generally defined as total effluent rates (UF and dialysate) exceeding 45 mL·kg−1·hr−1.40 In a subgroup analysis of the landmark study by Ronco et al., improvement in survival was found for septic patients randomized to HVHF (i.e., 45 mL·kg−1·hr−1 vs 35 or 20 mL·kg−1·hr−1). This subgroup represented only 12% of those enrolled; however, it generated considerable interest in HVHF as a novel therapy. In experimental models of enteric ischemia/reperfusion and septic shock, HVHF has been shown to improve hemodynamic parameters, including cardiac output, mean arterial pressure, and left ventricular stroke work, in addition to significantly reducing endotoxin levels.67,68 Numerous small clinical studies have applied HVHF to septic patients with and without AKI at doses in the range of 45-100 mL·kg−1·hr−1 and by variable methods, including continuously or as pulse/intermittent therapy (4-12 hr) followed by conventional CRRT.69-75 While these studies have generally been small, single-centre, and uncontrolled or crossover trials, results have consistently shown improved hemodynamics, reduced need for vasopressors, and better than expected survival (based on standardized mortality by illness severity scores). However, based on available data, we contend that HVHF should not be used routinely in critically ill patients with septic AKI, pending results of the “hIgh VOlume in Intensive caRE” (IVOIRE) trial. This is due to the uncertainly of the currently available data and several factors indicating that HVHF is resource and labour intensive, is technically challenging, and has limited data on safety/adverse effects (i.e,. excessive clearance of antimicrobials; nutrition). The IVOIRE trial is a multicentre randomized trial evaluating the impact of early HVHF (70 mL·kg−1·hr−1 for 96 hr) compared with standard-of-care (35 mL·kg−1·hr−1) on 28-day mortality in critically ill septic shock patients with AKI.72 This duration corresponds to a critical period of septic shock during which therapeutic interventions are likely to have the greatest impact on survival. The trial was recently completed and will inform on the safety, tolerance, and efficacy of this intervention.
High-cutoff hemofiltration
An additional EBP therapy in sepsis includes the use of high molecular weight cutoff hemofilters (> 50-60 kDa).76-79 These specialized hemofilters have greater porosity and are associated with significantly greater clearance of inflammatory mediators and cytokines and restoration of immune-homeostasis, both in vitro and in vivo, when compared with conventional hemofilters. There is an ongoing phase II randomized controlled trial of these hemofilters.
Polymyxin-B (PMX-B) hemoperfusion
Another approach has been to use an endotoxin binding column to attenuate the effect of endotoxemia in selected critically ill patients. Recently, the Early Use of Polymyxin B Hemoperfusion in Abdominal Sepsis (EUPHAS) study, a multicentre randomized trial of 64 patients receiving emergency surgery for intra-abdominal sepsis, compared treatment with a PMX-B (two sessions of PMX-B hemoperfusion) with conventional support postoperatively.80 The trial rationale was based on evidence that PMX-B avidly binds endotoxin and preliminary data showing benefit.81 The use of PMX-B hemoperfusion was associated with improvements in systemic hemodynamics and SOFA score at 72 hr, along with a significant reduction in 28-day mortality (32% vs 53%, respectively; unadjusted OR 0.43; 95% CI, 0.20-0.94). Additional confirmatory trials are in progress; however, these data are promising for early use of PMX-B hemoperfusion in patients with intra-abdominal sepsis.
Hemofiltration in rhabdomyolysis and myoglobinuria AKI
The use of HVHF has also been evaluated in rhabdomyolysis to prevent myoglobinuric AKI. The rationale is for early clearance of circulating myoglobin prior to overt kidney failure. Several experimental studies82,83 and small clinical trials84-89 have shown clearance rates of 10-25% of circulating myoglobin using UF rates of 2-3 L·hr−1 and conventional hemofilters. A recent small randomized trial of HVHF (75 mL·kg−1·hr−1) in patients at high risk for myoglobinuric AKI90 found a relatively low sieving coefficient for myoglobin during the first hour (0.23), which decreased to 0.10 over the next 12 hr. This finding implied that there was considerable myoglobin adsorption to the hemofilter that rapidly diminished its efficiency.91 However, none of the five patients receiving HVHF required continued RRT for AKI, compared with two of three patients in the non-HVHF group. In a case report of severe rhabdomyolysis, the use of a higher cutoff hemofilter (100 kDa) was shown to improve clearance of myoglobin (sieving coefficient 0.72) to a greater extent when compared with a conventional hemofilter.92 Similar to HVHF in sepsis, the prophylactic use of HVHF for patients with rhabdomyolysis at risk for myoglobinuric AKI should not be performed routinely, pending data from randomized trials. However, in patients with established AKI who are not responsive to initial resuscitation, early support with RRT should be initiated.
Extracorporeal liver support
Extracorporeal liver support technologies generally utilize albumin as a binding and scavenging molecule for the non-specific removal of toxins.93 Potential toxins removed include conjugated bilirubin, ammonia, bile acids, phenols, tryptophans, nitric oxide, and benzodiazepine-like substances. These liver support platforms are indicated in patients with acute or decompensated chronic liver failure (CLF) characterized by refractory hyperbilirubinemia, hepato-renal syndrome (HRS), and/or hepatic encephalopathy to provide a bridge for liver transplantation or to allow for liver regeneration. The molecular adsorbent recirculating system (MARS) consists of two parallel circuits containing an albumin hemofilter, a standard hemofilter, an activated charcoal adsorber, and anion exchanger filters. Two small trials in CLF patients with HRS found MARS treatment was associated with improvements in hemodynamics, biochemical profile, and hepatic encephalopathy.32,94,95 Single pass albumin dialysis is an alternative method for albumin dialysis whereby a conventional CRRT circuit is utilized and a custom fluid containing 5% albumin is used as a countercurrent dialysate. There are only case reports and series describing this form of liver support.96-100 Fractionated plasma separation and adsorption (Prometheus) is a modified form of liver support where plasma is separated across a very high cutoff membrane (250 kDa) that is permeable to albumin, pumped through a series of adsorptive columns, and re-constituted.93 Small clinical studies have also shown this modality to improve hemodynamics and biochemical parameters in acute or decompensated CLF.101,102 None of these liver support modalities have shown a clear survival advantage either to native liver recovery or to transplant, and they are limited by their complexity and need for specialized resources. Further clinical trials evaluating their effectiveness are ongoing.
The management of acute or CLF patients during a prolonged liver transplantation (LT) can be technically complex.103 The intraoperative course is associated with alterations to systemic hemodynamics, metabolic control, and coagulation status that may require the aggressive administration of fluid therapy, blood products, and clotting factors.104 Moreover, AKI is common in the preoperative setting and generally predicts a more complicated course and a less favourable postoperative outcome.105-112 Anesthetists may already be confronted with intraoperative challenges in a sick liver failure patient (i.e., cerebral edema) that may be compounded in those with oliguric AKI (i.e., metabolic acidosis, hyperkalemia, azotemia, and volume overload).113-115 There is physiologic rationale, although limited data, to support the intraoperative use of CRRT during LT to provide metabolic, acid-base, and volume homeostasis.113,116,117 In a recent series of 41 patients receiving LT, all with preoperative AKI and high illness acuity (median model for end-stage liver disease score 38), intraoperative CRRT was found to be a safe and feasible adjuvant supportive therapy.118 However, these data have significant limitations, and further confirmatory investigations are needed prior to there being a recommendation for routine use of intraoperative CRRT in selected at-risk patients.
Hemofiltration in patients with sodium disorders
Serum sodium (Na+) disorders, such as severe hyponatremia or hypernatremia, are surprisingly common in sick hospitalized patients and have been independently associated with less favourable outcomes.119-121 Many patients are critically ill perioperatively, have concomitant AKI, and are likely to receive renal support for indications beyond disorders in serum Na+. In these patients, overtly rapid Na+ correction needs to be avoided; however, during RRT, Na+ has the potential to equilibrate rapidly with the [Na+] in replacement fluid or dialysate. Below is a brief discussion on [Na+] adjustment in replacement/dialysate fluid during RRT to prevent complications related to rapid serum Na+ shifts.122
While it is possible to manufacture replacement/dialysate fluid on site for individual patients, most centres use commercially available fluids that have a final [Na+] of 140 mEq·L−1. CRRT using replacement/dialysate fluids containing this [Na+] may place both hyponatremic and hypernatremic patients at risk for rapid serum [Na+] corrections and predispose to osmotic demyelination or cerebral edema.
There are several pragmatic methods for altering CRRT prescription to allow for an acceptable rate of serum [Na+] correction. The first is simply to reduce the efficiency of the modality by decreasing the total effluent rate, for example, from a standard 25 mL·kg−1·hr−1 to 15-20 mL·kg−1·hr−1. However, this approach may be limited by the need for increased solute clearance or treatment of severe metabolic acidosis. The second (and more effective) approach is to alter the [Na+] of the replacement/dialysate fluids. This is accomplished either by custom solution or by altering commercially available solutions by addition of either hypertonic saline or water. The third approach is to administer concomitantly an intravenous infusion of either hypertonic or hypotonic fluid at a calculated rate to produce similar results to customizing the replacement/dialysis fluids. Whichever approach is employed, the most important aspect of therapy is to ensure frequent monitoring of serum [Na+], as there is no accurate method to predict the combined effect of CRRT and these approaches on the rate of change in serum [Na+].
The risk of osmotic demyelination in patients with chronic hyponatremia undergoing CRRT may be partially mitigated by a concomitant decrease in serum73 during the procedure. However, it is vital to reduce the [Na+] in the replacement/dialysate fluid to prevent this potentially fatal disorder. There are essentially two methods to accomplish this. The first is to add water (D5W) to the commercial replacement/dialysis fluid bag (Table 6). The second perhaps simpler solution is to administer separately an infusion of D5W that is completely removed with UF, thereby effectively diluting the replacement/dialysis fluid [Na+]. For example, if the total effluent flow rate is 2,000 mL·hr−1 with D5W infusing at 200 mL·hr−1 and removed via UF, the effective [Na+] in the replacement/dialysate fluid would be reduced to approximately 127 mEq·L−1. However, it is also important to recognize that the common practice of adding extra bicarbonate to replacement/dialysis fluids will increase [Na+] by roughly 8.5 mEq·L−1 for each 50 mEq of NaHCO3 added to a 5,000 mL bag.
The risk of cerebral edema in hypernatremic patients undergoing CRRT with relatively hypotonic replacement/dialysate fluid is increased by the concomitant decrease in serum [Na +].73 This risk can be mitigated by addition of small volumes of hypertonic saline to increase the [Na+] of commercial fluids (Table 7). In patients with severe metabolic acidosis, added Na+ can be added as NaHCO3, with the expected increase in [Na+] as mentioned above. Alternatively, each 100 mL of 3% NaCl solution added to a 5,000 mL bag will correspond to a 7.3 mEq·L−1 increase in [Na+].
Conclusions
Acute kidney injury (AKI) is a common clinical problem in sick hospitalized patients, and many ultimately require extracorporeal support with RRT. These patients are at high risk for long-term morbidity and death. There have been considerable technological innovations in the methods and techniques for RRT. These have greatly expanded our capacity to provide both renal and non-renal life-sustaining organ support. However, there are still several fundamental clinical questions that remain to be answered. These include issues regarding the ideal time to initiate/discontinue RRT, fluid accumulation in AKI, the role of HVHF or other blood purification techniques in sepsis, and extracorporeal support for combined liver-kidney failure. We anticipate that this field will continue to expand to promote research and innovation, hopefully for the benefit of sick critically ill patients.
References
Uchino S, Kellum JA, Bellomo R, et al. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA 2005; 294: 813-8.
Ronco C, Ricci Z. Renal replacement therapies: physiological review. Intensive Care Med 2008; 34: 2139-46.
Bagshaw SM, Gibney RT. Ideal determinants for the initiation of renal replacement therapy: timing, metabolic threshold or fluid balance? Acta Clin Belg Suppl 2007; (2): 357-61.
Gibney N, Hoste E, Burdmann EA, et al. Timing of initiation and discontinuation of renal replacement therapy in AKI: unanswered key questions. Clin J Am Soc Nephrol 2008; 3: 876-80.
Overberger P, Pesacreta M, Palevsky PM, VA/NIH Acute Renal Failure Trial Network. Management of renal replacement therapy in acute kidney injury: a survey of practitioner prescribing practices. Clin J Am Soc Nephrol 2007; 2: 623-30.
Ricci Z, Ronco C, D’Amico G, et al. Practice patterns in the management of acute renal failure in the critically ill patient: an international survey. Nephrol Dial Transplant 2006; 21: 690-6.
Bagshaw SM, Cruz DN, Gibney RT, Ronco C. A proposed algorithm for initiation of renal replacement therapy in adult critically ill patients. Crit Care 2009; 13: 317.
Bagshaw SM, Uchino S, Bellomo R, et al. Timing of renal replacement therapy and clinical outcomes in critically ill patients with severe acute kidney injury. J Crit Care 2009; 24: 129-40.
Gettings LG, Reynolds HN, Scalea T. Outcome in post-traumatic acute renal failure when continuous renal replacement therapy is applied early vs. late. Intensive Care Med 1999; 25: 805-13.
Kresse S, Schlee H, Deuber HJ, Koall W, Osten B. Influence of renal replacement therapy on outcome of patients with acute renal failure. Kidney Int Suppl 1999; (72): S75-8.
Liu KD, Himmelfarb J, Paganini EP, et al. Timing of initiation of dialysis in critically ill patients with acute kidney injury. Clin J Am Soc Nephrol 2006; 1: 915-9.
Ostermann M, Chang RW. Correlation between parameters at initiation of renal replacement therapy and outcome in patients with acute kidney injury. Crit Care 2009; 13: R175.
Shiao CC, Wu VC, Li WY, et al. Late initiation of renal replacement therapy is associated with worse outcomes in acute kidney injury after major abdominal surgery. Crit Care 2009; 13: R171.
Splendiani G, Mazzarella V, Cipriani S, Zazzaro D, Casciani CU. Continuous renal replacement therapy: our experience in intensive care unit. Ren Fail 2001; 23: 259-64.
Seabra VF, Balk EM, Liangos O, Sosa MA, Cendoroglo M, Jaber BL. Timing of renal replacement therapy initiation in acute renal failure: a meta-analysis. Am J Kidney Dis 2008; 52: 272-84.
Uchino S, Bellomo R, Morimatsu H, et al. Discontinuation of continuous renal replacement therapy: a post hoc analysis of a prospective multicenter observational study. Crit Care Med 2009; 37: 2576-82.
Wu VC, Ko WJ, Chang HW, et al. Risk factors of early redialysis after weaning from postoperative acute renal replacement therapy. Intensive Care Med 2008; 34: 101-8.
Ronco C, Bagshaw SM, Gibney RT, Bellomo R. Outcome comparisons of intermittent and continuous therapies in acute kidney injury: what do they mean? Int J Artif Organs 2008; 31: 213-20.
Augustine JJ, Sandy D, Seifert TH, Paganini EP. A randomized controlled trial comparing intermittent with continuous dialysis in patients with ARF. Am J Kidney Dis 2004; 44: 1000-7.
Gasparovic V, Filipovic-Grcic I, Merkler M, Pisl Z. Continuous renal replacement therapy (CRRT) or intermittent hemodialysis (IHD)–what is the procedure of choice in critically ill patients? Ren Fail 2003; 25: 855-62.
John S, Griesbach D, Baumgartel M, Weihprecht H, Schmieder RE, Geiger H. Effects of continuous haemofiltration vs intermittent haemodialysis on systemic haemodynamics and splanchnic regional perfusion in septic shock patients: a prospective, randomized clinical trial. Nephrol Dial Transplant 2001; 16: 320-7.
Mehta RL, McDonald B, Gabbai FB, et al. A randomized clinical trial of continuous versus intermittent dialysis for acute renal failure. Kidney Int 2001; 60: 1154-63.
Misset B, Timsit JF, Chevret S, Renaud B, Tamion F, Carlet J. A randomized cross-over comparison of the hemodynamic response to intermittent hemodialysis and continuous hemofiltration in ICU patients with acute renal failure. Intensive Care Med 1996; 22: 742-6.
Simpson K, Allison ME. Dialysis and acute renal failure: can mortality be improved? Nephrol Dial Transplant 1993; 8: 947 (abstract).
Davenport A, Will EJ, Davison AM. Continuous vs. intermittent forms of haemofiltration and/or dialysis in the management of acute renal failure in patients with defective cerebral autoregulation at risk of cerebral oedema. Contrib Nephrol 1991; 93: 225-33.
Uehlinger DE, Jakob SM, Ferrari P, et al. Comparison of continuous and intermittent renal replacement therapy for acute renal failure. Nephrol Dial Transplant 2005; 20: 1630-7.
Vinsonneau C, Camus C, Combes A, et al. Continuous venovenous haemodiafiltration versus intermittent haemodialysis for acute renal failure in patients with multiple-organ dysfunction syndrome: a multicentre randomised trial. Lancet 2006; 368: 379-85.
Lins RL, Elseviers MM, Van der Niepen P, et al. Intermittent versus continuous renal replacement therapy for acute kidney injury patients admitted to the intensive care unit: results of a randomized clinical trial. Nephrol Dial Transplant 2009; 24: 512-8.
Bagshaw SM, Berthiaume LR, Delaney A, Bellomo R. Continuous versus intermittent renal replacement therapy for critically ill patients with acute kidney injury: a meta-analysis. Crit Care Med 2008; 36: 610-7.
Kellum JA, Angus DC, Johnson JP, et al. Continuous versus intermittent renal replacement therapy: a meta-analysis. Intensive Care Med 2002; 28: 29-37.
Pannu N, Klarenbach S, Wiebe N, Manns B, Tonelli M, Alberta Kidney Disease Network. Renal replacement therapy in patients with acute renal failure: a systematic review. JAMA 2008; 299: 793-805.
Tonelli M, Manns B, Feller-Kopman D. Acute renal failure in the intensive care unit: a systematic review of the impact of dialytic modality on mortality and renal recovery. Am J Kidney Dis 2002; 40: 875-85.
Jacka MJ, Ivancinova X, Gibney RT. Continuous renal replacement therapy improves renal recovery from acute renal failure. Can J Anesth 2005; 52: 327-32.
Bell M, SWING, Granath F, Schon S, Ekbom A, Martling CR. Continuous renal replacement therapy is associated with less chronic renal failure than intermittent haemodialysis after acute renal failure. Intensive Care Med 2007; 33: 773-80.
Uchino S, Bellomo R, Kellum JA, et al. Patient and kidney survival by dialysis modality in critically ill patients with acute kidney injury. Int J Artif Organs 2007; 30: 281-92.
VA/NIH Acute Renal Failure Trial Network, Palevsky PM, Zhang JH, et al. Intensity of renal support in critically ill patients with acute kidney injury. N Engl J Med 2008; 359: 7-20.
Bouchard J, Soroko SB, Chertow GM, et al. Fluid accumulation, survival and recovery of kidney function in critically ill patients with acute kidney injury. Kidney Int 2009; 76: 422-7.
Manns B, Doig CJ, Lee H, et al. Cost of acute renal failure requiring dialysis in the intensive care unit: clinical and resource implications of renal recovery. Crit Care Med 2003; 31: 449-55.
Srisawat N, Lawsin L, Uchino S, Bellomo R, Kellum JA, BEST Kidney Investigators. Cost of acute renal replacement therapy in the intensive care unit: results from The Beginning, Ending Supportive Therapy for the Kidney (BEST Kidney) study. Crit Care 2010; 14: R46.
Ronco C, Bellomo R, Homel P, et al. Effects of different doses in continuous veno-venous haemofiltration on outcomes of acute renal failure: a prospective randomised trial. Lancet 2000; 356: 26-30.
Saudan P, Niederberger M, De Seigneux S, et al. Adding a dialysis dose to continuous hemofiltration increases survival in patients with acute renal failure. Kidney Int 2006; 70: 1312-7.
Schiffl H. Daily haemodialysis for acute renal failure. Curr Opin Nephrol Hypertens 2002; 11: 589-92.
Faulhaber-Walter R, Hafer C, Jahr N, et al. The Hannover Dialysis Outcome study: comparison of standard versus intensified extended dialysis for treatment of patients with acute kidney injury in the intensive care unit. Nephrol Dial Transplant 2009; 24: 2179-86.
Tolwani AJ, Campbell RC, Stofan BS, Lai KR, Oster RA, Wille KM. Standard versus high-dose CVVHDF for ICU-related acute renal failure. J Am Soc Nephrol 2008; 19: 1233-8.
RENAL Replacement Therapy Study Investigators, Bellomo R, Cass A. et al. Intensity of continuous renal-replacement therapy in critically ill patients. N Engl J Med 2009; 361: 1627-38.
Bagshaw SM, Brophy PD, Cruz D, Ronco C. Fluid balance as a biomarker: impact of fluid overload on outcome in critically ill patients with acute kidney injury. Crit Care 2008; 12: 169.
Alsous F, Khamiees M, DeGirolamo A, Amoateng-Adjepong Y, Manthous CA. Negative fluid balance predicts survival in patients with septic shock: a retrospective pilot study. Chest 2000; 117: 1749-54.
National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network, Wiedemann HP, Wheeler AP, et al. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med 2006; 354: 2564-75.
Sakr Y, Vincent JL, Reinhart K, et al. High tidal volume and positive fluid balance are associated with worse outcome in acute lung injury. Chest 2005; 128: 3098-108.
Upadya A, Tilluckdharry L, Muralidharan V, Amoateng-Adjepong Y, Manthous CA. Fluid balance and weaning outcomes. Intensive Care Med 2005; 31: 1643-7.
Van Biesen W, Yegenaga I, Vanholder R, et al. Relationship between fluid status and its management on acute renal failure (ARF) in intensive care unit (ICU) patients with sepsis: a prospective analysis. J Nephrol 2005; 18: 54-60.
Foland JA, Fortenberry JD, Warshaw BL, et al. Fluid overload before continuous hemofiltration and survival in critically ill children: a retrospective analysis. Crit Care Med 2004; 32: 1771-6.
Gillespie RS, Seidel K, Symons JM. Effect of fluid overload and dose of replacement fluid on survival in hemofiltration. Pediatr Nephrol 2004; 19: 1394-9.
Goldstein SL, Currier H, Graf C, Cosio CC, Brewer ED, Sachdeva R. Outcome in children receiving continuous venovenous hemofiltration. Pediatrics 2001; 107: 1309-12.
Goldstein SL, Somers MJ, Baum MA, et al. Pediatric patients with multi-organ dysfunction syndrome receiving continuous renal replacement therapy. Kidney Int 2005; 67: 653-8.
Sutherland SM, Zappitelli M, Alexander SR, et al. Fluid overload and mortality in children receiving continuous renal replacement therapy: the prospective pediatric continuous renal replacement therapy registry. Am J Kidney Dis 2010; 55: 316-25.
Payen D, de Pont AC, Sakr Y, et al. A positive fluid balance is associated with a worse outcome in patients with acute renal failure. Crit Care 2008; 12: R74.
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P, Acute Dialysis Quality Initiative workgroup. Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 2004; 8: R204-12.
Choi G, Gomersall CD, Tian Q, Joynt GM, Freebairn R, Lipman J. Principles of antibacterial dosing in continuous renal replacement therapy. Crit Care Med 2009; 37: 2268-82.
Li AM, Gomersall CD, Choi G, Tian Q, Joynt GM, Lipman J. A systematic review of antibiotic dosing regimens for septic patients receiving continuous renal replacement therapy: do current studies supply sufficient data? J Antimicrob Chemother 2009; 64: 929-37.
Pea F, Viale P, Pavan F, Furlanut M. Pharmacokinetic considerations for antimicrobial therapy in patients receiving renal replacement therapy. Clin Pharmacokinet 2007; 46: 997-1038.
Trotman RL, Williamson JC, Shoemaker DM, Salzer WL. Antibiotic dosing in critically ill adult patients receiving continuous renal replacement therapy. Clin Infect Dis 2005; 41: 1159-66.
Schetz M. Drug dosing in continuous renal replacement therapy: general rules. Curr Opin Crit Care 2007; 13: 645-51.
Mueller BA, Pasko DA, Sowinski KM. Higher renal replacement therapy dose delivery influences on drug therapy. Artif Organs 2003; 27: 808-14.
Ronco C, Tetta C, Mariano F, et al. Interpreting the mechanisms of continuous renal replacement therapy in sepsis: the peak concentration hypothesis. Artif Organs 2003; 27: 792-801.
Joannidis M. Continuous renal replacement therapy in sepsis and multisystem organ failure. Semin Dial 2009; 22: 160-4.
Rimmele T, Assadi A, Cattenoz M, et al. High-volume haemofiltration with a new haemofiltration membrane having enhanced adsorption properties in septic pigs. Nephrol Dial Transplant 2009; 24: 421-7.
Grootendorst AF, van Bommel EF, van Leengoed LA, Nabuurs M, Bouman CS, Groeneveld AB. High volume hemofiltration improves hemodynamics and survival of pigs exposed to gut ischemia and reperfusion. Shock 1994; 2: 72-8.
Boussekey N, Chiche A, Faure K, et al. A pilot randomized study comparing high and low volume hemofiltration on vasopressor use in septic shock. Intensive Care Med 2008; 34: 1646-53.
Cole L, Bellomo R, Journois D, Davenport P, Baldwin I, Tipping P. High-volume haemofiltration in human septic shock. Intensive Care Med 2001; 27: 978-86.
Cornejo R, Downey P, Castro R, et al. High-volume hemofiltration as salvage therapy in severe hyperdynamic septic shock. Intensive Care Med 2006; 32: 713-22.
Honore PM, Jamez J, Wauthier M, et al. Prospective evaluation of short-term, high-volume isovolemic hemofiltration on the hemodynamic course and outcome in patients with intractable circulatory failure resulting from septic shock. Crit Care Med 2000; 28: 3581-7.
Joannes-Boyau O, Rapaport S, Bazin R, Fleureau C, Janvier G. Impact of high volume hemofiltration on hemodynamic disturbance and outcome during septic shock. ASAIO J 2004; 50: 102-9.
Lonnemann G, Floege J, Kliem V, Brunkhorst R, Koch KM. Extended daily veno-venous high-flux haemodialysis in patients with acute renal failure and multiple organ dysfunction syndrome using a single path batch dialysis system. Nephrol Dial Transplant 2000; 15: 1189-93.
Oudemans-van Straaten HM, Bosman RJ, van der Spoel JI, Zandstra DF. Outcome of critically ill patients treated with intermittent high-volume haemofiltration: a prospective cohort analysis. Intensive Care Med 1999; 25: 814-21.
Haase M, Bellomo R, Morgera S, Baldwin I, Boyce N. High cut-off point membranes in septic acute renal failure: a systematic review. Int J Artif Organs 2007; 30: 1031-41.
Morgera S, Haase M, Rocktaschel J, et al. High permeability haemofiltration improves peripheral blood mononuclear cell proliferation in septic patients with acute renal failure. Nephrol Dial Transplant 2003; 18: 2570-6.
Morgera S, Klonower D, Rocktaschel J, et al. TNF-alpha elimination with high cut-off haemofilters: a feasible clinical modality for septic patients? Nephrol Dial Transplant 2003; 18: 1361-9.
Morgera S, Rocktaschel J, Haase M, et al. Intermittent high permeability hemofiltration in septic patients with acute renal failure. Intensive Care Med 2003; 29: 1989-95.
Cruz DN, Antonelli M, Fumagalli R, et al. Early use of polymyxin B hemoperfusion in abdominal septic shock: the EUPHAS randomized controlled trial. JAMA 2009; 301: 2445-52.
Cruz DN, Perazella MA, Bellomo R, et al. Effectiveness of polymyxin B-immobilized fiber column in sepsis: a systematic review. Crit Care 2007; 11: R47.
Nicolau DP, Feng YJ, Wu AH, Bernstein SP, Nightingale CH. Evaluation of myoglobin clearance during continuous hemofiltration in a swine model of acute renal failure. Int J Artif Organs 1996; 19: 578-81.
Nicolau D, Feng YS, Wu AH, Bernstein SP, Nightingale CH. Myoglobin clearance during continuous veno-venous hemofiltration with or without dialysis. Int J Artif Organs 1998; 21: 205-9.
Winterberg B, Ramme K, Tenschert W, et al. Hemofiltration in myoglobinuric acute renal failure. Int J Artif Organs 1990; 13: 113-6.
Berns JS, Cohen RM, Rudnick MR. Removal of myoglobin by CAVH-D in traumatic rhabdomyolysis. Am J Nephrol 1991; 11: 73.
Bellomo R, Daskalakis M, Parkin G, Boyce N. Myoglobin clearance during acute continuous hemodiafiltration. Intensive Care Med 1991; 17: 509.
Splendiani G, Mazzarella V, Cipriani S, Pollicita S, Rodio F, Casciani CU. Dialytic treatment of rhabdomyolysis-induced acute renal failure: our experience. Ren Fail 2001; 23: 183-91.
Amyot SL, Leblanc M, Thibeault Y, Geadah D, Cardinal J. Myoglobin clearance and removal during continuous venovenous hemofiltration. Intensive Care Med 1999; 25: 1169-72.
Maccario M, Fumagalli C, Dottori V, et al. Rhabdomyolytic acute renal failure in cardiac surgery. A clinical case. Minerva Anestesiol 1995; 61: 397-400.
Brown CV, Rhee P, Chan L, Evans K, Demetriades D, Velmahos GC. Preventing renal failure in patients with rhabdomyolysis: do bicarbonate and mannitol make a difference? J Trauma 2004; 56: 1191-6.
Kutsiogiannis DJ. A pilot randomized controlled trial of high-volume hemofiltration in rhabdomyolysis. Int J Art Organ 2008; 31: 593 (abstract).
Naka T, Jones D, Baldwin I, et al. Myoglobin clearance by super high-flux hemofiltration in a case of severe rhabdomyolysis: a case report. Crit Care 2005; 9: R90-5.
Karvellas CJ, Gibney N, Kutsogiannis D, Wendon J, Bain VG. Bench-to-bedside review: current evidence for extracorporeal albumin dialysis systems in liver failure. Crit Care 2007; 11: 215.
Jalan R, Sen S, Steiner C, Kapoor D, Alisa A, Williams R. Extracorporeal liver support with molecular adsorbents recirculating system in patients with severe acute alcoholic hepatitis. J Hepatol 2003; 38: 24-31.
Mitzner SR, Stange J, Klammt S, et al. Improvement of hepatorenal syndrome with extracorporeal albumin dialysis MARS: results of a prospective, randomized, controlled clinical trial. Liver Transpl 2000; 6: 277-86.
Karvellas CJ, Bagshaw SM, McDermid RC, Stollery DE, Bain VG, Gibney RT. A case-control study of single-pass albumin dialysis for acetaminophen-induced acute liver failure. Blood Purif 2009; 28: 151-8.
Karvellas CJ, Bagshaw SM, McDermid RC, Stollery DE, Gibney RT. Acetaminophen-induced acute liver failure treated with single-pass albumin dialysis: report of a case. Int J Artif Organs 2008; 31: 450-5.
Collins KL, Roberts EA, Adeli K, Bohn D, Harvey EA. Single pass albumin dialysis (SPAD) in fulminant Wilsonian liver failure: a case report. Pediatr Nephrol 2008; 23: 1013-6.
Rahman E, Al Suwaida AK, Askar A. Single pass albumin dialysis in hepatorenal syndrome. Saudi J Kidney Dis Transpl 2008; 19: 479-84.
Boonsrirat U, Tiranathanagul K, Srisawat N, et al. Effective bilirubin reduction by single-pass albumin dialysis in liver failure. Artif Organs 2009; 33: 648-53.
Grodzicki M, Kotulski M, Leonowicz D, Zieniewicz K, Krawczyk M. Results of treatment of acute liver failure patients with use of the Prometheus FPSA system. Transplant Proc 2009; 41: 3079-81.
Oppert M, Rademacher S, Petrasch K, Jorres A. Extracorporeal liver support therapy with Prometheus in patients with liver failure in the intensive care unit. Ther Apher Dial 2009; 13: 426-30.
Wiklund RA. Preoperative preparation of patients with advanced liver disease. Crit Care Med 2004; 32: S106-15.
Rettke SR, Janossy TA, Chantigian RC, et al. Hemodynamic and metabolic changes in hepatic transplantation. Mayo Clin Proc 1989; 64: 232-40.
Bilbao I, Charco R, Balsells J, et al. Risk factors for acute renal failure requiring dialysis after liver transplantation. Clin Transplant 1998; 12: 123-9.
Brown RS Jr, Lombardero M, Lake JR. Outcome of patients with renal insufficiency undergoing liver or liver-kidney transplantation. Transplantation 1996; 62: 1788-93.
Contreras G, Garces G, Quartin AA, et al. An epidemiologic study of early renal replacement therapy after orthotopic liver transplantation. J Am Soc Nephrol 2002; 13: 228-33.
Lafayette RA, Pare G, Schmid CH, King AJ, Rohrer RJ, Nasraway SA. Pretransplant renal dysfunction predicts poorer outcome in liver transplantation. Clin Nephrol 1997; 48: 159-64.
Lutkes P, Lutz J, Loock J, et al. Continuous venovenous hemodialysis treatment in critically ill patients after liver transplantation. Kidney Int Suppl 1999; (72): S71-4.
Naka T, Wan L, Bellomo R, et al. Kidney failure associated with liver transplantation or liver failure: the impact of continuous veno-venous hemofiltration. Int J Artif Organs 2004; 27: 949-55.
Paramesh AS, Roayaie S, Doan Y, et al. Post-liver transplant acute renal failure: factors predicting development of end-stage renal disease. Clin Transplant 2004; 18: 94-9.
Sanchez EQ, Gonwa TA, Levy MF, et al. Preoperative and perioperative predictors of the need for renal replacement therapy after orthotopic liver transplantation. Transplantation 2004; 78: 1048-54.
Bellomo R, Harris C, Kang Y, Daniel E, Fung JJ, Bronsther O. Combined veno-venous bypass and high volume hemofiltration during orthotopic liver transplantation. ASAIO J 1993; 39: 954-6.
Korbet SM, Casey C, Rodby RA, Williams W. The use of continuous arteriovenous hemofiltration in orthotopic liver transplantation. Clin Nephrol 1995; 43: 134-6.
Salord F, Bailly MP, Gaussorgues P, Workineh S, Pouyet M, Robert D. Continuous arteriovenous haemodialysis during emergency hepatic retransplantation: two case reports. Intensive Care Med 1990; 16: 330-1.
Davenport A, Will EJ, Davidson AM. Improved cardiovascular stability during continuous modes of renal replacement therapy in critically ill patients with acute hepatic and renal failure. Crit Care Med 1993; 21: 328-38.
Davenport A, Will EJ, Davison AM, et al. Changes in intracranial pressure during haemofiltration in oliguric patients with grade IV hepatic encephalopathy. Nephron 1989; 53: 142-6.
Townsend DR, Bagshaw SM, Jacka MJ, Bigam D, Cave D, Gibney RT. Intraoperative renal support during liver transplantation. Liver Transpl 2009; 15: 73-8.
Stelfox HT, Ahmed SB, Khandwala F, Zygun D, Shahpori R, Laupland K. The epidemiology of intensive care unit-acquired hyponatraemia and hypernatraemia in medical-surgical intensive care units. Crit Care 2008; 12: R162.
Stelfox HT, Ahmed SB, Zygun D, Khandwala F, Laupland K. Characterization of intensive care unit acquired hyponatremia and hypernatremia following cardiac surgery. Can J Anesth 2010; 57: 650-8.
Wald R, Jaber BL, Price LL, Upadhyay A, Madias NE. Impact of hospital-associated hyponatremia on selected outcomes. Arch Intern Med 2010; 170: 294-302.
Ostermann M, Dickie H, Tovey L, Treacher D. Management of sodium disorders during continuous haemofiltration. Crit Care 2010; 14: 418.
Acknowledgements
We are grateful to all those who supported and contributed to the Edmonton 2010 Acute Kidney Injury and Renal Support in Critical Illness Symposium and to this comprehensive overview of Critical Care Nephrology.
Dr. Bagshaw is supported by a Clinical Investigator Award from the Alberta Heritage Foundation for Medical Research. Dr. Zappitelli is supported by the Kidney Research Scientist Core Education and National Training program, the Fondation de Recherche en Santé du Québec, and the Montreal Children’s Hospital Research Institute.
Conflicts of interest/Financial disclosures
Dr. Bagshaw has received honoraria for speaking from Inverness Medical. Dr. Devarajan is a co-inventor on NGAL patents. Biosite®Incorporated has signed an exclusive licensing agreement with Cincinnati Children’s Hospital for developing plasma NGAL as a biomarker of acute renal failure. Abbott Diagnostics has signed an exclusive licensing agreement with Cincinnati Children’s Hospital for developing urine NGAL as a biomarker of acute renal failure. Dr. Devarajan has received honoraria for speaking assignments from Biosite® Incorporated and Abbott Diagnostics. Dr. Bellomo has acted as a paid consultant for Abbott Diagnostics and Inverness Medical. Drs. Sheinfeld and Gibney have received honoraria for speaking from Gambro Inc.
Author information
Authors and Affiliations
Corresponding author
Additional information
Editor’s Note: This article is the second of two linked special review articles published in this issue of the Journal. The concept of these articles emerged from the scientific content of the 2010 Acute Kidney Injury (AKI) and Renal Support in Critical Illness Symposium, hosted in Edmonton, Alberta. This review (Part 2) provides a focused and comprehensive update on emerging evidence regarding the practice of acute renal replacement therapy (RRT) for critically ill patients, extracorporeal therapies in sepsis, liver failure, and rhabdomyolysis, along with practical considerations in their management.
Rights and permissions
About this article
Cite this article
Bagshaw, S.M., Bellomo, R., Devarajan, P. et al. Review article: Renal support in critical illness. Can J Anesth/J Can Anesth 57, 999–1013 (2010). https://doi.org/10.1007/s12630-010-9376-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-010-9376-3