Abstract
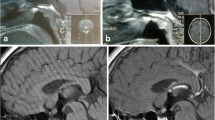
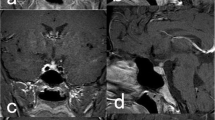
Langerhans cell histiocytosis (LCH) is a rare disease in which the most common endocrine manifestation is diabetes insipidus (DI). Data on anterior pituitary function in patients with LCH are limited. Thus, the present study investigated anterior pituitary function in LCH patients with DI via the evaluation of clinical and radiological findings at disease onset and during follow-up. The present study retrospectively evaluated nine patients with LCH (five males and four females). All diagnoses of LCH were made following histological and/or immunophenotypic analyses of tissue biopsies, bronchoalveolar lavage, or cerebrospinal fluid (CSF). Basal and, if necessary, dynamic pituitary function tests were used to assess anterior pituitary function, and magnetic resonance imaging (MRI) scans were used to image the pituitary. The LCH treatment modality was based on organ involvement. The mean age at onset of DI was 27.6 years (range 15–60 years). One patient (11 %) exhibited single organ involvement, while eight patients (89 %) displayed multisystem organ involvement. On admittance, one patient had hypogonadotropic hypogonadism, one patient exhibited panhypopituitarism [hypogonadotropic hypogonadism, central hypothyroidism, hypocortisolism, and growth hormone (GH) deficiency], and four patients (44 %) displayed hyperprolactinemia. The MRI data revealed infundibular enlargement in seven patients (78 %), a thalamic mass in one patient (11 %), and the absence of the bright spot in all patients. A single patient (11 %) showed a mass in the pons that had a partially empty sella. The patients were treated with radiation therapy (RT), chemotherapy (CT), or a combination of both (RT + CT) and were followed up for a median of 91.8 months (range 2–318 months). Seven patients were assessed during the follow-up period, of whom four patients (57.1 %) developed anterior pituitary hormone deficiency, three (43 %) were diagnosed with GH deficiency, and one (14 %) exhibited gonadotropin deficiency. The gonadotropin deficiency in the patient, which was diagnosed on admittance, was resolved during the follow-up period. DI persisted in all patients, and the conditions of the seven patients who have remained on follow-up are stable. In the present study, patients with LCH exhibited altered function in the anterior pituitary as well as the posterior pituitary, which may be due to the natural course of the disease or the effects of treatment. The present findings indicate that anterior pituitary function should be assessed in LCH patients on admittance and during follow-up, especially in LCH patients with multisystem organ involvement.




Similar content being viewed by others

References
L. Schmitz, B.E. Favara, Nosology and pathology of Langerhans cell histiocytosis. Hematol. Oncol. Clin. N. Am. 12, 221–246 (1998)
H. Stålemark, E. Laurencikas, J. Karis, D. Gavhed, B. Fadeel, J.I. Henter, Incidence of Langerhans cell histiocytosis in children: a population-based study. Pediatr. Blood Cancer. 51, 76–81 (2008)
J.S. Malpas, Langerhans cell histiocytosis in adults. Hematol. Oncol. Clin. N. Am. 12, 259–268 (1998)
I. Baumgartner, A. von Hochstetter, B. Baumert, U. Luetolf, F. Follath, Langerhans’-cell histiocytosis in adults. Med. Pediatr. Oncol. 28, 9–14 (1997)
M. Arico, R. Eceler, Clinical aspects of Langerhans cell histiocytosis. Hematol. Oncol. Clin. N. Am. 12, 247–258 (1998)
M. Arico, M. Girschikofsky, T. Généreau, C. Klersy, K. McClain, N. Grois, J.F. Emile, E. Lukina, E. De Juli, C. Danesino, Langerhans cell histiocytosis in adults. Report from the International Registry of the Histiocyte Society. Eur. J. Cancer 39, 2341–2348 (2003)
G. Badalian-Very, J.A. Vergillio, M. Fleming, B.J. Rollins, Pathogenesis of langerhans cell histiocytosis. Annu. Rev. Pathol. 24, 1–20 (2013)
P. Makras, K.I. Alexandraki, G.P. Chrousos, A.B. Grossman, G.A. Kaltsas, Endocrine manifestations in Langerhans cell histiocytosis. Trends Endocrinol. Metab. 18, 252–257 (2007)
D.B. Dunger, V. Broadbent, E. Yeoman, J.R. Seckle, S.L. Lightman, D.B. Grant, J. Pritchard, The frequency and natural history of diabetes insipidus in children with Langerhans-cell histiocytosis. N. Engl. J. Med. 321, 1157–1162 (1989)
N. Grois, B. Flucher-Wolfram, A. Heitger, G.H. Bostbeck, J. Hofmann, H. Gadner, Diabetes insipidus in Langerhans cell histiocytosis: results from the DAL-HX 83 study. Med. Pediatr. Oncol. 24, 248–256 (1995)
M.S. García Gallo, M.P. Martínez, M.S. Abalovich, S. Gutiérrez, M.A. Guitelman, Endocrine manifestations of Langerhans cell histiocytosis diagnosed in adults. Pituitary 13, 298–303 (2010)
V. Broadbent, D. Dunger, E. Yeomans, B. Kendall, Anterior pituitary function and computed tomography/magnetic resonance imaging in patients with Langerhans cell histiocytosis and diabetes insipidus. Med. Pediatr. Oncol. 21, 649–654 (1993)
P. Makras, C. Samara, M. Antoniou, A. Zetos, D. Papadogias, Z. Nikolakopoulou, E. Andreakos, G. Toloumis, G. Kontogeorgos, G. Piaditis, G.A. Kaltsas, Evolving radiological features of hypothalamo–pituitary lesions in adult patients with Langerhans cell histiocytosis (LCH). Neuroradiology 48, 37–44 (2006)
French Langerhans’ Cell Histiocytosis Group, A multicentric retrospective survey of Langerhans’ cell histiocytosis: 348 cases observed between 1983 and 1993. Arch. Dis. Child. 75, 17–24 (1996)
G.D. Braunstein, P.O. Kohler, Pituitary function in Hand–Schuller–Christian disease. N. Engl. J. Med. 286, 1225–1229 (1972)
B. Willis, A. Ablin, V. Weinberg, S. Zoger, W.M. Wara, K.K. Matthay, Disease course and late sequelae of Langerhans cell histiocytosis: 25-year experience at the University of California, San Francisco. J Clin. Oncol. 14, 2073–2082 (1996)
G.A. Kaltsas, Hypothalamo-pituitary abnormalities in adult patients with langerhans cell histiocytosis: clinical, endocrinological, and radiological features and response to treatment. J. Clin. Endocrinol. Metab 85, 1370–1376 (2000)
M.C. Amato, L.L. Elias, J. Elias, A.C. Santos, A.D. Bellucci, A.C. Moreira, M. De Castro, Endocrine disorders in pediatric—onset Langerhans Cell Histiocytosis. Horm. Metab. Res. 38, 746–751 (2006)
A.C. van den Hoek, A. Karstnes, R.M. Egeler, K. Hahlen, Growth of children with Langerhans cell histiocytosis. Eur. J. Pediatr. 154, 822–825 (1995)
H.J. Dean, A. Bishop, J.S.D. Winter, Growth hormone deficiency in patients with histiocytosis X. J. Pediatr. 109, 615–618 (1986)
H. Prosch, N. Grois, D. Prayer, F. Waldhauser, M. Steiner, M. Minkov, H. Gadner, Central diabetes insipidus as presenting symptom of Langerhans cell histiocytosis. Pediatr. Blood Cancer. 43, 594–599 (2004)
E. Mittheisz, R. Seidl, M. Waldenmair, M. Neophytou, U. Pötschger, M. Minkov, M. Steiner, H. Prosch, M. Wnorowski, H. Gadner, N. Grois, Central nervous system-related permanent consequences in patients with Langerhans cell histiocytosis. Pediatr. Blood Cancer 48, 50–56 (2007)
J. Donadieu, M.A. Rolon, C. Thomas, L. Brugieres, D. Plantaz, J.F. Emile, D. Frappaz, M. David, R. Brauner, T. Genereau, D. Debray, S. Cabrol, M.A. Barthez, K. Hoang-Xuan, M. Polak, French LCH Study Group, Endocrine involvement in pediatric-onset Langerhans’ cell histiocytosis: a population-based study. J. Pediatr. 144, 344–350 (2004)
V.R. Nanduri, P. Bareille, J. Pritchard, R. Stanhope, Growth and endocrine disorders in multisystem Langerhans’ cell histiocytosis. Clin. Endocrinol. (Oxf.) 53, 509–515 (2000)
Writing Group of the Histiocyte Society, Histiocytosis syndromes in children. Lancet 1, 208–209 (1987)
P.J. Trainer, G.M. Besser, The Bart’s endocrine protocols (Churchill-Livingstone, Edinburg, 1995)
M. Stockschlader, C. Sucker, Adult Langerhans cell histiocytosis. Eur. J. Haematol. 76, 363–368 (2006)
J.S. Malpas, A.J. Norton, Langerhans cell histiocytosis in the adult. Med. Pediatr. Oncol. 27, 540–546 (1996)
W.M. Yap, K.L. Chuah, P.H. Tan, Langerhans cell histiocytosis involving the thyroid and parathyroid glands. Mod. Pathol. 14, 111–115 (2001)
P.E. Coode, M.U. Shaikh, Histiocytosis X of the thyroid masquerading as thyroid carcinoma. Hum. Pathol. 19, 239–241 (1988)
S. Kitahama, M. Iitaka, T. Shimizu, N. Serizawa, N. Fukasawa, S. Miura, S. Kawasaki, K. Yamanaka, Y. Kawakami, S. Murakami, J. Ishii, S. Katayama, Thyroid involvement by malignant histiocytosis of Langerhans’ cell type. Clin. Endocrinol. (Oxf.) 45, 357–363 (1996)
R. Goyal, A. Das, R. Nijhawan, D. Bansal, R.K. Marwaha, Langerhans cell histiocytosis infiltration into pancreas and kidney. Pediatr. Blood Cancer. 49, 748–750 (2007)
R.D. Cone, M.J. Low, J.K. Elmquist, J.L. Cameron,: Neuroendocrinology. in Larsen P.R., Kronenberg H.M., Melmed S., Polonsky K.S. (eds) Williams Textbook of Endocrinology. (Elsevier Science, Philadelphia 2003) pp. 81–176
A. Vourtsi, A. Papadopoulos, L.A. Moulopoulos, J. Xenellis, L. Vlahos, Langerhans cell histiocytosis with involvement of the pons: case report. Neuroradiology 40, 161–163 (1998)
C.L. Teng, T.H. Lin, J.H. Young, G. Chou, C.S. Young, Rapidly fatal Langerhans’ cell histiocytosis in an adult. J. Formos. Med. Assoc. 104, 955–959 (2005)
K. Nagasaki, I. Tsumanuma, Y. Yoneoka, Y. Ogawa, T. Kikuchi, M. Uchiyama, Spontaneous regression of isolated neurohypophyseal langerhans cell histiocytosis with diabetes insipidus. Endocr. J. 56, 721–725 (2009)
D. Modan-Moses, M. Weintraub, J. Meyerovitch, G. Segal-Lieberman, B. Bielora, Hypopituitarism in langerhans cell histiocytosis: seven cases and literature review. J. Endocrinol. Invest. 24, 612–617 (2001)
J. Donadieu, M.A. Rolon, I. Pion, C. Thomas, F. Doz, M. Barkaoui, A. Robert, A. Deville, F. Mazingue, M. David, R. Brauner, S. Cabrol, C. Garel, M. Polak, French LCH Study Group, Incidence of growth hormone deficiency in pediatric-onset Langerhans cell histiocytosis: efficacy and safety of growth hormone treatment. J. Clin. Endocrinol. Metab. 89, 604–609 (2004)
R. Gramatovici, J.G. D’Angio, Radiation therapy in soft-tissue lesions in histiocytosis X (Langerhans cell histiocytosis). Med. Pediatr. Oncol. 16, 259–262 (1988)
B. Fahrner, H. Prosch, M. Minkov, M. Krischmann, H. Gadner, D. Prayer, N. Grois, Long-term outcome of hypothalamic pituitary tumors in Langerhans cell histiocytosis. Pediatr. Blood Cancer. 58, 606–610 (2012)
R. Haupt, V. Nanduri, M.G. Calevo, C. Bernstrand, J.L. Braier, B. Broadvent, G. Rey, K.L. McClain, G. Janka-Schaub, R.M. Egeler, Permanent consequences in Langerhans cell histiocytosis patients: a pilot study from the Histiocyte Society-Late Effects Study Group. Pediatr. Blood Cancer 42, 438–444 (2004)
R. Carpinteri, I. Patelli, F.F. Casanueva, A. Giustina, Pituitary tumors: inflammatory and granulomatous expansive lesions of the pituitary. Best Pract. Res. Clin. Endocrinol. Metab. 23, 639–650 (2009)
A.A. Toogood, Endocrine consequences of brain irradiation. Growth horm. IGF Res. 14, 1118–1124 (2004)
P. Makras, D. Papadogias, G. Kontogeorgos, G. Piaditis, G.A. Kaltsas, Spontaneous gonadotrophin deficiency recovery in an adult patient with Langerhans cell histiocytosis (LCH). Pituitary 8, 169–174 (2005)
N. Grois, D. Prayer, H. Prosch, M. Minkov, U. Pötschger, H. Gadner, Course and clinical impact of magnetic resonance imaging findings in diabetes insipidus associated with Langerhans cell histiocytosis. Pediatr. Blood Cancer 43, 59–65 (2004)
M. Maghnie, E. Genovese, M. Arico, A. Villa, G. Beluffi, R. Campani, F. Severi, Evolving pituitary hormone deficiency is associated with pituitary vasculopathy: dynamic MR study in children with hypopituitarism, diabetes insipidus and Langerhans cell histiocytosis. Radiology. 193, 493–499 (1994)
P. Sclozzi, T. Lombardi, P. Monnier, B. Jaques, Multisystem Langerhans cell histiocytosis (Hand–Schüller–Christian disease) in an adults: a case report and review of the literature. Eur. Arch. Otorhinolaryngol. 261, 326–330 (2004)
W.A. Scherbaum, J.A. Wass, G.M. Besser, G.F. Bottazzo, D. Doniach, Autoimmune cranial diabetes insipidus: its association with other endocrine diseases and with histiocytosis X. Clin. Endocrinol. (Oxf.) 25, 411–420 (1986)
C.E. Allen, K.L. McClain, Langerhans cell histiocytosis: a review of past, current and future therapy. Drugs Today (Barc.) 43, 627–643 (2007)
B. Ng-Cheng-Hin, C. O’Hanlon-Brown, C. Alifrangis, J. Waxman, Langerhans cell histiocytosis: old disease new treatment. QJM 104, 89–96 (2011)
O. Abla, R.M. Egeler, S. Weitzman: Langerhans cell histiocytosis: current concepts and treatments. Cancer Treat. Rev. 36, 354–359 (2010)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kurtulmus, N., Mert, M., Tanakol, R. et al. The pituitary gland in patients with Langerhans cell histiocytosis: a clinical and radiological evaluation. Endocrine 48, 949–956 (2015). https://doi.org/10.1007/s12020-014-0408-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-014-0408-6