Abstract
Background
Non-invasive assessment of subclinical atherosclerosis by means of coronary artery calcium scoring (CACS) and multi-slice computed tomography (MSCT) coronary angiography could improve patients’ risk stratification. However, data relating observations on CACS and MSCT coronary angiography to traditional risk assessment are scarce.
Methods and Results
In 314 consecutive outpatients (54 ± 13 years, 56% males) without known CAD, CACS and 64-slice MSCT coronary angiography were performed. According to the Framingham risk score (FRS), 51% of patients were at low, 24% at intermediate and 25% at high risk, respectively. MSCT angiograms showing atherosclerosis were classified as showing obstructive (≥50% luminal narrowing) CAD or not. Both CACS and MSCT coronary angiography showed a high prevalence of normal coronary arteries in low FRS patients (70% and 61%, respectively). An increase in the prevalence of CACS >400 (4% low vs 19% intermediate vs 36% high), CAD (39% low vs 79% intermediate vs 91% high), and obstructive CAD (15% low vs 43% intermediate vs 58% high) was observed across the FRS categories (P < .0001 for all comparisons).
Conclusions
A strong positive relationship exists between FRS and the prevalence and extent of atherosclerosis. Especially in intermediate FRS patients, CACS and MSCT coronary angiography provide useful information on the presence of subclinical atherosclerosis.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Identification of patients at risk of developing coronary artery disease (CAD) events is one of the most challenging issues in clinical cardiology. For this purpose, several scoring tools that take demographic and clinical characteristics into account have been developed. These tools allow stratification of patients into low-, intermediate-, and high-risk categories, in order to determine the intensity of risk-modifying interventions.1-3 Among them, the Framingham risk score (FRS) is one of the most frequently used;1,4 it considers traditional risk factors (age, gender, diabetes mellitus, systolic blood pressure, total cholesterol and HDL cholesterol level, and smoking history) to predict the 10-year risk of hard CAD events. However, traditional risk assessment may still fail to identify a considerable proportion of patients with future CAD events, since it provides a statistical probability of having CAD rather than a direct individual assessment.5 Indeed, it has been observed that as much as 20% of CAD events can occur in the absence of major cardiovascular risk factors.6
To improve risk stratification, direct visualization of subclinical atherosclerosis has been advocated. Indeed, previous studies have shown that non-invasive assessment of the coronary artery calcium score (CACS), by means of electron-beam computed tomography (EBCT) or multi-slice computed tomography (MSCT) provides prognostic information that is incremental to traditional risk stratification.7 Recently, more detailed visualization of the coronary arteries has become possible with the introduction of MSCT coronary angiography.8-10 Possibly, MSCT coronary angiography could also improve patients’ risk stratification similar to CACS. However, data relating observations on CACS and MSCT coronary angiography to traditional risk assessment are scarce. Aim of the present study therefore was to evaluate the prevalence of CAD across the FRS categories using CACS and MSCT coronary angiography. In addition, differences in CACS and MSCT coronary angiography findings between asymptomatic and symptomatic patients were explored.
Methods
Study Population
The study population consisted of 314 consecutive outpatients clinically referred to MSCT for coronary evaluation, due to an increased risk profile and/or stable chest pain complaints. Patients with typical angina, known history of CAD and/or contraindications to MSCT were not included in the study, as well as patients who were not in sinus rhythm during the MSCT examination. History of CAD was defined as the presence of previous acute coronary syndrome, percutaneous or surgical coronary revascularization, and/or one or more angiographically documented coronary artery stenosis ≥50% luminal diameter.11 Contraindications for MSCT were: (1) known allergy to iodinated contrast agent, (2) renal failure (defined as glomerular filtration rate <30 mL/min), and (3) pregnancy.
For each patient, the presence of coronary risk factors (diabetes mellitus, systemic hypertension, hypercholesterolemia, positive family history, cigarette smoking, and obesity) and the presence of chest pain complaints (atypical angina and non-cardiac chest pain), both defined in accordance to previously published guidelines,4,12-15 were recorded. The Framingham 10-year risk of hard CAD events was also calculated as previously described in the National Cholesterol Education Program’s Adult Treatment Panel III report.4 In accordance with the FRS, the study population was then categorized as at low (<10%), intermediate (10-20%), and high risk (>20%).4 In addition, patients were further divided as being asymptomatic or symptomatic.
MSCT Data Acquisition
MSCT coronary angiography was performed with a 64-slice MSCT scanner (Aquilion 64, Toshiba Medical Systems, Japan). The heart rate and blood pressure were monitored before the examination in each patient. In the absence of contraindications, patients with a heart rate ≥65 beats/minute were administered oral ß-blockers (metoprolol, 50 or 100 mg, single dose, 1 hour before the examination).
First, a prospective coronary calcium scan without contrast was performed, followed by 64-slice MSCT coronary angiography, performed according to protocols previously described.16 Data were subsequently transferred to dedicated workstations for post-processing and evaluation (Advantage, GE Healthcare, USA and Vitrea 2, Vital Images, USA).
MSCT Data Analysis
The MSCT data analysis was performed by two experienced observers who had no knowledge of the patient’s medical history and symptom status; disagreement was solved by consensus or evaluation by a third observer.
Coronary artery calcium score
Coronary artery calcium was identified as a dense area in the coronary artery >130 Hounsfield units. A total CACS was recorded for each patient. In accordance with the value of total CACS, patients were subsequently categorized as having no calcium (total score = 0) or low (total score = 1-100), moderate (total score = 101-400), and severe (total score > 400) CACS.17
MSCT coronary angiography
MSCT coronary angiograms were evaluated for the presence of obstructive CAD (≥50% luminal narrowing) on a patient and vessel level. For this purpose, both the original axial dataset as well as curved multi-planar reconstructions were used. Each vessel was evaluated for the presence of any atherosclerotic plaque, defined as structures >1 mm² within and/or adjacent to the coronary artery lumen, which could be clearly distinguished from the vessel lumen and the surrounding pericardial tissue, as described previously.9 Subsequently, the vessels were further classified as 1. completely normal, 2. having non-obstructive CAD when atherosclerotic lesions <50% of luminal diameter were present, or 3. having obstructive CAD when atherosclerotic lesions ≥50% of luminal diameter were present.
The prevalence of CAD (including obstructive and non-obstructive CAD), obstructive CAD, the presence of obstructive CAD in one vessel (single-vessel disease) or two or three vessels (multi-vessel disease), and location in the left main (LM) and/or proximal left anterior descending (LAD) coronary artery were evaluated. Multi-vessel disease and LM and/or proximal LAD disease were considered to represent high-risk features.
Statistical Analysis
Continuous variables are expressed as mean (standard deviation) or as median (25th to 75th percentile range), when not normally distributed. Categorical variables are expressed as absolute numbers (percentages). The differences in continuous variables were assessed using the Student t test when normally distributed and the Mann-Whitney test when not normally distributed. Χ² for greater than two-by-two and Fisher exact for two-by-two contingency tables were computed to test for differences in categorical variables. A P value <.05 was considered statistically significant. Statistical analyses were performed using SPSS software (version 14.0, SPSS Inc, Chicago, IL, USA).
Results
Patient Characteristics
Baseline characteristics of the study population are shown in Table 1. The mean age was 54 ± 13 years, and 177 (56%) patients were male. A total of 152 (48%) patients were asymptomatic, while 82 (26%) patients had history of atypical angina and 80 (26%) patients had a history of non-cardiac chest pain. The FRS was low, intermediate, and high, respectively, in 159 (51%), 77 (24%), and 78 (25%) patients.
MSCT Calcium Scoring and Coronary Angiography
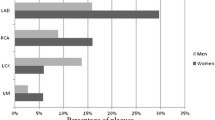
Table 2 and Figures 1 and 2 depict the results of calcium scoring and MSCT coronary angiography in the overall population and among asymptomatic and symptomatic patients.
Relationship between CACS and Framingham 10-year risk of hard coronary heart disease events in the overall population (A), among asymptomatic patients (B), and among symptomatic patients (C). The proportion of patients with no calcium, low CACS, intermediate CACS, and severe CACS differed significantly across the three FRS categories. CACS, Coronary artery calcium score; FRS, Framingham risk score
Relationship between MSCT coronary angiography and Framingham 10-year risk of hard coronary heart disease events in the overall population (A), among asymptomatic patients (B), and among symptomatic patients (C). The proportion of patients with normal coronary arteries, non-obstructive CAD, and obstructive CAD differed significantly across the three FRS categories. CAD, Coronary artery disease; FRS, Framingham risk score
Coronary artery calcium score
As shown in Table 2, the median CACS was 1 (25th to 75th percentile range 0-159). No calcium was observed in 157 (50%), while CACS was low in 63 (20%) patients, moderate in 44 (14%), and severe in 50 (16%) patients.
The median CACS did not differ between asymptomatic and symptomatic patients and the prevalence of no calcium and minimal, mild, moderate, and severe coronary calcifications was not statistically different between the two groups (Table 2).
Relationship between CACS and FRS As shown in Figure 1A, calcium was absent in 112 (70%) patients with low FRS, 26 (34%) patients with intermediate FRS, and in 19 (24%) patients with high FRS. Overall, a decrease in the prevalence of CACS zero and an increase in the prevalence of severe CACS were observed in line with increasing FRS (Figure 1A). However, among all three FRS categories still a significant proportion of patients presented with low and moderate CACS.
As shown in Figure 1B and C, this positive relationship between FRS and CACS was similarly present among both asymptomatic and symptomatic patients.
MSCT coronary angiography
As shown in Table 2, 120 (38%) patients were classified as having no CAD based on MSCT. A total of 92 (29%) patients showed non-obstructive CAD, whereas at least one significant (≥50% luminal narrowing) stenosis was observed in the remaining 102 (33%) patients. Obstructive single-vessel disease was present in 54 (17%) patients, whereas multi-vessel disease was noted in 48 (15%) patients. Obstructive CAD in the LM and/or proximal LAD was present in 37 (12%) patients, of which 24 also showed multi-vessel disease. Accordingly, 61 (19%) patients were identified as having high-risk features.
No difference in the prevalence of no CAD, and non-obstructive and obstructive CAD was observed between asymptomatic and symptomatic patients (Table 2).
Relationship between MSCT coronary angiography results and FRS As shown in Figure 2A, normal coronary arteries were observed in 97 (61%) patients with low FRS, 16 (21%) patients with intermediate FRS, and 7 (9%) patient with high FRS. Overall, a decrease in the prevalence of normal coronary arteries and an increase in the prevalence of obstructive CAD were observed in line with increasing FRS (Figure 2A). Moreover, an increase in the prevalence of high-risk features was observed across the FRS categories (13 (8%) patients in the low FRS versus 21 (27%) in the intermediate FRS versus 27 (35%) in the high FRS; P < .0001). Nevertheless, a significant proportion of patients with non-obstructive CAD was present in each category.
As shown in Figure 2B and C, this positive relationship between FRS and CAD was similarly present among both asymptomatic and symptomatic patients.
Discussion
The present study describes the prevalence and extent of CAD, assessed by means of both CACS and MSCT coronary angiography, across the FRS categories in a large cohort of patients. Both CACS and MSCT coronary angiography showed a high prevalence of normal coronary arteries in low FRS patients (70% and 61%, respectively), which decreased in patients with intermediate and high FRS. Similarly, an increase in the prevalence of high CACS and obstructive or even high-risk CAD were observed with increasing FRS. However, moderate calcium on CACS as well as non-obstructive CAD on MSCT coronary angiography were identified across all FRS categories.
In line with the current observations, an overall increase in the prevalence and extent of atherosclerosis in relation to FRS has been reported in several previous studies.18-21 At the same time, these studies have also highlighted a discrepancy between the presence of traditional risk factors and the presence of subclinical atherosclerosis: substantial atherosclerosis was frequently observed in patients at low to intermediate risk, while being absent in patients deemed at high risk. Also in the current study, atherosclerosis was identified across all FRS categories. These observations have led to the notion that (selective) atherosclerosis imaging may provide valuable information in addition to traditional risk assessment. Indeed, several large clinical trials have demonstrated that CACS has incremental value over risk factors.7,22,23 In a large cohort of 1461 asymptomatic individuals, Greenland et al7 demonstrated that knowledge of a high CACS resulted in superior risk stratification as compared to FRS alone. Other investigations have reported similar observations.22,23 Accordingly, addition of an atherosclerosis marker such as CACS can significantly modify initially predicted risk and can alter clinical decision-making and subsequent therapy/patients management. Knowledge of subclinical atherosclerosis may be of particular value in patients at intermediate risk. In these patients, who represent a substantial part of the population, clinical management is frequently uncertain. In the present study, evaluation by means of MSCT showed that coronary calcium was absent in 34% of patients. In contrast, a CACS exceeding 100 was observed in 45% of patients. Similarly, MSCT coronary angiography showed normal coronary arteries in 21%, whereas obstructive disease was noted in 43% of patients. Moreover, high-risk features were identified in 27%. Accordingly, these observations indicate that underlying atherosclerosis can be identified (but also ruled out) in a substantial proportion of patients at intermediate FRS. Possibly, refinement of risk using atherosclerosis imaging may allow more appropriate targeting of preventive measures in these patients. Indeed, the current American College of Cardiology appropriateness criteria for cardiac computed tomography suggest that assessment of calcium may be a “reasonable approach” among intermediate FRS patients, although substantial uncertainty remains regarding its general applicability.24
In low risk patients, the use of imaging remains controversial. In general, the prevalence of abnormal coronary arteries will be low. Indeed, in the present study, the prevalence of normal coronary arteries was high both on CACS and MSCT coronary angiography. Also, prognostic studies addressing CACS in relation to FRS observed that CACS had no additive value in patients with a FRS <10%.7 Still, recent data suggest that perhaps in certain subsets of individuals deemed at low risk by FRS, such as women younger than 70 years old, CACS may identify higher risk in a considerable proportion.25,26 Nevertheless, more data are needed before evaluation of atherosclerosis can be recommended in patients with low FRS.
In patients with high FRS on the other hand, the incremental value of atherosclerosis imaging remains debatable as well. In line with previous investigations, we observed a high prevalence of coronary calcium (76%). Moreover, the prevalence of abnormal coronary arteries on MSCT coronary angiography was even higher, 91%. Finally, a high prevalence of high-risk features was noted on MSCT coronary angiography as well (35%). Indeed, in this group of patients, the presence of high risk has already been established and these patients should receive targeted anti-atherosclerotic measures regardless of imaging results. In this context, assessment with MSCT coronary angiography may be favored over CACS as the former may provide a superior estimate of total plaque burden. Moreover, another advantage of MSCT coronary angiography could be the fact that it allows identification of high-risk features such as left main or multi-vessel disease. Possibly, these patients may benefit from even more aggressive measures, including revascularization, although supporting data in asymptomatic patients are scarce.
It is important to realize that thus far, the majority of data relating coronary atherosclerosis to FRS have been obtained using CACS with EBCT and data relating MSCT coronary angiography to clinical characteristics are scarce. Moreover, MSCT coronary angiography has mainly been applied in high-risk symptomatic patients in order to determine its value in the diagnosis of CAD rather than in risk assessment. As a result, only few data are available concerning its prognostic value.27,28 Preliminary studies however suggest that MSCT coronary angiography may provide prognostic information incremental to baseline risk stratification,29 although no systematic comparisons to FRS are currently available. In addition, no studies are available that evaluate the relative merits of CACS and MSCT coronary angiography with regard to risk stratification. Importantly, efficacy in improving patient outcome remains to be confirmed for both techniques.
The present study has some limitations that should be acknowledged. First, it is a single center experience with a relatively low sample size as compared to previous studies relating CACS to FRS. However, it is also one of the first relating both CACS and MSCT coronary angiography to FRS in patients without symptoms typical for CAD. Unfortunately, no follow-up data were available. Future studies should address whether MSCT coronary angiography may allow re-stratification of risk similar or even superior to CACS. Second, the FRS was developed in, and should be applied to, asymptomatic individuals only; however, due to the radiation exposure associated with MSCT coronary angiography, and the lack of evidence in this setting, use in truly asymptomatic patients cannot be recommended at present. This limitation could be overcome by more extensive implementation of dose-saving algorithms, which are likely to result in substantial dose reduction to <3 mSv, without degradation of image quality.30,31
Conclusion
A strong positive relationship exists between FRS and the prevalence and extent atherosclerosis on CACS and MSCT coronary angiography. Both techniques showed a high prevalence of normal coronary arteries in low FRS patients versus a low prevalence in high FRS patients. In intermediate FRS patients, however, CACS and MSCT coronary angiography may provide useful information on the presence of subclinical atherosclerosis.
References
Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation 1998;97:1837-47.
Assmann G, Cullen P, Schulte H. Simple scoring scheme for calculating the risk of acute coronary events based on the 10-year follow-up of the prospective cardiovascular Munster (PROCAM) study. Circulation 2002;105:310-5.
Conroy RM, Pyorala K, Fitzgerald AP, Sans S, Menotti A, De Backer G, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: The SCORE project. Eur Heart J 2003;24:987-1003.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 2001;285:2486-97.
Naghavi M, Libby P, Falk E, Casscells SW, Litovsky S, Rumberger J, et al. From vulnerable plaque to vulnerable patient: A call for new definitions and risk assessment strategies: Part II. Circulation 2003;108:1772-8.
Khot UN, Khot MB, Bajzer CT, Sapp SK, Ohman EM, Brener SJ, et al. Prevalence of conventional risk factors in patients with coronary heart disease. JAMA 2003;290:898-904.
Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA 2004;291:210-5.
Leber AW, Knez A, von Ziegler F, Becker A, Nikolaou K, Paul S, et al. Quantification of obstructive and nonobstructive coronary lesions by 64-slice computed tomography: A comparative study with quantitative coronary angiography and intravascular ultrasound. J Am Coll Cardiol 2005;46:147-54.
Leber AW, Knez A, Becker A, Becker C, von Ziegler F, Nikolaou K, et al. Accuracy of multidetector spiral computed tomography in identifying and differentiating the composition of coronary atherosclerotic plaques: A comparative study with intracoronary ultrasound. J Am Coll Cardiol 2004;43:1241-7.
Lau GT, Ridley LJ, Schieb MC, Brieger DB, Freedman SB, Wong LA, et al. Coronary artery stenoses: Detection with calcium scoring, CT angiography, and both methods combined. Radiology 2005;235:415-22.
Schuijf JD, Wijns W, Jukema JW, Atsma DE, de Roos A, Lamb HJ, et al. Relationship between noninvasive coronary angiography with multi-slice computed tomography and myocardial perfusion imaging. J Am Coll Cardiol 2006;48:2508-14.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2007;30:S42-7.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 2003;42:1206-52.
World Health Organization. Physical status: The use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser 1995;854:1-452.
Gibbons RJ, Abrams J, Chatterjee K, Daley J, Deedwania PC, Douglas JS, et al. ACC/AHA 2002 guideline update for the management of patients with chronic stable angina—summary article: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Chronic Stable Angina). Circulation 2003;107:149-58.
Schuijf JD, Pundziute G, Jukema JW, Lamb HJ, van der Hoeven BL, de Roos A, et al. Diagnostic accuracy of 64-slice multislice computed tomography in the noninvasive evaluation of significant coronary artery disease. Am J Cardiol 2006;98:145-8.
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990;15:827-32.
Simon A, Giral P, Levenson J. Extracoronary atherosclerotic plaque at multiple sites and total coronary calcification deposit in asymptomatic men. Association with coronary risk profile. Circulation 1995;92:1414-21.
Mahoney LT, Burns TL, Stanford W, Thompson BH, Witt JD, Rost CA, et al. Usefulness of the Framingham risk score and body mass index to predict early coronary artery calcium in young adults (Muscatine Study). Am J Cardiol 2001;88:509-15.
Taylor AJ, Feuerstein I, Wong H, Barko W, Brazaitis M, O’Malley PG. Do conventional risk factors predict subclinical coronary artery disease? Results from the prospective army coronary calcium project. Am Heart J 2001;141:463-8.
Nair D, Carrigan TP, Curtin RJ, Popovic ZB, Kuzmiak S, Schoenhagen P, et al. Association of coronary atherosclerosis detected by multislice computed tomography and traditional risk-factor assessment. Am J Cardiol 2008;102:316-20.
Arad Y, Goodman KJ, Roth M, Newstein D, Guerci AD. Coronary calcification, coronary disease risk factors, C-reactive protein, and atherosclerotic cardiovascular disease events: The St. Francis Heart Study. J Am Coll Cardiol 2005;46:158-65.
Taylor AJ, Bindeman J, Feuerstein I, Cao F, Brazaitis M, O’Malley PG. Coronary calcium independently predicts incident premature coronary heart disease over measured cardiovascular risk factors: Mean three-year outcomes in the prospective army coronary calcium (PACC) project. J Am Coll Cardiol 2005;46:807-14.
Hendel RC, Patel MR, Kramer CM, Poon M, Hendel RC, Carr JC, et al. ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR 2006 appropriateness criteria for cardiac computed tomography and cardiac magnetic resonance imaging: A report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American College of Radiology, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, American Society of Nuclear Cardiology, North American Society for Cardiac Imaging, Society for Cardiovascular Angiography and Interventions, and Society of Interventional Radiology. J Am Coll Cardiol 2006;48:1475-97.
Michos ED, Nasir K, Braunstein JB, Rumberger JA, Budoff MJ, Post WS, et al. Framingham risk equation underestimates subclinical atherosclerosis risk in asymptomatic women. Atherosclerosis 2006;184:201-6.
Lakoski SG, Greenland P, Wong ND, Schreiner PJ, Herrington DM, Kronmal RA, et al. Coronary artery calcium scores and risk for cardiovascular events in women classified as “low risk” based on Framingham risk score: The multi-ethnic study of atherosclerosis (MESA). Arch Intern Med 2007;167:2437-42.
Pundziute G, Schuijf JD, Jukema JW, Boersma E, de Roos A, van der Wall EE, et al. Prognostic value of multislice computed tomography coronary angiography in patients with known or suspected coronary artery disease. J Am Coll Cardiol 2007;49:62-70.
Min JK, Shaw LJ, Devereux RB, Okin PM, Weinsaft JW, Russo DJ, et al. Prognostic value of multidetector coronary computed tomographic angiography for prediction of all-cause mortality. J Am Coll Cardiol 2007;50:1161-70.
Choi EK, Choi SI, Rivera JJ, Nasir K, Chang SA, Chun EJ, et al. Coronary computed tomography angiography as a screening tool for the detection of occult coronary artery disease in asymptomatic individuals. J Am Coll Cardiol 2008;52:357-65.
Hausleiter J, Meyer T, Hadamitzky M, Huber E, Zankl M, Martinoff S, et al. Radiation dose estimates from cardiac multislice computed tomography in daily practice: Impact of different scanning protocols on effective dose estimates. Circulation 2006;113:1305-10.
Stolzmann P, Leschka S, Scheffel H, Krauss T, Desbiolles L, Plass A, et al. Dual-source CT in step-and-shoot mode: Noninvasive coronary angiography with low radiation dose. Radiology 2008;249:71-80.
Acknowledgment
Conflict of interest and financial disclosures: Gaetano Nucifora is financially supported by the European Association of Percutaneous Cardiovascular Interventions. Jacob M. van Werkhoven is financially supported by the Netherlands Society of Cardiology. Jeroen J. Bax has research grants from Biotronik, BMS medical imaging, Boston Scientific, Edwards Lifesciences, GE Healthcare, Medtronic, and St. Jude Medical. Martin J. Schalij has research grants from Biotronik, Boston Scientific, and Medtronic.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Nucifora, G., Schuijf, J.D., van Werkhoven, J.M. et al. Prevalence of coronary artery disease across the Framingham risk categories: coronary artery calcium scoring and MSCT coronary angiography. J. Nucl. Cardiol. 16, 368–375 (2009). https://doi.org/10.1007/s12350-009-9059-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-009-9059-z