Abstract
Objective
High permeability hemofiltration (HP-HF) is a new renal replacement modality designed to facilitate the elimination of cytokines in sepsis. Clinical safety data on this new procedure is still lacking. This study investigates the effects of HP-HF on the protein and coagulation status as well as on cardiovascular hemodynamics in patients with septic shock. In addition, the clearance capacity for interleukin-6 (IL-6) and tumor necrosis factor-α (TNF-α) is analyzed.
Design
Prospective, single-center pilot trial.
Setting
University hospital.
Patients
Sixteen patients with multiple organ failure (MOF) induced by septic shock were studied.
Intervention
Patients were treated by intermittent high permeability hemofiltration (iHP-HF; nominal cut-off point: 60 kilodaltons). Intermittent HP-HF was performed over 5 days for 12 h per day and alternated with conventional hemofiltration.
Measurements and results
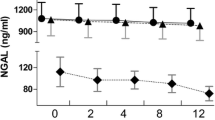
Intermittent HP-HF proved to be a safe hemofiltration modality in regard to cardiovascular hemodynamics and its impact on the coagulation status. However, transmembrane protein loss occurred and cumulative 12-h protein loss was 7.60 g (IQR: 6.2–12.0). The filtration capacity for IL-6 was exceptionally high. The IL-6 sieving coefficient approximated 1 throughout the study period. The total plasma IL-6 burden, estimated by area under curve analysis, declined over time (p<0.001 vs baseline). The TNF-α elimination capacity was poor.
Conclusions
High permeability hemofiltration is a new approach in the adjuvant therapy of sepsis that facilitates the elimination of cytokines. HP-HF alternating with conventional hemofiltration is well tolerated. Further studies are needed to analyze whether HP-HF is able to mitigate the course of sepsis.





Similar content being viewed by others
References
Barton R, Cerra FB (1989) The hypermetabolism multiple organ failure syndrome. Chest 96:1153–1161
Pinsky MR, Vincent JL, Deviere J, Alegre M, Kahn RJ, Dupont E (1993) Serum cytokine levels in human septic shock. Relation to multiple-system organ failure and mortality. Chest 103:565–575
Heering P, Morgera S, Schmitz FJ, Schmitz G, Willers R, Schultheiss HP, Strauer BE, Grabensee B (1997) Cytokine removal and cardiovascular hemodynamics in septic patients with continuous venovenous hemofiltration. Intensive Care Med 23:288–296
Bellomo R, Ronco C (2001) Blood purification in the intensive care unit: evolving concepts. World J Surg 25:677–668
De Vriese AS, Colardyn FA, Philippe JJ, Vanholder RC, De Sutter JH, Lameire NH (1999) Cytokine removal during continuous hemofiltration in septic patients. J Am Soc Nephrol 10:846–853
Silvester W (1997) Mediator removal with CRRT: complement and cytokines. Am J Kidney Dis 30:38–43
Goldfarb S, Golper T (1994) Proinflammatory cytokines and hemofiltration membranes. J Am Soc Nephrol 5:228–232
Lonnemann G, Bechstein M, Linnenweber S, Burg M, Koch KM (1999) Tumor necrosis factor-alpha during continuous high-flux hemodialysis in sepsis with acute renal failure. Kidney Int 56:84–87
Van Deuren M, van der Meer JW (2000) Hemofiltration in septic patients is not able to alter the plasma concentration of cytokines therapeutically. Intensive Care Med 26:1176–1178
Sanchez-Izquierdo JA, Perez Vela JL, Lozano Quintana MJ, Alted Lopez E, Ortuno de Solo B, Ambros Checa A (1997) Cytokines clearance during venovenous hemofiltration in the trauma patient. Am J Kidney Dis 30:483–488
Hoffmann JN, Faist E (2001) Removal of mediators by continuous hemofiltration in septic patients. World J Surg 25:651–659
Lee PA, Weger GW, Pryor RW, Matson JR (1998) Effects of filter pore size on efficacy of continuous arteriovenous hemofiltration therapy for Staphylococcus aureus-induced septicemia in immature swine. Crit Care Med 26:730–737
Knaus WA, Draper EA, Wagner DP, Zimmermann JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Moreno R, Vincent JL, Matos R, Mendonca A, Cantraine F, Thijs L, Takala J, Sprung C, Antonelli M, Bruining H, Willatts S (1999) The use of maximum SOFA score to quantify organ dysfunction/failure in intensive care. Results of a prospective, multicentre study. Working Group on Sepsis-related Problems of the ESICM. Intensive Care Med 25:686–696
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 101:1644–1655
Hoffmann JN, Hartl WH, Deppisch R, Faist E, Jochum M, Inthorn D (1996) Effect of hemofiltration on hemodynamics and systemic concentrations of anaphylatoxins and cytokines in human sepsis. Intensive Care Med 22:1360–1367
Hinshaw LB (1996) Sepsis/septic shock: participation of the microcirculation: an abbreviated review. Crit Care Med 24:1072–1078
Bone RC (1996) Immunologic dissonance: a continuing evolution in our understanding of the systemic inflammatory response syndrome (SIRS) and the multiple organ dysfunction syndrome. Ann Intern Med 125:680–687
Bone RC, Grodzin CJ, Balk RA (1997) Sepsis: a new hypothesis for pathogenesis of the disease process. Chest 112:235–243
Uchino S, Bellomo R, Goldsmith D, Davenport P, Cole L, Baldwin I, Panagiotopoulos S, Tipping P (2002) Super high flux hemofiltration: a new technique for cytokine removal. Intensive Care Med 28:651–655
Uchino S, Bellomo R, Morimatsu H, Goldsmith D, Davenport P, Cole L, Baldwin I, Panagiotopoulos S, Tipping P, Morgera S, Neumayer HH, Goehl H (2002) Cytokine dialysis: an ex vivo study. ASAIO J 48:650–653
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morgera, S., Rocktäschel, J., Haase, M. et al. Intermittent high permeability hemofiltration in septic patients with acute renal failure. Intensive Care Med 29, 1989–1995 (2003). https://doi.org/10.1007/s00134-003-2003-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-2003-9