Abstract
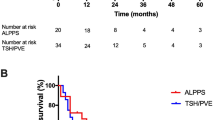
Liver resection is the treatment of choice for patients with colorectal liver metastases (CRLM). The possibility of achieving curative resection is limited by the future liver remnant (FLR), with posthepatectomy liver failure (PHLF) the most severe possible complication after major liver resection. Associated liver partition and portal vein ligation for staged hepatectomy (ALPPS) has recently been introduced as a strategy for prevention of PHLF by inducing a rapid and large FLR hypertrophy not achieved by other methods. To date, most of the evidence regarding ALPPS is based on retrospective analysis of small series of patients or of case reports. The promising short-term results obtained are difficult to interpret oncologically, because of the heterogeneous groups of patients with different underlying pathology, variable chemotherapy use, and technical variations applied. Only increased experience and long-term outcomes will better define the utility of this novel method.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127(12):2893–917.
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62(1):10–29.
Rocha FG, Helton WS. Resectability of colorectal liver metastases: an evolving definition. HPB (Oxford). 2012;14(5):283–4.
Adair RA, Young AL, Cockbain AJ, et al. Repeat hepatic resection for colorectal liver metastases. Br J Surg. 2012;99(9):1278–83.
Tzeng CW, Aloia TA. Colorectal liver metastases. J Gastrointest Surg. 2012 Oct 3. [Epub ahead of print].
Robinson SM, Wilson CH, Burt AD, Manas DM, White SA. Chemotherapy—associated liver injury in patients with colorectal liver metastases: a systematic review and meta-analysis. Ann Surg Oncol. 2012 Jul 6. [Epub ahead of print].
Mohammad WM, Martel G, Mimeault R, et al. Evaluating agreement regarding the resectability of colorectal liver metastases: a national case-based survey of hepatic surgeons. HPB (Oxford). 2012;14(5):291–7.
Lehmann K, Rickenbacher A, Weber A, Pestalozzi BC, Clavien PA. Chemotherapy before liver resection of colorectal metastases: friend or foe? Ann Surg. 2012;255(2):237–47.
Viganò L, Ferrero A, Lo Tesoriere R, Capussotti L. Liver surgery for colorectal metastases: results after 10 years of follow-up. Long-term survivors, late recurrences, and prognostic role of morbidity. Ann Surg Oncol. 2008;15(9):2458–64.
Rahbari NN, Garden OJ, Padbury R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 2011;149:713–24.
Liu H, Zhu S. Present status and future perspectives of preoperative portal vein embolization. Am J Surg. 2009;197:686–90.
Rubbia-Brandt L, Audard V, Sartoretti P, et al. Severe hepatic sinusoidal obstruction associated with oxaliplatin-based chemotherapy in patients with metastatic colorectal cancer. Ann Oncol. 2004;15:460–6.
Clavien PA, Petrowsky H, De Oliveira ML, Graf R. Strategies for safer liver surgery and partial liver transplantation. N Engl J Med. 2007;356:1545–1559-8.
Wicherts DA, Miller R, de Haas RJ, et al. Long-term results of two-stage hepatectomy for irresectable colorectal cancer liver metastases. Ann Surg. 2008;248(6):994–1005.
Abulkhir A, Limongelli P, Healey AJ, et al. Preoperative portal vein embolization for major liver resection: a meta-analysis. Ann Surg. 2008;247(1):49–57.
Mueller L, Hillert C, Möller L, et al. Major hepatectomy for colorectal metastases: is preoperative portal occlusion an oncological risk factor? Ann Surg Oncol. 2008;15(7):1908–17.
Simoneau E, Aljiffry M, Salman A, et al. Portal vein embolization stimulates tumor growth in patients with colorectal cancer liver metastases. HPB (Oxford). 2012;14(7):461–8.
• Hoekstra LT, van Lienden KP, Doets A, et al. Tumor progression after preoperative portal vein embolization. Ann Surg. 2012;256(5):812–8. This is the first study to compare patients with and without portal vein embolization for whom tumor growth before and after embolization was reported.
•• Schnitzbauer AA, Lang SA, Goessmann H, et al. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling two-staged extended right hepatic resection in small-for-size settings. Ann Surg. 2012;255:405–14. The authors publish the largest series to date, covering the ALPPS approach in a multicenter study including 25 patients.
de Santibañes E, Clavien PA. Playing Play-Doh to prevent postoperative liver failure: the “ALPPS” approach. Ann Surg. 2012;255(3):415–7.
Baumgart J, Lang S, Lang H. A new method for induction of liver hypertrophy prior to right trisectionectomy: a report of three cases. HPB (Oxford). 2011;13 suppl 2:1–145.
• de Santibañes E, Alvarez FA, Ardiles V. How to avoid postoperative liver failure: a novel method. World J Surg. 2012;36:125–8. For the first time the function of both hemilivers during the interval period of ALPPS is evaluated by scintigraphy and the concept of an auxiliary liver is introduced.
Alvarez FA, Iniesta J, Lastiri J, et al. New method of hepatic regeneration. Cir Esp. 2011;89:645–9.
Sala S, Ardiles V, Ulla M, et al. Our initial experience with ALPPS technique: encouraging results. Updates Surg. 2012;64(3):167–72.
Donati M, Stavrou GA, Basile F, et al. Combination of in situ split and portal ligation: lights and shadows of a new surgical procedure. Ann Surg. 2012;256(3):e11–2. author reply e16–9.
Hemming AW, Reed AI, Howard RJ, et al. Preoperative portal vein embolization for extended hepatectomy. Ann Surg. 2003;237(5):686–91.
Clavien PA, Lillemoe KD. Note from the editors on the ALPPS e-Letters-to-the-Editor. Ann Surg. 2012;256(3):552.
• Alvarez FA, Ardiles V, Sanchez Claria R, Pekolj J, de Santibañes E. Associating Liver Partition and Portal vein ligation for Staged hepatectomy (ALPPS): tips and tricks. J Gastrointest Surg. 2012 Nov 27. [Epub ahead of print]. This technical report is based on the largest ALPPS experience in a single center without mortality.
Ulla M, Ardiles V, Levy-Yeyati E, et al. New surgical strategy to induce liver hypertrophy: role of MDCT-volumetry to monitor and predict liver growth. Hepatogastroenterology. 2012;20:60(122).
Li J, Girotti P, Königsrainer I, Ladurner R, Königsrainer A, Nadalin S. ALPPS in right trisectionectomy: a safe procedure to avoid postoperative liver failure?. J Gastrointest Surg. 2013 Jan 4. [Epub ahead of print].
Dokmak S, Belghiti J. Which limits to the “ALPPS” approach? Ann Surg. 2012;256(3):e6. author reply e16–7.
Agrawal S, Belghiti J. Oncologic resection for malignant tumors of the liver. Ann Surg. 2011;253:656–65.
Moszkowicz D, Cauchy F, Dokmak S, Belghiti J. Routine pedicular lymphadenectomy for colorectal liver metastases. J Am Coll Surg. 2012;214(6):e39–45.
Jaeck D, Nakano H, Bachellier P, et al. Significance of hepatic pedicle lymph node involvement in patients with colorectal liver metastases: a prospective study. Ann Surg Oncol. 2002;9(5):430–8.
Aloia TA, Vauthey JN. Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): what is gained and what is lost? Ann Surg. 2012;256(3):e9. author reply e16–9.
Jain HA, Bharathy KG, Negi SS. Associating liver partition and portal vein ligation for staged hepatectomy: will the morbidity of an additional surgery be outweighed by better patient outcomes in the long-term? Ann Surg. 2012;256(3):e10. author reply e16–7.
Narita M, Oussoultzoglou E, Ikai I, et al. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg. 2012;256(3):e7–8. author reply e16–7.
Govil S. Rapid improvement in liver volume induced by portal vein ligation and staged hepatectomy: the ALPPS procedure. HPB (Oxford). 2012;14(12):874.
Strobel O, Büchler MW. Portal vein ligation combined with in situ splitting. Rapid hypertrophy of the liver remnant enables 2-stage extended hepatic resections. Chirurg. 2012;83(5):483.
Loos M, Friess H. Is there new hope for patients with marginally resectable liver malignancies. World J Gastrointest Surg. 2012;4(7):163–5.
Schnitzbauer AA, Lang SA. ALPPS: response to letter to the editor. Ann Surg. 2012;256(3):e16–7.
Clavien PA. de Santibañes. The ALPPS: time to explore! Ann Surg. 2012;256(3):e18–9.
• Andriani OC. Long-term results with associating liver partition and portal vein ligation for staged hepatectomy (ALPPS). Ann Surg. 2012;256(3):e5. author reply e16–9. The longest survivals with ALPPS are reported in this interesting letter to the editor.
Machado MA, Makdissi FF, Surjan RC. Totally laparoscopic ALPPS is feasible and may be worthwhile. Ann Surg. 2012;256(3):e13. author reply e16–9.
Conrad C, Shivathirthan N, Camerlo A, Strauss C, Gayet B. Laparoscopic portal vein ligation with in situ liver split for failed portal vein embolization. Ann Surg. 2012;256(3):e14–5. author reply e16–7.
Riehle KJ, Dan YY, Campbell JS, Fausto N. New concepts in liver regeneration. J Gastroenterol Hepatol. 2011;26 Suppl 1:203–12.
Ding BS, Nolan DJ, Butler JM, et al. Inductive angiocrine signals from sinusoidal endothelium are required for liver regeneration. Nature. 2010;468:310–5.
Abshagen K, Eipel C, Vollmar B. A critical appraisal of the hemodynamic signal driving liver regeneration. Langenbecks Arch Surg. 2012;397(4):579–90.
Michalopoulos GK. Liver regeneration after partial hepatectomy: critical analysis of mechanistic dilemmas. Am J Pathol. 2010;176(1):2–13.
Nadalin S, Testa G, Malagó M, et al. Volumetric and functional recovery of the liver after right hepatectomy for living donation. Liver Transpl. 2004;10(8):1024–9.
Zappa M, Dondero F, Sibert A, et al. Liver regeneration at day 7 after right hepatectomy: global and segmental volumetric analysis by using CT. Radiology. 2009;252(2):426–32.
Madoff DC, Abdalla EK, Gupta S, et al. Transhepatic ipsilateral right portal vein embolization extended to segment IV: improving hypertrophy and resection outcomes with spherical particles and coils. J Vasc Interv Radiol. 2005;16:215–25.
Goéré D, Farges O, Leporrier J, et al. Chemotherapy does not impair hypertrophy of the left liver after right portal vein obstruction. J Gastrointest Surg. 2006;10(3):365–70.
Sturesson C, Keussen I, Tranberg KG. Prolonged chemotherapy impairs liver regeneration after portal vein occlusion—an audit of 26 patients. Eur J Surg Oncol. 2010;36(4):358–64.
Narita M, Oussoultzoglou E, Chenard MP, et al. Sinusoidal obstruction syndrome compromises liver regeneration in patients undergoing two-stage hepatectomy with portal vein embolization. Surg Today. 2011;41(1):7–17.
Millet G, Truant S, Leteurtre E, et al. Volumetric analysis of remnant liver regeneration after major hepatectomy in bevacizumab-treated patients: a case-matched study in 82 patients. Ann Surg. 2012;256(5):755–61.
Cavaness KM, Doyle MB, Lin Y, et al. Using ALPPS to induce rapid liver hypertrophy in a patient with hepatic fibrosis and portal vein thrombosis. J Gastrointest Surg. 2013;17(1):207–12.
Kishi Y, Zorzi D, Contreras CM, et al. Extended preoperative chemotherapy does not improve pathologic response and increases postoperative liver insufficiency after hepatic resection for colorectal liver metastases. Ann Surg Oncol. 2010;17(11):2870–6.
Scatton O, Belghiti J, Dondero F, et al. Harvesting the middle hepatic vein with a right hepatectomy does not increase the risk for the donor. Liver Transpl. 2004;10(1):71–6.
• de Graaf W, van Lienden KP, van den Esschert JW, Bennink RJ, van Gulik TM. Increase in future remnant liver function after preoperative portal vein embolization. Br J Surg. 2011;98(6):825–34. The authors demonstrated that after portal vein embolization, future liver remnant function is recovered before volume.
Uesaka K, Nimura Y, Nagino M. Changes in hepatic lobar function after right portal vein embolization. An appraisal by biliary indocyanine green excretion. Ann Surg. 1996;223(1):77–83.
Stockmann M, Lock JF, Malinowski M, et al. The LiMAx test: a new liver function test for predicting postoperative outcome in liver surgery. HPB (Oxford). 2010;12(2):139–46.
de Graaf W, van Lienden KP, van Gulik TM, Bennink RJ. (99m)Tc-mebrofenin hepatobiliary scintigraphy with SPECT for the assessment of hepatic function and liver functional volume before partial hepatectomy. J Nucl Med. 2010;51(2):229–36.
de Graaf W, van Lienden KP, Dinant S, et al. Assessment of future remnant liver function using hepatobiliary scintigraphy in patients undergoing major liver resection. J Gastrointest Surg. 2010;14(2):369–78.
Oldhafer KJ, Donati M, Maghsoudi T, Ojdanić D, Stavrou GA. Integration of 3D volumetry, portal vein transection and in situ split procedure: a new surgical strategy for inoperable liver metastasis. J Gastrointest Surg. 2012;16(2):415–6.
Cauchy F, Aussilhou B, Dokmak S, et al. Reappraisal of the risks and benefits of major liver resection in patients with initially unresectable colorectal liver metastases. Ann Surg. 2012;256(5):746–54.
Wicherts DA, de Haas RJ, Andreani P, et al. Impact of portal vein embolization on long-term survival of patients with primarily unresectable colorectal liver metastases. Br J Surg. 2010;97(2):240–50.
de Santibañes E, Fernandez D, Vaccaro C, et al. Short-term and long-term outcomes after simultaneous resection of colorectal malignancies and synchronous liver metastases. World J Surg. 2010;34(9):2133–40.
Disclosure
Fernando A. Alvarez declares that he has no conflict of interest. Victoria Ardiles declares that she has no conflict of interest. Eduardo de Santibañes declares that he has no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alvarez, F.A., Ardiles, V. & de Santibañes, E. The ALPPS Approach for the Management of Colorectal Carcinoma Liver Metastases. Curr Colorectal Cancer Rep 9, 168–177 (2013). https://doi.org/10.1007/s11888-013-0159-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11888-013-0159-4
Keywords
- Colorectal cancer
- Liver metastases
- Chemotherapy
- ALPPS
- Major liver resection
- Malignant disease
- Posthepatectomy liver failure
- Surgical technique
- Portal vein ligation
- Portal vein embolization
- Staged hepatectomy
- Metastatic colorectal cancer
- Survival
- Complications
- Liver hypertrophy
- Scintigraphy
- Auxiliary liver
- Liver regeneration
- Biliary leak
- Future liver remnant
- Monoclonal antibodies
- Volumetric studies
- Cirrhosis
- Laparoscopy
- Histology
- Liver function