Abstract
Background
Hip dislocation after treatment of a femoral neck fracture with a hemiarthroplasty remains an important problem in the treatment of hip fractures, but the associations between patient factors and surgical factors, and how these factors contribute to dislocation in patients who have undergone bipolar hemiarthroplasty through an anterolateral approach for femoral neck fracture currently are only poorly characterized.
Questions/purposes
We evaluated patients with bipolar hemiarthroplasty dislocation after surgery for femoral neck fracture treated through an anterolateral approach and asked: (1) What are the frequency, characteristics, and risk factors of bipolar hemiarthroplasty dislocations? (2) What are the frequency, characteristics, and risk factors of bipolar hemiarthroplasty dissociations?
Methods
A review of hospital records for patients who underwent bipolar hip hemiarthroplasty for femoral neck fracture at one hospital between July 2004 and August 2014 was conducted. During that time, 1428 patients were admitted with a diagnosis of femoral neck fracture; 508 of these patients underwent bipolar hip hemiarthroplasty, of whom 61 died and 23 were lost to followup during the first year, leaving 424 (83%) available for analysis. The remainder of the patients during that time were treated with internal fixation (512), unipoloar hip arthroplasty (17), or THA (391). For each patient with dislocation, we selected five control patients from the cohort according to sex, age (± 3 years), and year of entry in the study to eliminate some confounding factors. We recorded patient characteristics regarding demographics, medical comorbidities, Katz score, American Society of Anesthesiologists score, Mini-Mental State Examination (MMSE) score, and anesthesia type. Medical comorbidities included diabetes, chronic pulmonary disease, heart disease, neuromuscular diseases, and dementia. Univariate analyses were used to search for possible risk factors. Conditional logistic regression analyses on dislocation or dissociation were performed to estimate hazard rates (HRs) and corresponding 95% CIs with covariates of a probability less than 0.1 in univariate analysis.
Results
In this cohort, there were 26 dislocations including four that were also dissociations. The proportion of patients experiencing a dislocation was 6% (26 of 424). The mean interval from surgery to dislocation was 56 weeks (range, 0–433 weeks), and 18 dislocations (69%) occurred within 3 months after surgery. Three variables were independently associated with an increased risk of hip dislocation: dementia (HR, 3.51; 95% CI, 1.19–10.38; p = 0.02), discrepancy of offset (HR, 1.72; 95% CI, 1.15–2.58; p = 0.008), and lower MMSE score (HR, 0.93; 95% CI, 0.88–0.98; p = 0.007). The proportion of patients experiencing a dissociation was 0.9% (four of 424). The result of conditional logistic regression for dissociation showed that cup size smaller than 43 mm was the risk factor (HR = 513.05). However, there was no statistical difference with the probability equaling 0.47.
Conclusions
After the anterolateral approach for treatment of femoral neck fracture using bipolar hemiarthroplasty, 6% of hips dislocated and 0.9% experienced dissociation. Cognitive dysfunction and discrepancy of offset were independent risk factors associated with an increased risk of prosthetic dislocation. The small cup without a safety ring may be the risk factor of dissociation. Discrepancy of offset should be avoided during the operation by performing an accurate femoral osteotomy and choosing an adequate femoral stem neck length. For patients with cognitive dysfunction and a small cup, suturing the joint capsule during the operation and reinforcing protective measures after surgery might reduce the occurrence of dislocation and dissociation, however a study addressing this is necessary to confirm this.
Level of Evidence
Level III, therapeutic study.
Similar content being viewed by others
Introduction
Dislocation of a bipolar hemiarthroplasty in a patient who received the implant to treat a hip fracture can be devastating [5, 18]. The reported dislocation incidence of bipolar hemiarthroplasty ranges from 1.5% to 11% and may be associated with patient- and operation-related factors [1, 17, 22].
However, the available evidence on the factors contributing to dislocation in patients who have undergone bipolar hemiarthroplasty is limited. A large registry study with unadjusted covariates found a high prevalence of preoperative neurologic conditions in patients who experienced dislocation after bipolar arthroplasty [22]. Another large registry study reported that using the posterior surgical approach increased the risk of reoperation as a result of dislocation in elderly patients with hip fracture [20], however, this study did not distinguish between unipolar and bipolar hemiarthroplasties. Another study showed that postoperative global femoral offset and limb length discrepancy were risk factors for prosthetic dislocation after hemiarthroplasty through the posterolateral approach for femoral neck fracture [17]. None of these previous studies examined risk factors for bipolar hemiarthroplasty dislocation after surgery for femoral neck fracture through an anterolateral approach; in addition, there is no evidence available, to our knowledge, regarding the associations between patient factors and surgical factors and how these predisposing factors contribute to dislocation.
Dissociation was a special type of dislocation after bipolar hemiarthroplasty, in which the femoral stem and head components separate after dislocation. We found little information regarding this rare and serious complication except for a few case reports [4, 7, 8, 13, 16].
We therefore evaluated patients with bipolar hemiarthroplasty dislocation after surgery for femoral neck fracture through an anterolateral approach and asked: (1) What are the frequency, characteristics, and risk factors of bipolar hemiarthroplasty dislocations? (2) What are the frequency, characteristics, and risk factors of bipolar hemiarthroplasty dissociations?
Patients and Methods
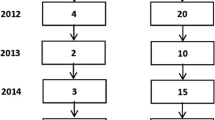
This study was approved by the research and ethics committee of the PLA Army General Hospital. The cohort for this retrospective nested case-control study consisted of every bipolar hip hemiarthroplasty performed to treat femoral neck fracture at the department of orthopaedics of a general hospital between July 2004 and August 2014. This analysis considered only patients older than 60 years. During the study period, patients with stable hip fractures (Garden Grade I or II) were treated with internal fixation (512), and patients with unstable hip fractures were treated with arthroplasty. In general, patients who could walk independently before injury and who could tolerate the slightly larger procedure underwent THA (391), whereas the remainder underwent hemiarthroplasty (525). Early during this period, unipolar arthroplasties were performed sporadically (17); these patients were excluded from this study, leaving 508 patients for consideration. Of those, 61 died and 23 were lost to followup during the first year, leaving 424 patients (83%) available for analysis in this report (Fig. 1).
Dislocation occurred in 26 patients treated with bipolar hemiarthroplasty and four with dissociation (Table 1). We chose a 10-year period (2004–2014) to obtain a recent sample of patients with a large enough sample to include an adequate number of patients with hemiarthroplasty dislocation.
The inclusion criteria were age 61 to 99 years, primary diagnosis of femoral neck fracture at admission, and surgical repair of fracture with bipolar hip hemiarthroplasty. The exclusion criteria were serious physical disease such as a tumor during the past 6 months and hip fractures that were treated with a unipolar hemiarthroplasty. The mean duration of followup was 4 years (range, 1–10 years).
Bipolar hip hemiarthroplasty was performed using an anterolateral approach modified from the Hardinge approach. Patients were positioned in a lateral decubitus position. An oblique incision of approximately 6 cm was made over the greater trochanter region; the angle between the direction of the incision and the axis of the femoral shaft was approximately 45°. The subcutis and fascia lata were incised parallel to the skin incision, and the gluteus medius were split between the anterior third and posterior two-thirds along the line of their fibers. The anterior third of the gluteus medius was stripped from the greater trochanter. The joint capsule was exposed and routinely excised, and the femoral head was removed. The choice of cemented prostheses (270 patients) or cementless prostheses (154 patients) depended on the bone mass of the proximal femur. After the bipolar hemiarthroplasty prosthesis was implanted, the gluteus medius was reattached through drilling holes on greater trochanteric bone using nonabsorbable Ethibond Excel® suture (Ethicon, Bridgewater, NJ, USA). We did not remove the labrum or repair the hip capsule. The fascia was closed, and the skin was stapled.
All patients had rehabilitation under the guidance of a physiotherapist, with weightbearing being introduced gradually after surgery. Patients were mobilized with two crutches during the first month after surgery. All patients were instructed to restrain hip ROM to less than 90° flexion and 45° rotation and to avoid adduction of the hip. All patients had standard AP and lateral radiographs taken postoperatively and were followed up for at least 1 year.
The nested case-control study often is used when the outcome is rare and the exposure of interest is difficult to obtain, and some number of control patients are selected for each patient from that case’s matched risk set in a cohort. For each patient with dislocation, we selected five control patients from the cohort according to sex, age (± 3 years), and year of entry in the study to eliminate some confounding factors. We recorded patient characteristics regarding demographics, medical comorbidities, Katz score, American Society of Anesthesiologists (ASA) score, Mini-Mental State Examination (MMSE) score, and anesthesia type. Medical comorbidities included diabetes, chronic pulmonary disease, heart disease (myocardial infarction, congestive heart failure), neuromuscular diseases (cerebral infarction, Parkinson’s disease), and dementia.
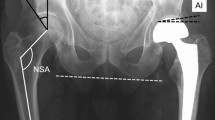
The Katz score is a simplified graded scale of the Index of Independence in Activities of Daily Living in the areas of bathing, dressing, toileting, transferring, continence, and feeding with the total score ranging from zero to six [12]. The ASA score was used to measure the severity of the patients’ health problems at admission. The MMSE was used to determine the patients’ cognitive level. Anesthesia type was divided into general or regional anesthesia. Surgical characteristics included prosthesis type, cup size, and discrepancy of limb length and offset. The Vario-Cup (LubinusTM SPII®, Link®; Waldemar Link, Hamburg, Germany) was used and the prosthesis type was divided into cemented (270 patients) or uncemented (154 patients) stems. Patients were classified in two groups on the basis of the diameter of the outer bearing of the bipolar prosthesis: small cup (< 43 mm) and normal cup (≥ 43 mm), because there is no safety ring between the outer head and the inner head in the small cup. Discrepancy of limb length was measured as the difference in perpendicular distance between the top of the lesser trochanter to the line passing through the lower edge of the teardrop points, and discrepancy of offset was the difference in the distance between the longitudinal axis of the femur to the center of the femoral head [17]. The research endpoint was dislocation of the bipolar hip hemiarthroplasty.
Statistical analyses were performed using a statistical software package (IBM SPSS Statistics for Windows, Version 20.0; IBM Corp, Armonk, NY, USA). Standard descriptive statistics were calculated including frequencies, percentages, means, and SD. The cohort was converted to nested case-control data based on a 1:5 ratio. Univariate analyses were used to search for possible risk factors. Conditional logistic regression analyses on dislocation or dissociation were performed to estimate hazard rates (HRs) and corresponding 95% CIs with covariates of p less than 0.1 in univariate analysis.
Results
Dislocation
A total of 26 (seven men, 19 women) of the 424 patients available at 1 year or greater experienced dislocation (6%) (Fig. 2) including four of which also were dissociations. The mean age of these patients was 81 ± 6 years (Table 2). The mean interval from surgery to dislocation was 56 weeks (range, 0–433 weeks), and 18 dislocations (69%) occurred within 3 months after surgery. Fourteen patients (54%) sustained recurrent dislocations. The mechanism leading to dislocation in 21 patients (81%) was atraumatic, and the other five (19%) were the result of falls. Anterior dislocations (21 patients; 81%) accounted for the majority.
Univariate analyses were performed (Appendix 1. Supplemental material is available with the online version of CORR®.). After controlling for relevant confounding variables, we found that decreasing Katz score, decreasing MMSE score, neuromuscular disease, dementia, cup size smaller than 43 mm, greater leg length difference, and greater offset difference were associated with an increased risk of dislocation. Conditional logistic regression was performed with these covariates of p less than 0.1 in univariate analysis to estimate HRs and 95% CIs.
Because dementia and MMSE were factors reflecting cognitive function in the elderly, we did not include the two variables in conditional logistic regression simultaneously. First, the six variables (decreasing Katz score, neuromuscular disease, dementia, cup size smaller than 43 mm, greater leg length difference, and greater offset difference) excluding the MMSE, were included in the conditional logistic regression and the result showed that two variables were independently associated with an increased risk of hip dislocation: dementia (HR, 3.51; 95% CI, 1.19–10.38; p = 0.02) and discrepancy of offset (HR, 1.72; 95% CI, 1.15–2.58; p = 0.008). Sensitivity analysis was performed with the MMSE score as an alternative to dementia; the results showed that lower MMSE score was independently associated with an increased risk of hip dislocations (HR, 0.93; 95% CI, 0.88–0.98; p = 0.007) whereas discrepancy of offset remained fairly constant (HR, 1.74; 95% CI, 1.16–2.60; p = 0.007) (Table 3).
Dissociations
The proportion of patients who experienced bipolar dissociations was 0.9% (four of 424), including one man and three women with a mean age of 83 ± 6 years (Fig. 3). All patients with dissociation underwent open reduction. Among the patients with dissociations, there were two with a cup size smaller than 43 mm (50%), one with dementia (25%), and one with neuromuscular disease (25%). The result of the conditional logistic regression performed with the covariates of Katz score, MMSE score, neuromuscular disease, dementia, cup size smaller than 43 mm, leg length difference, and offset difference showed that cup size smaller than 43 mm was the risk factor of dissociation (HR = 513.05). However, there was no statistical difference (p = 0.47) (Table 3).
Discussion
The bipolar hemiarthroplasty has been used to treat displaced femoral neck fractures in older patients, and it has been reported to provide patients with pain relief, functional improvement, and low revision rate [10, 21]. Dislocation and dissociation are relatively uncommon but devastating complications. To the best of our knowledge, there are no published studies examining risk factors for bipolar hemiarthroplasty dislocation and dissociation after surgery for femoral neck fracture through an anterolateral approach. This retrospective nested case-control study showed that approximately 6% of patients treated with bipolar hip hemiarthroplasty through an anterolateral approach for femoral neck fracture experienced dislocation of the hip at some point after the procedure, and approximately 0.9% experienced a prosthetic dissociation. Cognitive dysfunction and discrepancy of offset were associated with an increased risk of prosthetic dislocation; other factors such as age, sex, anesthesia type, prosthesis type, cup size, and other comorbidities such as diabetes, chronic obstructive pulmonary disease, and heart disease were not.
Our study has some limitations. Selection bias in the choice of control subjects was inevitable in the process of selecting the control group according to sex, age, and year of entry in the study for each patient with dislocation. All procedures were done by two high-volume surgeons (ZL and TS), therefore our results might underestimate the overall proportion of dislocations. There also was selection bias in that younger, healthier patients were treated primarily with other methods such THA. Our findings related to less-active, less-healthy patients. We could not standardize the postoperative radiographs for all patients, and we did not use the blind method for patients versus control subjects when measuring leg length discrepancy length and discrepancy of offset, which would bring measurement error to the study. There was a selection bias owing to the high number of patients lost to followup, therefore the cumulative incidence of dislocation might be different from the rate indicated. This study lacked information regarding other risk factors for hip dislocation, including rotation of the prosthesis and fall risk score. The results of the study therefore should be interpreted cautiously.
We found that the proportion of bipolar hemiarthroplasty prostheses that dislocated was 6% in our patients. We defined dislocation as the prosthetic femoral head component coming out of the acetabulum, whereas dissociation refers to uncoupling of the modular femoral head from the femoral stem (which also usually is associated with a dislocation). These are major complications of hip arthroplasty performed on patients with displaced femoral neck fractures [1, 22]. The posterior surgical approach clearly increases the risk of dislocation, as supported by several clinical studies on patients with hip fracture [6, 19, 20]. Enocson et al. [6] reported a higher dislocation proportion of 13% using the posterolateral approach than the 3% with the anterolateral approach in 720 patients with femoral neck fractures, and Pajarinen et al. [19] reported a 16% dislocation rate after surgery through the posterior approach compared with 7% after the anterior approach in 338 hip fracture surgeries. The proportion of dislocations in the 508 patients in our study after surgery through the anterolateral approach was 6%, which was less than the 11% dislocation rate reported after surgery through the posterior approach in another recent cohort study [17].
We found that cognitive decline, including dementia and lower MMSE score, was associated with an increased risk of hip dislocations. It was difficult to maintain patients with impaired cognitive function in a suitable posture postoperatively, which may have led to dislocation of the hip during the early postoperative period [2]. In the current study, another factor significantly associated with an increased risk of hip dislocation was discrepancy of offset; this could give rise to poor soft tissue tension and therefore contribute to the increased risk of dislocation. Other studies have found that lower offset was a risk factor for dislocation of unipolar hemiarthroplasty prostheses [14, 18]. Mukka et al. [17] reported that patients with single dislocations had no difference in postoperative femoral offset compared with age- and sex-matched control subjects, but there was a smaller femoral offset compared with offset in the patients with recurrent dislocations. Neurologic impairment affects the position of the hip in the resting state and leads to hip imbalance owing to paresis, spasticity, contractures, or tremors [9]. Some studies have suggested that these patients had high risks of hip dislocation ranging from 11% to 45% after bipolar hemiarthroplasty for hip fracture [3, 22, 24]. In contrast, Suh et al. [23] and we observed similar proportions of dislocation in patients with and without neuromuscular disease, but their study and our study might lack enough patients with neuromuscular conditions to really test the question with adequate statistical power.
The proportion of our patients experiencing a dissociation was 0.9%. Dissociation must be treated with open reduction. Dissociation is rare and has been reported in only a few case reports [4, 7, 8, 13, 16]. The reasons for disassociation after hemiarthroplasty have been reported as component selection and alignment, surgical technique, and patient factors [4, 7, 8, 11, 13, 15, 16]. Varley and Parker [25] reported that dissociations accounted for 12% of all dislocations in bipolar prostheses. We found that 15% (four of 26) of all dislocations also were dissociations, and two of the four dissociations were in patients with small cups (50%; HR = 513) that had no safety ring between the outer and inner head. The number of dissociations was too small to do a statistical analysis of risk factors.
After the anterolateral approach for treatment of femoral neck fractures using bipolar hemiarthroplasty, 6% of hips dislocated, and 0.9% experienced dissociation. Cognitive dysfunction and discrepancy of offset were independent risk factors significantly associated with an increased risk of prosthetic dislocation. The small cup without a safety ring may be the risk factor of dissociation. Discrepancy of offset should be avoided during the operation by performing an accurate femoral osteotomy and choosing an adequate femoral stem neck length. For patients with cognitive dysfunction and a small cup, suturing the joint capsule during surgery and reinforcing protective measures after surgery might reduce the occurrence of dislocation and dissociation, but further study is necessary to confirm this contention.
References
Barnes CL, Berry DJ, Sledge CB. Dislocation after bipolar hemiarthroplasty of the hip. J Arthroplasty. 1995;10:667–669.
Bliemel C, Lechler P, Oberkircher L, Colcuc C, Balzer-Geldsetzer M, Dodel R, Ruchholtz S, Buecking B. Effect of preexisting cognitive impairment on in-patient treatment and discharge management among elderly patients with hip fractures. Dement Geriatr Cogn Disord. 2015;40:33–43.
Coughlin L, Templeton J. Hip fractures in patients with Parkinson’s disease. Clin Orthop Relat Res. 1980;148:192–195.
Ellanti P, Bahari S, McCarthy T. Significantly displaced femoral head component in a dissociated bipolar hip hemiarthroplasty. Orthop Surg. 2012;4:194–196.
Enocson A, Pettersson H, Ponzer S, Tornkvist H, Dalen N, Tidermark J. Quality of life after dislocation of hip arthroplasty: a prospective cohort study on 319 patients with femoral neck fractures with a one-year follow-up. Qual Life Res. 2009;18:1177–1184.
Enocson A, Tidermark J, Tornkvist H, Lapidus LJ. Dislocation of hemiarthroplasty after femoral neck fracture: better outcome after the anterolateral approach in a prospective cohort study on 739 consecutive hips. Acta Orthop. 2008;79:211–217.
Georgiou G, Siapkara A, Dimitrakopoulou A, Provelengios S, Dounis E. Dissociation of bipolar hemiarthroplasty of the hip after dislocation: a report of five different cases and review of literature. Injury. 2006;37:162–168.
Guo JJ, Yang H, Yang T, Tang T. Disassembly of cemented bipolar prothesis of the hip. Orthopedics. 2008;31:813.
Han SK, Kim YS, Kang SH. Treatment of femoral neck fractures with bipolar hemiarthroplasty using a modified minimally invasive posterior approach in patients with neurological disorders. Orthopedics. 2012;35:e635–640.
Inngul C, Hedbeck CJ, Blomfeldt R, Lapidus G, Ponzer S, Enocson A. Unipolar hemiarthroplasty versus bipolar hemiarthroplasty in patients with displaced femoral neck fractures: a four-year follow-up of a randomised controlled trial. Int Orthop. 2013;37:2457–2464.
Kanda A, Kaneko K, Obayashi O, Mogami A. A 42-year-old patient presenting with femoral head migration after hemiarthroplasty performed 22 years earlier: a case report. J Med Case Rep. 2015;9:17.
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged: the index of ADL: A standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919.
Lee HH, Lo YC, Lin LC, Wu SS. Disassembly and dislocation of a bipolar hip prosthesis. J Formos Med Assoc. 2008;107:84–88.
Madanat R, Makinen TJ, Ovaska MT, Soiva M, Vahlberg T, Haapala J. Dislocation of hip hemiarthroplasty following posterolateral surgical approach: a nested case-control study. Int Orthop. 2012;36:935–940.
Moores TS, Blackwell JR, Chatterton BD, Eisenstein N. Disassociation at the head-trunnion interface: an unseen complication of modular hip hemiarthroplasty. BMJ Case Rep. 2013; 2013. pii: bcr2013200387. doi:10.1136/bcr-2013-200387.
Moriarity A, Ellanti P, Talha S, McKenna J. Dislocation and dissociation of bipolar hip hemiarthroplasty. BMJ Case Rep. 2015; 2015. pii: bcr2015210282. doi:10.1136/bcr-2015-210282.
Mukka S, Lindqvist J, Peyda S, Broden C, Mahmood S, Hassany H, Sayed-Noor A. Dislocation of bipolar hip hemiarthroplasty through a postero-lateral approach for femoral neck fractures: a cohort study. Int Orthop. 2015;39:1277–1282.
Ninh CC, Sethi A, Hatahet M, Les C, Morandi M, Vaidya R. Hip dislocation after modular unipolar hemiarthroplasty. J Arthroplasty. 2009;24:768–774.
Pajarinen J, Savolainen V, Tulikoura I, Lindahl J, Hirvensalo E. Factors predisposing to dislocation of the Thompson hemiarthroplasty: 22 dislocations in 338 patients. Acta Orthop Scand. 2003;74:45–48.
Rogmark C, Fenstad AM, Leonardsson O, Engesaeter LB, Karrholm J, Furnes O, Garellick G, Gjertsen JE. Posterior approach and uncemented stems increases the risk of reoperation after hemiarthroplasties in elderly hip fracture patients. Acta Orthop. 2014;85:18–25.
Rogmark C, Leonardsson O. Hip arthroplasty for the treatment of displaced fractures of the femoral neck in elderly patients. Bone Joint J. 2016;98:291–297.
Sierra RJ, Schleck CD, Cabanela ME. Dislocation of bipolar hemiarthroplasty: rate, contributing factors, and outcome. Clin Orthop Relat Res. 2006;442:230–238.
Suh KT, Kim DW, Lee HS, Seong YJ, Lee JS. Is the dislocation rate higher after bipolar hemiarthroplasty in patients with neuromuscular diseases? Clin Orthop Relat Res. 2012;470:1158–1164.
Turcotte R, Godin C, Duchesne R, Jodoin A. Hip fractures and Parkinson’s disease: a clinical review of 94 fractures treated surgically. Clin Orthop Relat Res. 1990;256:132–136.
Varley J, Parker MJ. Stability of hip hemiarthroplasties. Int Orthop. 2004;28:274–277.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Li, L., Ren, J., Liu, J. et al. What Are the Risk Factors for Dislocation of Hip Bipolar Hemiarthroplasty Through the Anterolateral Approach? A Nested Case-control Study. Clin Orthop Relat Res 474, 2622–2629 (2016). https://doi.org/10.1007/s11999-016-5053-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-016-5053-3