Abstract
Purpose of Review
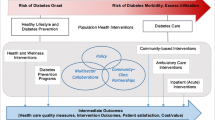
Community health centers (CHCs) provide care to millions of vulnerable patients in the USA, including a disproportionate number with diabetes. Policies affecting diabetes management in CHCs therefore have broad implications for clinical practice and patient outcomes nationwide. We describe prior policies that have influenced diabetes management in CHCs, discuss current policies and programs, as well as present emerging innovations and future directions for diabetes care in this setting.
Recent Findings
Domains for current diabetes policies and programs in CHCs include coverage requirements, quality reporting and incentives, prescription discounts, healthy behavior incentives, and team-based care. Policies in these areas affect the management of diabetes at multiple levels, from organizations that support CHCs to individual health centers, and the providers and patients based there.
Summary
Several domains of interrelated policies and programs impact CHC diabetes management at multiple levels. Stakeholders’ understanding of these policies and programs may identify opportunities to improve diabetes care.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP). National Diabetes Statistics Report, 2017. In: Division of Diabetes Translation Centers for Disease Control and Prevention 2019. https://www.cdc.gov/diabetes/data/statistics-report/index.html. Accessed October 29, 2019.
St Sauver JL, Warner DO, Yawn BP, Jacobson DJ, McGree ME, Pankratz JJ, et al. Why patients visit their doctors: assessing the most prevalent conditions in a defined American population. Mayo Clin Proc. 2013;88(1):56–67. https://doi.org/10.1016/j.mayocp.2012.08.020.
•• Health Centers are Providing Care to Growing Numbers of Patients with Complex Needs. National Association of Community Health Centers. 2019. http://www.nachc.org/wp-content/uploads/2019/05/Growth_in_Patients_with_Complex_Needs_5.30.19.pdf. Accessed October 29, 2019. This policy brief highlights the disproportionate share of diabetes care community health centers provide.
Saydah SH, Imperatore G, Beckles GL. Socioeconomic status and mortality: contribution of health care access and psychological distress among U.S. adults with diagnosed diabetes. Diabetes Care. 2013;36(1):49–55. https://doi.org/10.2337/dc11-1864.
Health Outcomes and Disparities. National Data. In: Health Center Program. Table 7. Health Resources and Services Adminstration (HRSA). 2018. https://bphc.hrsa.gov/uds/datacenter.aspx?q=t7&year=2018&state=&fd=. Accessed October 29, 2019.
Health Resources & Services Administration. Diabetes quality improvement initiative. HRSA Health Center Program. 2019. https://bphc.hrsa.gov/qualityimprovement/clinicalquality/diabetes.html. .
America’s Health Centers. National Association of Community Health Centers. 2019. http://www.nachc.org/wp-content/uploads/2019/07/Americas-Health-Centers-Final-8.5.19.pdf. Accessed October 29, 2019.
Richard P, Shin P, Beeson T, Burke LS, Wood SF, Rosenbaum S. Quality and cost of diabetes mellitus care in community health centers in the United States. PLoS One. 2015;10(12):e0144075. https://doi.org/10.1371/journal.pone.0144075.
Health Centers and Medicaid. In: Research Fact Sheets and Infographics. National Association of Community Health Centers. 2018. http://www.nachc.org/wp-content/uploads/2018/05/Medicaid_FS_5.15.18.pdf. Accessed October 29, 2019.
Downer S, Condra A, White KL, Shaw S, Myneni A, Leonce M et al. Beating type 2 diabetes: recommendations for Federal Policy Reform. Center for Health Law and Policy Innovation of Harvard Law School 2015. https://www.chlpi.org/wp-content/uploads/2014/01/PATHS-Beating-Type-2-Diabetes-Recommendations-for-Federal-Policy-Reform-Report_FINAL.pdf. .
Key Health Center Data by State, 2018. National Association of Community Health Centers. 2018. http://www.nachc.org/wp-content/uploads/2019/07/Key-Facts-By-State-2018-UDS-1.pdf. .
Health Insurance Coverage of the Total Population: 2017. The Henry J. Kaiser Family Foundation. 2019. https://www.kff.org/other/state-indicator/total-population/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. .
State Level Health Center Data. National Association of Community Health Centers. 2017. http://www.nachc.org/state-level-data-maps/. Accessed October 29, 2019.
Ku LC, Cunningham M, Goldberg DG, Darnell JS, Hiller M, Shin PH et al. Quality incentives for federally qualified health centers, rural health clinics and free clinics: a report to Congress. Department of Health Policy, School of Public Health and Health Services, The George Washington University. 2012. https://www.healthit.gov/sites/default/files/pdf/quality-incentives-final-report-1-23-12.pdf. .
Quatromoni PA, Milbauer M, Posner BM, Carballeira NP, Brunt M, Chipkin SR. Use of focus groups to explore nutrition practices and health beliefs of urban Caribbean Latinos with diabetes. Diabetes Care. 1994;17(8):869–73.
McCaughan M. The 340B drug discount program. Health Afffairs Health Policy Brief. 2017:1–4.
Community Health Center Revenues by Payer Source. The Henry J. Kaiser Family Foundation. 2017. https://www.kff.org/other/state-indicator/community-health-center-revenues-by-payer-source/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Accessed October 29, 2019.
https://bphc.hrsa.gov/uds/datacenter.aspx?q=t7&year=2018&state=&fd=. HRaSAHHCPTHOaDNDAa.
CDC. Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2014. Atlanta, GA: U.S. Department of Health and Human Services; 2014. 2014.
Health Resources & Services Administration. Communities of practice: health center controlled networks. U.S. Department of Health and Human Services https://www.hrsa.gov/sites/default/files/communitiesofpractice/AtaGlance/healthcenternetworks.pdf. .
Rosenbaum S, Tolbert J, Sharac J, Shin P, Gunsalus R, Zur J. Community health centers: growing importance in a changing health care system. In: Medicaid. The Henry J. Kaiser Family Foundation. 2018. https://www.kff.org/medicaid/issue-brief/community-health-centers-growing-importance-in-a-changing-health-care-system/. .
Chin MH, Cook S, Jin L, Drum ML, Harrison JF, Koppert J, et al. Barriers to providing diabetes care in community health centers. Diabetes Care. 2001;24(2):268–74. https://doi.org/10.2337/diacare.24.2.268.
Medicaid & CHIP. In: ADA Resources: Health Insurance. American Diabetes Association. 2019. https://www.diabetes.org/resources/health-insurance/medicaid-chip. Accessed August 15, 2019.
Medicare. In: ADA Resources: Health Insurance. American Diabetes Association. 2019. https://www.diabetes.org/resources/health-insurance/medicare. Accessed August 15, 2019.
Medicaid.gov. Mandatory & Optional Medicaid Benefits. In: Medicaid: Benefits. Centers for Medicare and Medicaid Services. 2019. https://www.medicaid.gov/medicaid/benefits/list-of-benefits/index.html. Accessed August 16, 2019.
Cauchi R, Mason K, Chung Y, Thangasamy A. Diabetes Health Coverage: State Laws and Programs. National Conference of State Legislatures. 2016. http://www.ncsl.org/research/health/diabetes-health-coverage-state-laws-and-programs.aspx#4. .
MLN Matters. Current Medicare coverage of diabetes supplies. U.S. Department of Health and Human Services. 2018. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/SE18011.pdf. .
Federally Qualified Health Centers (FQHC) Center: New FQHC Care Management Services. Centers for Medicare & Medicaid Services. 2018. https://www.cms.gov/Center/Provider-Type/Federally-Qualified-Health-Centers-FQHC-Center.html. Accessed August 15, 2019.
Evaluation Activities of the U.S. Department of Health and Human Services. In: Performance Improvement 2006. U.S. Department of Health and Human Services. 2006. https://aspe.hhs.gov/system/files/pdf/36416/pi_2006.pdf. Accessed October 29, 2019.
Shane-McWhorter L. Diabetes care in community health centers: a focus on health resources and services administration-funded clinical pharmacy demonstration projects. Diabetes Spectrum. 2006;19(3):141–4. https://doi.org/10.2337/diaspect.19.3.141.
House Committee on Energy & Commerce. Review of the 340B drug pricing program. U.S. House of Representatives. 2018. https://morningconsult.com/wp-content/uploads/2018/01/340B-Report20180111.pdf. Accessed October 29, 2019.
National Association of Community Health Centers. Chapter 9: Medicaid and 340B. NACHC 340B Manual for Health Centers, Second Edition. Accessed at https://hcpsocal.org/wp-content/uploads/2018/09/2nd-Edition-NACHC-340B-Manual-March-2018-FINAL.pdf: National Association of Community Health Centers; 2018.
Chin MH, Auerbach SB, Cook S, Harrison JF, Koppert J, Jin L, et al. Quality of diabetes care in community health centers. Am J Public Health. 2000;90(3):431–4. https://doi.org/10.2105/ajph.90.3.431.
Chin MH. Quality improvement implementation and disparities: the case of the health disparities collaboratives. Med Care. 2011;49(Suppl):S65–71. https://doi.org/10.1097/MLR.0b013e31823ea0da.
Huang ES, Zhang Q, Brown SE, Drum ML, Meltzer DO, Chin MH. The cost-effectiveness of improving diabetes care in U.S. federally qualified community health centers. Health Serv Res. 2007;42(6 Pt 1):2174–93; discussion 294-323. https://doi.org/10.1111/j.1475-6773.2007.00734.x.
Quality Improvement Awards (QIA). In: HRSA Program Opportunities. Health Resources and Services Administration. 2019. https://bphc.hrsa.gov/program-opportunities/funding-opportunities/quality. Accessed September 7, 2019.
Purnell JQ, Herrick C, Moreland-Russell S, Eyler AA. Outside the exam room: policies for connecting clinic to community in diabetes prevention and treatment. Prev Chronic Dis. 2015;12:E63. https://doi.org/10.5888/pcd12.140403.
Peek ME, Harmon SA, Scott SJ, Eder M, Roberson TS, Tang H, et al. Culturally tailoring patient education and communication skills training to empower African-Americans with diabetes. Transl Behav Med. 2012;2(3):296–308. https://doi.org/10.1007/s13142-012-0125-8.
Peek ME, Wilkes AE, Roberson TS, Goddu AP, Nocon RS, Tang H, et al. Early lessons from an initiative on Chicago’s South Side to reduce disparities in diabetes care and outcomes. Health Aff (Millwood). 2012;31(1):177–86. https://doi.org/10.1377/hlthaff.2011.1058.
Tung EL, Gunter KE, Bergeron NQ, Lindau ST, Chin MH, Peek ME. Cross-sector collaboration in the high-poverty setting: qualitative results from a community-based diabetes intervention. Health Serv Res. 2018;53(5):3416–36. https://doi.org/10.1111/1475-6773.12824.
Tricco AC, Ivers NM, Grimshaw JM, Moher D, Turner L, Galipeau J, et al. Effectiveness of quality improvement strategies on the management of diabetes: a systematic review and meta-analysis. Lancet. 2012;379(9833):2252–61. https://doi.org/10.1016/S0140-6736(12)60480-2.
Ali MK, Bullard KM, Saaddine JB, Cowie CC, Imperatore G, Gregg EW. Achievement of goals in U.S. diabetes care, 1999-2010. N Engl J Med. 2013;368(17):1613–24. https://doi.org/10.1056/NEJMsa1213829.
McMahon GT, Dluhy RG. Diabetes report card--time for a winning streak. N Engl J Med. 2013;368(17):1650–1. https://doi.org/10.1056/NEJMe1302610.
Stellefson M, Dipnarine K, Stopka C. The chronic care model and diabetes management in US primary care settings: a systematic review. Prev Chronic Dis. 2013;10:E26. https://doi.org/10.5888/pcd10.120180.
Zhang JX, Huang ES, Drum ML, Kirchhoff AC, Schlichting JA, Schaefer CT, et al. Insurance status and quality of diabetes care in community health centers. Am J Public Health. 2009;99(4):742–7. https://doi.org/10.2105/AJPH.2007.125534.
Li V, McBurnie MA, Simon M, Crawford P, Leo M, Rachman F, et al. Impact of social determinants of health on patients with complex diabetes who are served by national safety-net health centers. J Am Board Fam Med. 2016;29(3):356–70. https://doi.org/10.3122/jabfm.2016.03.150226.
Jackson GL, Powers BJ, Chatterjee R, Bettger JP, Kemper AR, Hasselblad V, et al. The patient centered medical home. A systematic review. Ann Intern Med. 2013;158(3):169–78. https://doi.org/10.7326/0003-4819-158-3-201302050-00579.
FQHC Advanced Primary Care Practice Demonstration. In: Innovation models. Centers for Medicare and Medicaid Services, Accessed at https://innovation.cms.gov/initiatives/fqhcs/. 2019. https://innovation.cms.gov/initiatives/fqhcs/. .
Cykert S, Lefebvre A, Bacon T, Newton W. Meaningful use in chronic care: improved diabetes outcomes using a primary care extension center model. N C Med J. 2016;77(6):378–83. doi:https://doi.org/10.18043/ncm.77.6.378.
Cebul RD, Love TE, Jain AK, Hebert CJ. Electronic health records and quality of diabetes care. N Engl J Med. 2011;365(9):825–33. https://doi.org/10.1056/NEJMsa1102519.
Duffy L. “Step-by-step we are stronger”: women’s empowerment through photovoice. J Community Health Nurs. 2011;28(2):105–16. https://doi.org/10.1080/07370016.2011.564070.
Laws R, Gillespie S, Puro J, Van Rompaey S, Quach T, Carroll J et al. The Community Health Applied Research Network (CHARN) data warehouse: a resource for patient-centered outcomes research and quality improvement in underserved, safety net populations. EGEMS (Wash DC). 2014;2(3):1097. doi:https://doi.org/10.13063/2327-9214.1097.
Mayer KH, Loo S, Crawford PM, Crane HM, Leo M, DenOuden P, et al. Excess clinical comorbidity among HIV-infected patients accessing primary care in US community health centers. Public Health Rep. 2018;133(1):109–18. https://doi.org/10.1177/0033354917748670.
Uniform Data System (UDS) Resources: 2020. In: Health center data. Health Resources & Services Administration 2019. https://bphc.hrsa.gov/sites/default/files/bphc/datareporting/pdf/2020-uds-proposed-pal-oqi.pdf. .
Comprensive Diabetes Care (CDC). In: HEDIS Measures and Technical Resources. National Committee for Quality Assurance. 2018. https://www.ncqa.org/hedis/measures/comprehensive-diabetes-care/. Accessed October 29, 2019.
CDC’s Funded Programs to Address Diabetes. In: State, Local, and National Partner Diabetes Programs. Centers for Disease Control and Prevention. 2019. https://www.cdc.gov/diabetes/programs/stateandlocal/cdcfunded.html. Accessed September 20, 2019.
Contreary K, Miller R. Incentives to change health behaviors: beneficiary engagement strategies in Indiana, Iowa, and Michigan. U.S. Department of Health and Human Services, Centers for Medicare and Medicaid Services. 2017. https://www.medicaid.gov/medicaid/section-1115-demo/downloads/evaluation-reports/incentives-to-change-health-behaviors.pdf. .
Askelson NM, Wright B, Bentler S, Momany ET, Damiano P. Iowa’s Medicaid expansion promoted healthy behaviors but was challenging to implement and attracted few participants. Health Aff (Millwood). 2017;36(5):799–807. https://doi.org/10.1377/hlthaff.2017.0048.
Goold SD, Tipirneni R, Kieffer E, Haggins A, Salman C, Solway E, et al. Primary care clinicians’ views about the impact of Medicaid expansion in Michigan: a mixed methods study. J Gen Intern Med. 2018;33(8):1307–16. https://doi.org/10.1007/s11606-018-4487-6.
The Use of Healthy Behavior Incentives in Medicaid. Medicaid and CHIP Payment and Access Commission, MACPAC. 2016. https://www.macpac.gov/publication/the-use-of-healthy-behavior-incentives-in-medicaid/. Accessed October 29, 2019.
Van Vleet A, Rudowitz R. An overview of Medicaid Incentives for the Prevention of Chronic Diseases (MIPCD) Grants. The Henry J. Kaiser Family Foundation, The Kaiser Commission on Medicaid and the Uninsured. 2014. https://www.kff.org/medicaid/issue-brief/an-overview-of-medicaid-incentives-for-the-prevention-of-chronic-diseases-mipcd-grants/. .
Saunders R, Vulimiri M, Japinga M, Bleser W, Wong C. Are carrots good for your health? Current evidence on health behavior incentives in the Medicaid Program. Margolis Center for Health Policy, Duke University. 2018. https://healthpolicy.duke.edu/sites/default/files/atoms/files/duke_healthybehaviorincentives_6.1.pdf.
Kelley AT, Goold SD, Ayanian JZ, Patel M, Zhang E, Beathard E et al. Engagement with Health Risk Assessments and Commitment to Healthy Behaviors in Michigan's Medicaid Expansion Program. J Gen Intern Med. 2019. https://doi.org/10.1007/s11606-019-05562-x
Yue D, Pourat N, Chen X, Lu C, Zhou W, Daniel M, et al. Enabling services improve access to care, preventive services, and satisfaction among health center patients. Health Aff (Millwood). 2019;38(9):1468–74. https://doi.org/10.1377/hlthaff.2018.05228.
Dobbins JM, Peiper N, Jones E, Clayton R, Peterson LE, Phillips RL Jr. Patient-centered medical home recognition and diabetes control among health centers: exploring the role of enabling services. Popul Health Manag. 2018;21(1):6–12. https://doi.org/10.1089/pop.2017.0001.
Beck J, Greenwood DA, Blanton L, Bollinger ST, Butcher MK, Condon JE, et al. 2017 National Standards for diabetes self-management education and support. Diabetes Educ. 2019;45(1):34–49. https://doi.org/10.1177/0145721718820941.
National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP). Emerging practices in diabetes prevention and control: Medicaid coverage for diabetes self-management education. Centers for Disease Control and Prevention. 2016. https://www.cdc.gov/diabetes/pdfs/programs/stateandlocal/emerging_practices-dsme.pdf. Accessed October 29, 2019.
Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, Fischl AH, et al. Diabetes self-management education and support in type 2 diabetes. Diabetes Educ. 2017;43(1):40–53. https://doi.org/10.1177/0145721716689694.
Center for Surveillance E, and Laboratory Services (CSELS),. Providing diabetes self-management education and support for rural Americans. Centers for Disease Control and Prevention. 2018. https://www.cdc.gov/ruralhealth/diabetes/policybrief.html. Accessed October 29, 2019.
National Institute of Diabetes and Digestive and Kidney Diseases. Community partnerships. In: Diabetes practice changes: tools and strategies. National Institutes of Health. 2019. https://www.niddk.nih.gov/health-information/communication-programs/ndep/health-professionals/practice-transformation-physicians-health-care-teams/diabetes-practice-changes/community-partnerships. Accessed August 15, 2019.
Barbero C, Gilchrist S, Chriqui JF, Martin MA, Wennerstrom A, VanderVeur J, et al. Do state community health worker Laws align with best available evidence? J Community Health. 2016;41(2):315–25. https://doi.org/10.1007/s10900-015-0098-x.
Allen NA, Zagarins S, Welch G. Reducing social distress for chronic disease patients in primary care: an intervention for Latino type 2 diabetes patients seen at community health centers. Diabetes Spectr. 2017;30(4):288–96. https://doi.org/10.2337/ds16-0031.
Kane EP, Collinsworth AW, Schmidt KL, Brown RM, Snead CA, Barnes SA, et al. Improving diabetes care and outcomes with community health workers. Fam Pract. 2016;33(5):523–8. https://doi.org/10.1093/fampra/cmw055.
Simonsen SE, Ralls B, Guymon A, Garrett T, Eisenman P, Villalta J, et al. Addressing health disparities from within the community: community-based participatory research and community health worker policy initiatives using a gender-based approach. Womens Health Issues. 2017;27(Suppl 1):S46–53. https://doi.org/10.1016/j.whi.2017.09.006.
Norris SL, Chowdhury FM, Van Le K, Horsley T, Brownstein JN, Zhang X, et al. Effectiveness of community health workers in the care of persons with diabetes. Diabet Med. 2006;23(5):544–56. https://doi.org/10.1111/j.1464-5491.2006.01845.x.
Cherrington A, Ayala GX, Amick H, Scarinci I, Allison J, Corbie-Smith G. Applying the community health worker model to diabetes management: using mixed methods to assess implementation and effectiveness. J Health Care Poor Underserved. 2008;19(4):1044–59. https://doi.org/10.1353/hpu.0.0077.
Shah M, Kaselitz E, Heisler M. The role of community health workers in diabetes: update on current literature. Curr Diab Rep. 2013;13(2):163–71. https://doi.org/10.1007/s11892-012-0359-3.
Malcarney MB, Pittman P, Quigley L, Horton K, Seiler N. The changing roles of community health workers. Health Serv Res. 2017;52(Suppl 1):360–82. https://doi.org/10.1111/1475-6773.12657.
Spencer MS, Rosland AM, Kieffer EC, Sinco BR, Valerio M, Palmisano G, et al. Effectiveness of a community health worker intervention among African American and Latino adults with type 2 diabetes: a randomized controlled trial. Am J Public Health. 2011;101(12):2253–60. https://doi.org/10.2105/AJPH.2010.300106.
Rothschild SK, Martin MA, Swider SM, Tumialan Lynas CM, Janssen I, Avery EF, et al. Mexican American trial of community health workers: a randomized controlled trial of a community health worker intervention for Mexican Americans with type 2 diabetes mellitus. Am J Public Health. 2014;104(8):1540–8. https://doi.org/10.2105/AJPH.2013.301439.
Collinsworth AW, Vulimiri M, Schmidt KL, Snead CA. Effectiveness of a community health worker-led diabetes self-management education program and implications for CHW involvement in care coordination strategies. Diabetes Educ. 2013;39(6):792–9. https://doi.org/10.1177/0145721713504470.
Heisler M, Choi H, Palmisano G, Mase R, Richardson C, Fagerlin A, et al. Comparison of community health worker-led diabetes medication decision-making support for low-income Latino and African American adults with diabetes using e-health tools versus print materials: a randomized, controlled trial. Ann Intern Med. 2014;161(10 Suppl):S13–22. https://doi.org/10.7326/M13-3012.
Perez-Escamilla R, Damio G, Chhabra J, Fernandez ML, Segura-Perez S, Vega-Lopez S, et al. Impact of a community health workers-led structured program on blood glucose control among Latinos with type 2 diabetes: the DIALBEST trial. Diabetes Care. 2015;38(2):197–205. https://doi.org/10.2337/dc14-0327.
Carrasquillo O, Lebron C, Alonzo Y, Li H, Chang A, Kenya S. Effect of a community health worker intervention among Latinos with poorly controlled type 2 diabetes: the Miami healthy heart initiative randomized clinical trial. JAMA Intern Med. 2017;177(7):948–54. https://doi.org/10.1001/jamainternmed.2017.0926.
Brown HS 3rd, Wilson KJ, Pagan JA, Arcari CM, Martinez M, Smith K, et al. Cost-effectiveness analysis of a community health worker intervention for low-income Hispanic adults with diabetes. Prev Chronic Dis. 2012;9:E140. https://doi.org/10.5888/pcd9.120074.
Allen C, Brownstein JN, Jayapaul-Philip B, Matos S, Mirambeau A. Strengthening the effectiveness of state-level community health worker initiatives through ambulatory care partnerships. J Ambul Care Manage. 2015;38(3):254–62. https://doi.org/10.1097/JAC.0000000000000085.
Albritton E. How states can fund community health workers through Medicaid to improve people’s health, decrease costs, and reduce disparities. FamiliesUSA. 2016; http://familiesusa.org/sites/default/files/product_documents/HE_HST_Community_Health_Workers_Brief_v4.pdf. .
Komaromy M, Ceballos V, Zurawski A, Bodenheimer T, Thom DH, Arora S. Extension for Community Healthcare Outcomes (ECHO): a new model for community health worker training and support. J Public Health Policy. 2018;39(2):203–16. https://doi.org/10.1057/s41271-017-0114-8.
Bureau of Labor Statistics. 21-1094 community health workers. In: Occupational employment and wages, May 2018. United States Department of Labor 2018. https://www.bls.gov/oes/current/oes211094.htm. .
Kartika T. Innovative community health worker strategies: Medicaid payment models for community health worker home visits. 2017. https://nashp.org/wp-content/uploads/2017/11/CHW-Home-Improvement1.pdf. .
State Community Health Worker Models. National Academy for State Health Policy. 2019. https://nashp.org/state-community-health-worker-models/. Accessed August 16, 2019.
Nagahisa T, Saisho Y. Cardiorenal protection: potential of SGLT2 inhibitors and GLP-1 receptor agonists in the treatment of type 2 diabetes. Diabetes Ther. 2019;10:1733–52. https://doi.org/10.1007/s13300-019-00680-5.
O’Brien MJ, Karam SL, Wallia A, Kang RH, Cooper AJ, Lancki N, et al. Association of second-line antidiabetic medications with cardiovascular events among insured adults with type 2 diabetes. JAMA Netw Open. 2018;1(8):e186125. https://doi.org/10.1001/jamanetworkopen.2018.6125.
Ackermann RT, Wallia A, O'Brien MJ, Kang R, Cooper A, Moran MR, et al. Correlates of second-line type 2 diabetes medication selection in the USA. BMJ Open Diabetes Res Care. 2017;5(1):e000421. https://doi.org/10.1136/bmjdrc-2017-000421.
Montvida O, Shaw J, Atherton JJ, Stringer F, Paul SK. Long-term trends in antidiabetes drug usage in the U.S.: real-world evidence in patients newly diagnosed with type 2 diabetes. Diabetes Care. 2018;41(1):69–78. https://doi.org/10.2337/dc17-1414.
Sasson C, Eckel R, Alger H, Bozkurt B, Carson A, Daviglus M, et al. American Heart Association Diabetes and Cardiometabolic Health Summit: summary and recommendations. J Am Heart Assoc. 2018;7(15):e009271. https://doi.org/10.1161/JAHA.118.009271.
Sanchez EJ, Cefalu WT. Know diabetes by heart. Circulation. 2019;140(7):526–8. https://doi.org/10.1161/CIRCULATIONAHA.119.039161.
Powering Healthier Communities: Community Health Centers Address the Social Determinants of Health. National Association of Community Health Centers. 2012. http://www.nachc.org/wp-content/uploads/2016/07/SDH_Brief_2012.pdf. Accessed October 29, 2019.
Community Health Centers Leveraging the Social Determinants of Health. Institute for alternative futures. 2012. http://www.altfutures.org/wp-content/uploads/2016/04/2012_Report_Community-Health-Centers-Leveraging-the-Social-Determinants-of-Health.pdf. Accessed November 8, 2019.
Billioux A, Verlander K, Anthony S, Alley D. Standardized screening for health-related social needs in clinical settings: the accountable health communities screening tool. In: Discussion Paper, National Academy of Medicine. National Academy of Medicine, Washington, DC. 2017. http://www.ncalhd.org/wp-content/uploads/2017/09/Standardized-Screening-for-Health-Related-Social-Needs-in-Clinical-Settings.pdf. .
• Berkowitz SA, Karter AJ, Corbie-Smith G, Seligman HK, Ackroyd SA, Barnard LS et al. Food insecurity, food “deserts,” and glycemic control in patients with diabetes: a longitudinal analysis. Diabetes Care. 2018;41(6):1188–95. doi:https://doi.org/10.2337/dc17-1981. This study provides compelling evidence for food insecurity as a factor in diabetes management—a social determinant of health of relatively high frequency among community health center patients.
Berkowitz SA, Meigs JB, DeWalt D, Seligman HK, Barnard LS, Bright OJ, et al. Material need insecurities, control of diabetes mellitus, and use of health care resources: results of the Measuring Economic Insecurity in Diabetes study. JAMA Intern Med. 2015;175(2):257–65. https://doi.org/10.1001/jamainternmed.2014.6888.
Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE). National Association of Community Health Centers,. 2019. http://www.nachc.org/research-and-data/prapare/. Accessed October 28, 2019.
Gold R, Bunce A, Cowburn S, Dambrun K, Dearing M, Middendorf M, et al. Adoption of social determinants of health EHR tools by community health centers. Ann Fam Med. 2018;16(5):399–407. https://doi.org/10.1370/afm.2275.
Hessler D, Bowyer V, Gold R, Shields-Zeeman L, Cottrell E, Gottlieb LM. Bringing social context into diabetes care: intervening on social risks versus providing contextualized care. Curr Diab Rep. 2019;19(6):30. https://doi.org/10.1007/s11892-019-1149-y.
Alvarez C, Lantz P, Sharac J, Shin P. Food insecurity, food assistance and health status in the U.S. community health center population. J Health Care Poor Underserved. 2015;26(1):82–91. https://doi.org/10.1353/hpu.2015.0006.
Burke RE, O’Grady ET. Group visits hold great potential for improving diabetes care and outcomes, but best practices must be developed. Health Aff (Millwood). 2012;31(1):103–9. https://doi.org/10.1377/hlthaff.2011.0913.
Riley SB, Marshall ES. Group visits in diabetes care: a systematic review. Diabetes Educ. 2010;36(6):936–44. https://doi.org/10.1177/0145721710385013.
Housden L, Wong ST, Dawes M. Effectiveness of group medical visits for improving diabetes care: a systematic review and meta-analysis. CMAJ. 2013;185(13):E635–44. https://doi.org/10.1503/cmaj.130053.
Careyva BA, Johnson MB, Shaak K, Stello B, Hansen SE. Patient-reported barriers and limitations to attending diabetes group visits. J Prim Care Community Health. 2015;6(4):279–81. https://doi.org/10.1177/2150131915585107.
Careyva BA, Johnson MB, Goodrich SA, Shaak K, Stello B. Clinician-reported barriers to group visit implementation. J Prim Care Community Health. 2016;7(3):188–93. https://doi.org/10.1177/2150131916631924.
Noya CE, Chesla C, Waters C, Alkon A. Shared medical appointments: an innovative model to reduce health disparities among Latinos with type-2 diabetes. West J Nurs Res. 2019;193945919845677. https://doi.org/10.1177/0193945919845677.
Peek ME. Can mHealth interventions reduce health disparities among vulnerable populations? Nursing and Health Care Diversity. 2016;14(2):44–5.
Kitsiou S, Pare G, Jaana M, Gerber B. Effectiveness of mHealth interventions for patients with diabetes: an overview of systematic reviews. PLoS One. 2017;12(3):e0173160. https://doi.org/10.1371/journal.pone.0173160.
Ruggiero L, Moadsiri A, Quinn LT, Riley BB, Danielson KK, Monahan C et al. Diabetes island: preliminary impact of a virtual world self-care educational intervention for african americans with type 2 diabetes. JMIR Serious Games. 2014;2(2). doi:https://doi.org/10.2196/games.3260.
• Fu H, McMahon SK, Gross CR, Adam TJ, Wyman JF. Usability and clinical efficacy of diabetes mobile applications for adults with type 2 diabetes: a systematic review. Diabetes Res Clin Pract. 2017;131:70–81. doi:https://doi.org/10.1016/j.diabres.2017.06.016. This study synthesizes evidence that mobile health technologies have the potential to improve diabetes care.
Welch G, Balder A, Zagarins S. Telehealth program for type 2 diabetes: usability, satisfaction, and clinical usefulness in an urban community health center. Telemed J E Health. 2015;21(5):395–403. https://doi.org/10.1089/tmj.2014.0069.
Sasso FC, Pafundi PC, Gelso A, Bono V, Costagliola C, Marfella R, et al. Telemedicine for screening diabetic retinopathy: the NO BLIND Italian multicenter study. Diabetes Metab Res Rev. 2019;35(3):e3113. https://doi.org/10.1002/dmrr.3113.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
A. Taylor Kelley declares that he has no conflict of interest.
Robert Nocon reports personal fees from RCHN Community Health Foundation, personal fees and non-financial support from Health Resources and Services Administration, and non-financial support from National Association of Community Health Centers.
Matthew J. O’Brien reports grants and personal fees from United Healthcare Services, and personal fees from NovoNordisk.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Economics and Policy in Diabetes
Rights and permissions
About this article
Cite this article
Kelley, A.T., Nocon, R.S. & O’Brien, M.J. Diabetes Management in Community Health Centers: a Review of Policies and Programs. Curr Diab Rep 20, 8 (2020). https://doi.org/10.1007/s11892-020-1289-0
Published:
DOI: https://doi.org/10.1007/s11892-020-1289-0