Abstract
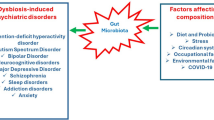
Gut microbes play prime role in human health and have shown to exert their influence on various physiological responses including neurological functions. Growing evidences in recent years have indicated a key role of gut microbiota in contributing to mental health. The connection between gut and brain is modulated by microbes via neural, neuroendocrinal and metabolic pathways that are mediated through various neurotransmitters and their precursors, hormones, cytokines and bioactive metabolites. Impaired functioning of this connection can lead to manifestation of mental disorders. Around 1 billion of the world population is reported to suffer from emotional, psychological and neurological imbalances, substance use disorders and cognitive, psychosocial and intellectual disabilities. Thus, it becomes imperative to understand the role of gut microbes in mental disorders. Since variations occur in the conditions associated with different mental disorders and some of them have overlapping symptoms, it becomes important to have a holistic understanding of gut dysbiosis in these disorders. In this review, we consolidate the recent data on alterations in the gut microbes and its consequences in various neurological, psychological and neurodegenerative disorders. Further, considering these evidences, several studies have been undertaken to specifically target the gut microbiota through different therapeutic interventions including administration of live microbes (psychobiotics) to treat mental health disorders and/or their symptoms. We review these studies and propose that an integrative and personalized approach, where combinations of microbe-based therapeutic interventions to modulate gut microbes and in-use psychological treatment practices can be integrated and based on patient’s gut microbiome can be potentially adopted for effective treatment of the mental disorders.



Similar content being viewed by others
References
Cullen CM, Aneja KK, Beyhan S, Cho CE, Woloszynek S, Convertino M, McCoy SJ, Zhang Y, Anderson MZ, Alvarez-Ponce D, Smirnova E, Karstens L, Dorrestein PC, Li H, Sen Gupta A, Cheung K, Powers JG, Zhao Z, Rosen GL (2020) Emerging priorities for microbiome research. Front Microbiol 11:136. https://doi.org/10.3389/fmicb.2020.00136
Arnold WM, Hill ES, Fei N, Yee AL, Garcia MS, Cralle LE, Gilbert JA (2019) The human microbiome in health and disease. In: Netto G, Kaul K (eds) Genomic applications in pathology. Springer, Cham, pp 607–618. https://doi.org/10.1007/978-3-319-96830-8_39
Singhvi N, Gupta V, Gaur M, Sharma V, Puri A, Singh Y, Dubey GP, Lal R (2020) Interplay of human gut microbiome in health and wellness. Indian J Microbiol 60:26–36. https://doi.org/10.1007/s12088-019-00825-x
Ekanayake A, Madegedara D, Chandrasekharan V, Magana-Arachchi D (2020) Respiratory bacterial microbiota and individual bacterial variability in lung cancer and bronchiectasis patients. Indian J Microbiol 60:196–205. https://doi.org/10.1007/s12088-019-00850-w
Rogers GB, Keating DJ, Young RL, Wong ML, Licinio J, Wesselingh S (2016) From gut dysbiosis to altered brain function and mental illness: mechanisms and pathways. Mol Psychiatry 21:738–748. https://doi.org/10.1038/mp.2016.50
Gupta V, Sood U, Kumar R, Lal R, Kalia VC (2020) Microbiome: a new lease to microbiology. Indian J Microbiol 60:1. https://doi.org/10.1007/s12088-019-00852-8
Sender R, Fuchs S, Milo R (2016) Revised estimates for the number of human and bacteria cells in the body. PLoS Biol 14:e1002533. https://doi.org/10.1371/journal.pbio.1002533
Kho ZY, Lal SK (2018) The human gut microbiome—a potential controller of wellness and disease. Front Microbiol 9:1835. https://doi.org/10.3389/fmicb.2018.01835
Dafale NA, Srivastava S, Purohit HJ (2020) Zoonosis: an emerging link to antibiotic resistance under "One Health Approach". Indian J Microbiol 60:139–152. https://doi.org/10.1007/s12088-020-00860-z
Carabotti M, Scirocco A, Maselli MA, Severi C (2015) The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol 28:203–209
Dinan TG, Cryan JF (2017) The microbiome-gut-brain axis in health and disease. Gastroenterol Clin North Am 46:77–89. https://doi.org/10.1016/j.gtc.2016.09.007
GBD (2017) Disease and Injury Incidence and Prevalence Collaborators (2018) Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease study 2017. Lancet 392:1789–1858. https://doi.org/10.1016/S0140-6736(18)32279-7
Bastiaanssen TFS, Cussotto S, Claesson MJ, Clarke G, Dinan TG, Cryan JF (2020) Gutted! unraveling the role of the microbiome in major depressive disorder. Harv Rev Psychiatry 28:26–39. https://doi.org/10.1097/HRP.0000000000000243
Caspani G, Kennedy S, Foster JA, Swann J (2019) Gut microbial metabolites in depression: understanding the biochemical mechanisms. Microb Cell 6:454–481. https://doi.org/10.15698/mic2019.10.693
Neufeld KM, Kang N, Bienenstock J, Foster JA (2011) Reduced anxiety-like behavior and central neurochemical change in germ-free mice. Neurogastroenterol Motil 23(255–264):e119. https://doi.org/10.1111/j.1365-2982.2010.01620.x
Bravo JA, Forsythe P, Chew MV, Escaravage E, Savignac HM, Dinan TG, Bienenstock J, Cryan JF (2011) Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proc Natl Acad Sci USA 108:16050–16055. https://doi.org/10.1073/pnas.1102999108
Roubalova R, Prochazkova P, Papezova H, Smitka K, Bilej M, Tlaskalova-Hogenova H (2020) Anorexia nervosa: gut microbiota-immune-brain interactions. Clin Nutr 39:676–684. https://doi.org/10.1016/j.clnu.2019.03.023
Unger MM, Spiegel J, Dillmann KU, Grundmann D, Philippeit H, Burmann J, Fassbender K, Schwiertz A, Schafer KH (2016) Short chain fatty acids and gut microbiota differ between patients with Parkinson's disease and age-matched controls. Parkinsonism Relat Disord 32:66–72. https://doi.org/10.1016/j.parkreldis.2016.08.019
Zhang L, Wang Y, Xiayu X, Shi C, Chen W, Song N, Fu X, Zhou R, Xu YF, Huang L, Zhu H, Han Y, Qin C (2017) Altered gut microbiota in a mouse model of Alzheimer's disease. J Alzheimers Dis 60:1241–1257. https://doi.org/10.3233/JAD-170020
Wang L, Christophersen CT, Sorich MJ, Gerber JP, Angley MT, Conlon MA (2012) Elevated fecal short chain fatty acid and ammonia concentrations in children with autism spectrum disorder. Dig Dis Sci 57:2096–2102. https://doi.org/10.1007/s10620-012-2167-7
Galland L (2014) The gut microbiome and the brain. J Med Food 17:1261–1272. https://doi.org/10.1089/jmf.2014.7000
Golubeva AV, Joyce SA, Moloney G, Burokas A, Sherwin E, Arboleya S, Flynn I, Khochanskiy D, Moya-Perez A, Peterson V, Rea K, Murphy K, Makarova O, Buravkov S, Hyland NP, Stanton C, Clarke G, Gahan CGM, Dinan TG, Cryan JF (2017) Microbiota-related changes in bile acid & tryptophan metabolism are associated with gastrointestinal dysfunction in a mouse model of autism. EBioMedicine 24:166–178. https://doi.org/10.1016/j.ebiom.2017.09.020
Kim YK, Shin C (2018) The microbiota-gut-brain axis in neuropsychiatric disorders: pathophysiological mechanisms and novel treatments. Curr Neuropharmacol 16:559–573. https://doi.org/10.2174/1570159X15666170915141036
Sagar R, Dandona R, Gururaj G, Dhaliwal RS, Singh A, Ferrari A, Dua T, Ganguli A, Varghese M, Chakma JK, Kumar GA, Shaji KS, Ambekar A, Rangaswamy T, Vijayakumar L, Agarwal V, Krishnankutty RP, Bhatia R, Charlson F, Chowdhary N, Erskine HE, Glenn SD, Krish V, Mantilla Herrera AM, Mutreja P, Odell CM, Pal PK, Prakash S, Santomauro D, Shukla DK, Singh R, Singh RKL, Thakur JS, ThekkePurakkal AS, Varghese CM, Reddy KS, Swaminathan S, Whiteford H, Bekedam HJ, Murray CJL, Vos T, Dandona L (2020) The burden of mental disorders across the states of India: the global burden of disease study 1990–2017. Lancet Psychiatry 7:148–161. https://doi.org/10.1016/S2215-0366(19)30475-4
Bundgaard-Nielsen C, Knudsen J, Leutscher PDC, Lauritsen MB, Nyegaard M, Hagstrøm S, Sørensen S (2020) Gut microbiota profiles of autism spectrum disorder and attention deficit/hyperactivity disorder: a systematic literature review. Gut Microbes. https://doi.org/10.1080/19490976.2020.1748258
Kang D, Adams JB, Coleman D, Pollard EL, Maldonado J, McDonough-Means S, Caporaso JG, Krajmalnik-Brown S (2019) Long-term benefit of Microbiota Transfer Therapy on autism symptoms and gut microbiota. Sci Rep 9:5821. https://doi.org/10.1038/s41598-019-42183-0
Prehn-Kristensen A, Zimmermann A, Tittmann L, Lieb W, Schreiber S, Baving L, Fischer A (2018) Reduced microbiome alpha diversity in young patients with ADHD. PLoS ONE 13:e0200728. https://doi.org/10.1371/journal.pone.0200728
Woo HD, Kim DW, Hong YS, Kim YM, Seo JH, Choe BM, Park JH, Kang JW, Yoo JH, Chueh HW, Lee JH, Kwak MJ, Kim J (2014) Dietary patterns in children with attention deficit/hyperactivity disorder (ADHD). Nutrients 6:1539–1553. https://doi.org/10.3390/nu6041539
Jiang HY, Zhang X, Yu ZH, Zhang Z, Deng M, Zhao JH, Ruan B (2018) Altered gut microbiota profile in patients with generalized anxiety disorder. J Psychiatr Res 104:130–136. https://doi.org/10.1016/j.jpsychires.2018.07.007
Yang B, Wei J, Ju P, Chen J (2019) Effects of regulating intestinal microbiota on anxiety symptoms: a systematic review. Gen Psychiatr 32:e100056. https://doi.org/10.1136/gpsych-2019-100056
Valles-Colomer M, Falony G, Darzi Y, Tigchelaar EF, Wang J, Tito RY, Schiweck C, Kurilshikov A, Joossens M, Wijmenga C, Claes S, Van Oudenhove L, Zhernakova A, Vieira-Silva S, Valles-Colomer M, Falony G, Darzi Y, Tigchelaar EF, Wang J, Tito RY, Schiweck C, Kurilshikov A, Joossens M, Wijmenga C, Claes S, Van Oudenhove L, Zhernakova A, Vieira-Silva S, Raes J (2019) The neuroactive potential of the human gut microbiota in quality of life and depression. Nat Microbiol 4:623–632. https://doi.org/10.1038/s41564-018-0337-x
Huang TT, Lai JB, Du YL, Xu Y, Ruan LM, Hu SH (2019) Current understanding of gut microbiota in mood disorders: an update of human studies. Front Genet 10:98. https://doi.org/10.3389/fgene.2019.00098
Hu S, Li A, Huang T, Lai J, Li J, Sublette ME, Lu H, Lu Q, Du Y, Hu Z, Ng CH, Zhang H, Lu J, Mou T, Lu S, Wang D, Duan J, Hu J, Huang M, Wei N, Zhou W, Ruan L, Li MD, Xu Y (2019) Gut microbiota changes in patients with bipolar depression. Adv Sci (Weinh) 6:1900752. https://doi.org/10.1002/advs.201900752
Rucklidge JJ, Harrison R (2010) Successful treatment of bipolar disorder II and ADHD with a micronutrient formula: a case study. CNS Spectr 15:289–295. https://doi.org/10.1017/s1092852900027516
Flowers SA, Ward KM, Clark CT (2020) The gut microbiome in bipolar disorder and pharmacotherapy management. Neuropsychobiology 79:43–49. https://doi.org/10.1159/000504496
Fond GB, Lagier JC, Honore S, Lancon C, Korchia T, Sunhary De Verville PL, Llorca PM, Auquier P, Guedj E, Boyer L (2020) Microbiota-orientated treatments for major depression and schizophrenia. Nutrients 12:1024. https://doi.org/10.3390/nu12041024
Szeligowski T, Yun AL, Lennox BR, Burnet PWJ (2020) The gut microbiome and schizophrenia: the current state of the field and clinical applications. Front Psychiatry 11:156. https://doi.org/10.3389/fpsyt.2020.00156
Zhu F, Ju Y, Wang W, Wang Q, Guo R, Ma Q, Sun Q, Fan Y, Xie Y, Yang Z, Jie Z, Zhao B, Xiao L, Yang L, Zhang T, Feng J, Guo L, He X, Chen Y, Chen C, Gao C, Xu X, Yang H, Wang J, Dang Y, Madsen L, Brix S, Kristiansen K, Jia H, Ma X (2020) Metagenome-wide association of gut microbiome features for schizophrenia. Nat Commun 11:1612. https://doi.org/10.1038/s41467-020-15457-9
Seitz J, Belheouane M, Schulz N, Dempfle A, Baines JF, Herpertz-Dahlmann B (2019) The impact of starvation on the microbiome and gut-brain interaction in anorexia nervosa. Front Endocrinol (Laussanne) 10:41. https://doi.org/10.3389/fendo.2019.00041
Hata T, Miyata N, Takakura S, Yoshihara K, Asano Y, Kimura-Todani T, Yamashita M, Zhang XT, Watanabe N, Mikami K, Koga Y, Sudo N (2019) The gut microbiome derived from anorexia nervosa patients impairs weight gain and behavioral performance in female mice. Endocrinology 160:2441–2452. https://doi.org/10.1210/en.2019-00408
Leclercq S, Starkel P, Delzenne NM, de Timary P (2019) The gut microbiota: a new target in the management of alcohol dependence? Alcohol 74:105–111. https://doi.org/10.1016/j.alcohol.2018.03.005
Meckel KR, Kiraly DD (2019) A potential role for the gut microbiome in substance use disorders. Psychopharmacology 236:1513–1530. https://doi.org/10.1007/s00213-019-05232-0
Bajaj JS, Sikaroodi M, Fagan A, Heuman D, Gilles H, Gavis EA, Fuchs M, Gonzalez-Maeso J, Nizam S, Gillevet PM, Wade JB (2019) Posttraumatic stress disorder is associated with altered gut microbiota that modulates cognitive performance in veterans with cirrhosis. Am J Physiol Gastrointest Liver Physiol 317:G661–G669. https://doi.org/10.1152/ajpgi.00194.2019
Xu M, Wang C, Krolick KN, Shi H, Zhu J (2020) Difference in post-stress recovery of the gut microbiome and its altered metabolism after chronic adolescent stress in rats. Sci Rep 10:3950. https://doi.org/10.1038/s41598-020-60862-1
Li Y, Hao Y, Fan F, Zhang B (2018) The role of microbiome in insomnia, circadian disturbance and depression. Front Psychiatry 9:669. https://doi.org/10.3389/fpsyt.2018.00669
Zhang J, Bi JJ, Guo GJ, Yang L, Zhu B, Zhan GF, Li S, Huang NN, Hashimoto K, Yang C, Luo AL (2019) Abnormal composition of gut microbiota contributes to delirium-like behaviors after abdominal surgery in mice. CNS Neurosci Ther 25:685–696. https://doi.org/10.1111/cns.13103
Saji N, Niida S, Murotani K, Hisada T, Tsuduki T, Sugimoto T, Kimura A, Toba K, Sakurai T (2019) Analysis of the relationship between the gut microbiome and dementia: a cross-sectional study conducted in Japan. Sci Rep 9:1008. https://doi.org/10.1038/s41598-018-38218-7
Angelucci F, Cechova K, Amlerova J, Hort J (2019) Antibiotics, gut microbiota, and Alzheimer's disease. J Neuroinflammation 16:108. https://doi.org/10.1186/s12974-019-1494-4
Adler CH, Beach TG (2016) Neuropathological basis of nonmotor manifestations of Parkinson's disease. Mov Disord 31:1114–1119. https://doi.org/10.1002/mds.26605
Hill-Burns EM, Debelius JW, Morton JT, Wissemann WT, Lewis MR, Wallen ZD, Peddada SD, Factor SA, Molho E, Zabetian CP, Knight R, Payami H (2017) Parkinson's disease and Parkinson's disease medications have distinct signatures of the gut microbiome. Mov Disord 32:739–749. https://doi.org/10.1002/mds.26942
Rinninella E, Raoul P, Cintoni M, Franceschi F, Miggiano GAD, Gasbarrini A, Mele MC (2019) What is the healthy gut microbiota composition? A changing ecosystem across age, environment, diet, and diseases. Microorganisms 7:14. https://doi.org/10.3390/microorganisms7010014
Kulkarni AS, Kumbhare SV, Dhotre DP, Shouche YS (2019) Mining the core gut microbiome from a sample Indian population. Indian J Microbiol 59:90–95. https://doi.org/10.1007/s12088-018-0742-0
Kumar R, Sood U, Gupta V, Singh M, Scaria J, Lal R (2020) Recent advancements in the development of modern probiotics for restoring human gut microbiome dysbiosis. Indian J Microbiol 60:12–25. https://doi.org/10.1007/s12088-019-00808-y
Naumova N, Alikina T, Tupikin A, Kalmykova A, Soldatova G, Vlassov V, Kabilov M (2020) Human gut microbiome response to short-term Bifidobacterium-based probiotic treatment. Indian J Microbiol. https://doi.org/10.1007/s12088-020-00888-1
Sarkar A, Lehto SM, Harty S, Dinan TG, Cryan JF, Burnet PWJ (2016) Psychobiotics and the manipulation of bacteria-gut-brain signals. Trends Neurosci 39:763–781. https://doi.org/10.1016/j.tins.2016.09.002
Barbosa RSD, Vieira-Coelho MA (2020) Probiotics and prebiotics: focus on psychiatric disorders—a systematic review. Nutr Rev 78:437–450. https://doi.org/10.1093/nutrit/nuz080
Ansari F, Pourjafar H, Tabrizi A, Homayouni A (2020) The effects of probiotics and prebiotics on mental disorders: a review on depression, anxiety, alzheimer, and autism spectrum disorders. Curr Pharm Biotechnol 21:555–565. https://doi.org/10.2174/1389201021666200107113812
Messaoudi M, Lalonde R, Violle N, Javelot H, Desor D, Nejdi A, Bisson JF, Rougeot C, Pichelin M, Cazaubiel M, Cazaubiel JM (2011) Assessment of psychotropic-like properties of a probiotic formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in rats and human subjects. Br J Nutr 105:755–764. https://doi.org/10.1017/S0007114510004319
Allen AP, Hutch W, Borre YE, Kennedy PJ, Temko A, Boylan G, Murphy E, Cryan JF, Dinan TG, Clarke G (2016) Bifidobacterium longum 1714 as a translational psychobiotic: modulation of stress, electrophysiology and neurocognition in healthy volunteers. Transl Psychiatry 6:e939. https://doi.org/10.1038/tp.2016.191
Steenbergen L, Sellaro R, van Hemert S, Bosch JA, Colzato LS (2015) A randomized controlled trial to test the effect of multispecies probiotics on cognitive reactivity to sad mood. Brain Behav Immun 48:258–264. https://doi.org/10.1016/j.bbi.2015.04.003
Akbari E, Asemi Z, Daneshvar Kakhaki R, Bahmani F, Kouchaki E, Tamtaji OR, Hamidi GA, Salami M (2016) Effect of probiotic supplementation on cognitive function and metabolic status in Alzheimer's disease: a randomized, double-blind and controlled trial. Front Aging Neurosci 8:256. https://doi.org/10.3389/fnagi.2016.00256
Tamtaji OR, Taghizadeh M, Daneshvar Kakhaki R, Kouchaki E, Bahmani F, Borzabadi S, Oryan S, Mafi A, Asemi Z (2019) Clinical and metabolic response to probiotic administration in people with Parkinson's disease: a randomized, double-blind, placebo-controlled trial. Clin Nutr 38:1031–1035. https://doi.org/10.1016/j.clnu.2018.05.018
Nimgampalle M, Kuna Y (2017) Anti-Alzheimer properties of probiotic, Lactobacillus plantarum MTCC 1325 in Alzheimer's disease induced albino rats. J Clin Diagn Res 11:KC01–KC05. https://doi.org/10.7860/JCDR/2017/26106.10428
Shaaban SY, El Gendy YG, Mehanna NS, El-Senousy WM, El-Feki HSA, Saad K, El-Asheer OM (2018) The role of probiotics in children with autism spectrum disorder: a prospective, open-label study. Nutr Neurosci 21:676–681. https://doi.org/10.1080/1028415X.2017.1347746
Liu J, Sun J, Wang F, Yu X, Ling Z, Li H, Zhang H, Jin J, Chen W, Pang M, Yu J, He Y, Xu J (2015) Neuroprotective effects of Clostridium butyricum against vascular dementia in mice via metabolic butyrate. Biomed Res Int 2015:412946. https://doi.org/10.1155/2015/412946
Kelly JR, Allen AP, Temko A, Hutch W, Kennedy PJ, Farid N, Murphy E, Boylan G, Bienenstock J, Cryan JF, Clarke G, Dinan TG (2017) Lost in translation? The potential psychobiotic Lactobacillus rhamnosus (JB-1) fails to modulate stress or cognitive performance in healthy male subjects. Brain Behav Immun 61:50–59. https://doi.org/10.1016/j.bbi.2016.11.018
Reininghaus EZ, Wetzlmair LC, Fellendorf FT, Platzer M, Queissner R, Birner A, Pilz R, Hamm C, Maget A, Koidl C, Riedrich K, Klampfer K, Ferk K, Dalkner N (2020) The impact of probiotic supplements on cognitive parameters in euthymic individuals with bipolar disorder: a pilot study. Neuropsychobiology 79:63–70. https://doi.org/10.1159/000492537
Zmora N, Zilberman-Schapira G, Suez J, Mor U, Dori-Bachash M, Bashiardes S, Kotler E, Zur M, Regev-Lehavi D, Brik RB, Federici S, Cohen Y, Linevsky R, Rothschild D, Moor AE, Ben-Moshe S, Harmelin A, Itzkovitz S, Maharshak N, Shibolet O, Shapiro H, Pevsner-Fischer M, Sharon I, Halpern Z, Segal E, Elinav E (2018) Personalized gut mucosal colonization resistance to empiric probiotics is associated with unique host and microbiome features. Cell 174:1388–1405.e21. https://doi.org/10.1016/j.cell.2018.08.041
Järbrink-Sehgal E, Andreasson A (2020) The gut microbiota and mental health in adults. Curr Opin Neurobiol 62:102–114. https://doi.org/10.1016/j.conb.2020.01.016
Godos J, Currenti W, Angelino D, Mena P, Castellano S, Caraci F, Galvano F, Del Rio D, Ferri R, Grosso G (2020) Diet and mental health: review of the recent updates on molecular mechanisms. Antioxidants (Basel) 9:346. https://doi.org/10.3390/antiox9040346
Acknowledgements
HV and CDR acknowledge Ramjas College, University of Delhi, Delhi, India for providing infrastructural support. SP thank Department of Biotechnology (DBT), Government of India for Junior Research Fellowship in a project. PL thank University Grants Commission (UGC), Government of India for Senior Research Fellowship. SS and RL thank The Energy and Resources Institute (TERI), New Delhi, India for providing infrastructure facilities. RL acknowledges The National Academy of Sciences, India (NASI) for support under the NASI-Senior Scientist Platinum Jubilee Fellowship Scheme.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Verma, H., Phian, S., Lakra, P. et al. Human Gut Microbiota and Mental Health: Advancements and Challenges in Microbe-Based Therapeutic Interventions. Indian J Microbiol 60, 405–419 (2020). https://doi.org/10.1007/s12088-020-00898-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12088-020-00898-z