Abstract
Rhinosinusitis (RS) is a symptomatic disease classification of many causes and is a major economic burden worldwide. It is widely accepted that RS is further classified into acute (ARS) and chronic (CRS) rhinosinusitis based on the duration of the symptoms, and that viral infection plays a large role in initiating or potentiating the disease. In this review, we examine the role of respiratory virus infection in the exacerbation of ARS and CRS. We explore the epidemiology of viral exacerbation of ARS and CRS and highlight key viruses that may cause exacerbation. We also review the current understanding of viral infections in the upper airway to further explain the putative underlying mechanisms of inflammatory events in ARS and CRS exacerbation. Advances in accurate diagnosis of the etiologic respiratory viruses of ARS and CRS symptoms which can lead to better disease management are also surveyed. In addition to the current treatments which provide symptomatic relief, we also explore the potential of harnessing existing antiviral strategies to prevent ARS and CRS exacerbation, especially with improved viral diagnostic tools to guide accurate prescription of antivirals against causative respiratory viruses.
Similar content being viewed by others
Introduction
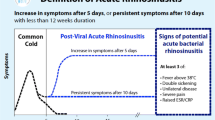
Rhinosinusitis (RS) is a condition that arises from inflammation of the nose and the paranasal sinuses resulting in two or more symptoms including nasal blockage, obstruction, congestion, and nasal discharge [1••, 2••]. Additional symptoms may include facial pain and pressure, reduction or loss of smell. During diagnosis, endoscopic signs of polyps, mucopurulent discharge, and mucosal obstruction in the middle meatus and computerized tomography (CT) changes within the ostiomeatal complex may be observed [2••]. RS can be classified into two major types based on the duration and nature of the disease. Acute rhinosinusitis (ARS) involves the presentation of two or more symptoms for the duration of less than 12 weeks, with the damage to the nasal passage being often reversible. On the other hand, chronic rhinosinusitis (CRS) involves remodeling of the nasal passage due to long-standing inflammation causing persistent symptoms for more than 12 weeks [2••, 3]. Regardless of duration, both ARS and CRS can be caused by infection by pathogens or allergies against environmental allergens. However, in most cases, the key trigger of RS is often a viral infection that either initiates or exacerbates the symptoms [1••, 2••, 4••].
Epidemiology of ARS and CRS
RS is a very common condition encountered in primary care, accounting for about 15% of the population in Western countries [4••]. The prevalence of ARS is relatively high with an estimated prevalence rate of 6–15% worldwide according to various epidemiological studies [2••, 5]. On the other hand, studies on the epidemiology and prevalence of CRS are less comprehensive compared to ARS. This is due to the fact that CRS encompasses many forms of presentation which confound the study parameters when accounting for their prevalence. A prevalence of 5–15% prevalence is estimated both in the USA and Europe based on compilation of available studies [2••, 6,7,8,9].
Pathophysiology and Mechanism of Action of Viral Infection in ARS and CRS
The nature of the disease of RS is highly dependent on the predisposing conditions such as allergic rhinitis, nasal deformity, immune deficiency, and other environmental factors. These underlying conditions can be exacerbated following primary damage caused by viral infections and the secondary damage caused by the host response against the virus, resulting in the pathology of RS and its symptoms. In ARS, the primary and secondary damage does not result in permanent changes to the nasal passage, and the ARS symptoms arising from the acute infection typically subside within 12 weeks. On the other hand, when the host responses triggered by the viral infection cause permanent alteration of the anatomy of the nasal passage such as remodeling of the epithelial layer, long-term effects may present in the form of CRS [2••, 3, 10].
As the main cause of ARS is viral, the host immune response that leads to the pathophysiology of RS is mainly antiviral in nature. The antiviral immune response involves nonspecific and specific components that require the coordination between different cell types including neutrophils, macrophages, eosinophils, dendritic cells, epithelial cells, mast cells, natural killer cells, and lymphocytes [11••, 12•]. An ideal scenario is when the elicited immune response is timely and culminates in early viral elimination and minimal damage to the host. However, the cascade of inflammation initiated by the epithelial cells normally lead to damage by the infiltrating cells, causing edema, engorgement, fluid extravasation, mucus production, and sinus obstruction in the process, eventually leading to ARS or exacerbating ARS [1••, 2••].
The exact roles and mechanisms of respiratory viruses in ARS exacerbation are still under debate. It is often speculated that the T-helper 1 (Th1) response is initiated from the epithelial innate immune response via toll-like receptors 3, 7, and 9 (TLR 3, TLR7, and TLR9) due to the virus infection [13, 14••]. Depending on the type of viral pathogen, the pathogen-sensing molecules in turn activate the production and secretion of nuclear factor-κB (NF-κB), interferon-β (IFN-β), tumor necrosis factor-α (TNF-α), and interleukins-1β, 6, and 8 (IL-1 β, IL-6, and IL-8), which are potent inducers or recruiters of neutrophils and macrophages [4••, 12•]. The initial action of neutrophils against virus-infected cells usually contributes to the early symptoms of an acute respiratory virus infection. Following this, the further secretion of TNF-α and interferon-γ (IFN-γ) increases the recruitment of Th1 cells and cytotoxic T-cells which leads to the clearance of the viral pathogens and viral-infected cells. The process of clearing the virus generates dead epithelial and infiltrating cells which contribute to the pathology of ARS. It also creates an environment suitable for secondary bacterial infections (such as Staphylococcus aureus and Streptococcus pneumoniae), which represent another factor that exacerbates ARS symptoms initiated by a viral infection [11••, 12•, 15].
On the other hand, CRS pathology is not as straightforward as ARS as the former is associated with multiple factors and disease presentations. However, virus infection is known to contribute to and exacerbate CRS. People suffering from CRS often have predisposing factors that contribute to the inflammatory condition in the nasal passage. One factor is the remodeling of the nasal epithelium due to the extended period of inflammation. During viral infection, the similar inflammatory process causes exacerbation as with ARS. In addition, the destruction of the epithelial layer and macrophage recruitment also induce the production of matrix metalloproteinase-9 (MMP-9), a key remodeling protein that mediates repair of the epithelial and extracellular matrix [16]. The remodeling of the nasal passage in turn exacerbates the symptoms of CRS even further, as normal epithelial function is further diminished due to possible hyperplasia and replacement of epithelial cells with fibroblasts following respiratory viral infection.
Key Viruses Causing the Pathophysiology of ARS and CRS Exacerbation
Viruses account for at least 80 to 90% of the ARS occurrence, with rhinovirus (RV), respiratory syncytial virus (RSV), influenza virus, coronavirus (CorV), parainfluenza virus (PIV), adenovirus (AdeV), and enterovirus (EV) playing a major role in ARS exacerbation [2••, 4••, 9]. These viruses induce strong Th1 responses which lead to the pathology of ARS exacerbation. In addition, RV and PIV may contribute further to the exacerbation as their infection upregulates ICAM-1, viral receptor for major type of RV [17,18,19] (Tan et al., unpublished observation). ICAM-1 is also a signaling protein that activates the migration and infiltration of immune cells to contribute further to the exacerbation and pathophysiology of ARS [20]. RV and CorV are the most common viruses isolated from adult ARS, accounting for approximately 50% of ARS diagnosis. Geographically, there are also other viruses isolated from patients with ARS, e.g., human bocavirus is frequently isolated from ARS cases in Taiwan [21].
On the other hand, most of the viruses that exacerbate ARS will also cause similar exacerbation in CRS patients. There is a high rate of viral detection from the nasal wash of CRS patients including viruses commonly found in ARS patients, with RV also being the most prevalent virus in CRS exacerbation [22]. Human bocavirus and metapneumovirus (hMPV) are also found in the nasal washes of CRS patients during flare ups. Moreover, there are also certain viruses (herpes virus, Epstein-Barr virus, and human cytomegalovirus) found in CRS patients with nasal polyps, and it is currently unclear whether they contribute to exacerbation of CRS [23]. Due to the multifactorial nature of CRS exacerbation, it is relatively harder to identify key viruses that exacerbate CRS compared to ARS, and thus, a direct association between CRS and viral exacerbation is still unclear. The putative underlying mechanism of viral ARS and CRS exacerbation is summarized in Fig. 1 based on existing literature [1••, 2••, 11••, 12•, 14••].
Putative underlying mechanisms of viral-induced ARS and CRS exacerbation. The figure shows the chain of events leading to ARS and CRS exacerbation from common respiratory virus infections (rhinovirus and influenza virus). When a respiratory virus infects its respective host cells in the nasal epithelium, the intracellular pathogen sensors TLRs 3, 7, and 9 are activated to initiate an antiviral cellular response via the activation of STAT1/2 and NF-κB transcription factors. These activated transcription factors then induce the expression of interferons (IFNs), interferon-stimulated genes (ISGs), chemokines, and cytokines against the virus. The cascade of intracellular events leads to the recruitment of innate responders such as neutrophils, macrophages, and dendritic cells, and in turn activates Th1 adaptive responses against the invading respiratory pathogen. This cascade of inflammatory events against the virus culminates in the symptoms of ARS and its exacerbation, especially if persistent infection occurs due to insufficient viral clearance. Furthermore, the priming of the nasal epithelium against viral infection potentiates its environment to be suitable for secondary bacterial infection which may further exacerbate the symptoms. The infection, if kept unchecked, may result in continued inflammation and expression of remodeling genes that may transition into chronic symptoms of CRS, which increases the susceptibility against further viral infection, causing further exacerbation of symptoms. The putative underlying mechanisms are summarized based on existing literature [1••, 4••, 11••, 12•, 14••]. ARS acute rhinosinusitis, CD cluster of differentiation, CRS chronic rhinosinusitis, DCs dendritic cells, IFN interferon, IL interleukin, ISGs interferon stimulated genes, STAT signaling transducers and activators of transcription, TLR toll-like receptor, MMP matrix metalloproteinase, NF-κB nuclear factor kappa-light-chain-enhancer of activated B cells, TGF transforming growth factor, Th1 T-helper 1
Diagnosis of Viral Infections that Lead to ARS and CRS Exacerbation
As the cause of RS (especially ARS) is almost exclusively viral in nature, the diagnosis of specific viral infection is important to prevent the unnecessary prescription of antibiotics [1••]. In clinical practice, most viral infections are usually diagnosed by symptomatic assessment, which lack objective diagnostic tools for confirmation as well as identification of the type of viral infection [1••, 2••, 9, 15]. However, with the development of rapid viral assays and diagnostic kits, viral detection and identification can now be performed within a point-of-care setting for sensitive and specific identification of respiratory virus infections in patients presenting with ARS or CRS exacerbation [24••]. The current viral detection systems, their features, and use in clinical settings are summarized in Table 1.
Current assays for rapid detection of respiratory viruses include virus detection, antigen detection, and molecular detection. Rapid virus detection culture such as shell vial or cluster trays facilitate detection of adenovirus, influenza A and B virus, PIV 1–4, hMPV, and RSV within 48 h [25]. Assays for virus antigen detection involve the use of viral antigen-specific antibodies using direct fluorescence antibody test and rapid antigen test. The direct fluorescence antibody test can detect AdeV, influenza A and B virus, hMPV, PIV, and RSV within 30 to 60 min [26], while the rapid direct antigen test utilizes immuno-chromatographic antibody detection kits that are simple to perform (detection in 15–20 min), but so far limited only for detecting influenza A and B virus and RSV [27, 28]. Lastly, molecular detection includes amplification of viral nucleic acid sequences through polymerase chain reaction of patient samples. This assay can detect respiratory viruses with high sensitivity and specificity within a short time frame of 20 to 80 min [29] and are recognized to play important roles in respiratory viral diagnosis due to their versatility [24••, 30, 31]. In addition to the above methods, there is also serological detection such as ELISA which detects antibodies against the virus. However, while serological detection was widely used in the current diagnostic settings, it is not suitable for the diagnostics of acute infections that caused ARS and CRS exacerbations, and therefore not discussed in this review.
Currently, rapid culture, direct fluorescence antibody, and molecular detection necessitate specialized laboratories attached to larger hospitals to perform the diagnosis and identification of viruses causing ARS and CRS exacerbation, due to the complexity and training to operate such assays. The point-of-care detection method is the rapid direct antigen test through immuno-chromatography, but this test suffers from sensitivity issues and may lead to false negatives and misdiagnosis [32, 33]. Therefore, it is imperative to continue to improve diagnostic kits to rapidly and accurately pinpoint the causative agents of ARS or CRS exacerbation to prevent inappropriate prescriptions for treatment of exacerbation episodes, especially the misuse of antibiotics for viral-induced exacerbation of ARS and CRS.
Prevention and Treatment of Viral Exacerbation of ARS and CRS
The clinical management of ARS and CRS exacerbation due to virus infection should be similar for any episodes of ARS and CRS exacerbation. Treatment usually aims to resolve and relieve the symptoms while the infection resolves itself. Symptomatic treatment involves the use of nasal decongestants and topical corticosteroids to relieve nasal congestion and to reduce nasal edema [34]. Nonsteroidal anti-inflammatory drugs (NSAIDs) may also be used to decrease inflammation arising from viral infection to relieve symptoms such as fever and nasal edema [2••]. When secondary bacterial infection is suspected, narrow-spectrum antibiotics such as amoxicillin can be prescribed. In addition to symptomatic management and relief, treatment and prevention of ARS and CRS exacerbation can be further enhanced with advances in viral detection to identify the exact viral etiology. By using antiviral treatments, viral load in the nasal epithelium can be reduced and therefore further lowering the inflammation associated with the infection, reducing RS symptoms and its duration. Hence, it is possible to add currently available antivirals to the repertoire of preventive and therapeutic strategies to counter viral exacerbation episodes of ARS and CRS.
From the perspective of exploiting antiviral agents to prevent or treat ARS and CRS exacerbation, influenza virus infection has the widest array of therapies. While the adamantane derivatives amantadine and rimantadine that blocks influenza fusion is currently not recommended as a treatment due to widespread resistance [35, 36], there are still multiple neuraminidase inhibitors specific against influenza viruses that are available as therapeutic agents for severe episodes of ARS and CRS exacerbation. For example, oseltamivir, laninamivir, peramivir, and zanamivir specifically inhibit the replication of influenza viruses, and thus prevent or minimize the effects of ARS and CRS exacerbation [37•, 38••]. Such treatments may be harnessed as useful prophylaxis during influenza season for patients with severe episodes of ARS or CRS exacerbation. In addition to neuraminidase inhibitors, annual influenza vaccination can also serve as a means of preventing ARS and CRS exacerbation due to influenza virus infection.
On the other hand, other common respiratory infections due to RV, PIV, RSV, CorV, and AdeV do not have suitable vaccines and have limited antiviral agents that can be used against them. Palivizumab is a monoclonal antibody targeting the fusion of RSV and is used as a prophylaxis for infants at high risk of morbidity or mortality from RSV complications [39]. There are also broad-spectrum antivirals such as ribavirin that prevent viral RNA synthesis that can be used against influenza virus, RSV, PIV, and to a certain extent, coronavirus, but are only reserved for severe cases due to their undesirable adverse effects [40, 41]. Similarly, cidofovir, a DNA synthesis inhibitor is used against disseminated adenovirus infection as a last line of defense against severe adenovirus disease due to concerns on its toxicity. To date, noninfluenza antivirals against respiratory viruses are still in the early stages of development and may not yet be optimal for the prevention and management of viral ARS and CRS exacerbation [37•].
Notwithstanding this, there are also investigational agents in clinical trial phases and are close to being available clinically. These treatments may be useful in the near future to treat respiratory viral infections to manage viral ARS and CRS exacerbation. Favipiravir (T-705) has so far been tested to be efficacious against influenza virus and is being evaluated for other RNA viruses and was recently approved in 2014 to be marketed in Japan for severe influenza [42, 43]. Fludase (DAS181), a fusion protein that prevents influenza infection, is currently in phase II clinical trials [44, 45]. Presatovir (GS-5806), ALS-8176, and ALN-RSV01 are all inhibitors of RSV replication that are undergoing trials as potential treatment against RSV [46,47,48,49]. If found to be efficacious with minimal side effects, these investigational agents can be exploited in the future as effective measures in managing viral exacerbation of ARS and CRS [38••]. Detailed information on the current antiviral drugs against respiratory viruses and their mechanisms of action is discussed in Fig. 2 and Table 2.
Current antiviral drugs against respiratory viruses and their mechanisms of action. The figure shows a representative respiratory virus infection (influenza) in the host cell. Other than vaccines, which do not act directly on viral replication in the host cell, other antivirals target specific virus components required for the replication cycle: (1) viral entry receptor—fludase; (2) viral fusion—presatovir, palivizumab; (3) preventing transcription/replication—ribavirin, taribavirin, cidofovir, favipiravir, ALS-8176; (4) preventing translation—ALN-RSV01; (5) preventing viral excision—oseltamivir, laninamivir, peramivir, zanamivir. The antivirals and their mechanisms are summarized based on existing literature [37•, 38••, 39,40,41]. mRNA messenger RNA, vRNP viral ribonucleoprotein, siRNA small interfering RNA, ALS-8176 deoxy-3′,5′-di-O-isobutyryl-2′-fluorocytidine, ALN-RSV01 asvasiran sodium
Conclusion
ARS and CRS remain a considerable economic and public health burden worldwide due to their high prevalence. As virus infections are now established as the key cause of most cases of RS and exacerbation (especially ARS), more attention should be focused on the proper study, diagnosis, prevention, management, and treatment of viral-induced exacerbation of ARS and CRS symptoms. A more detailed perspective of the virology of ARS and CRS exacerbation can enhance our current understanding of RS to improve the quality of treatment of episodes of ARS and CRS exacerbation, as well as to minimize and prevent the misuse of antibiotics in the treatment of ARS and CRS exacerbation, which may contribute to the growing spectrum of antibiotic resistance.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Hoggard M, Wagner Mackenzie B, Jain R, et al. Chronic rhinosinusitis and the evolving understanding of microbial ecology in chronic inflammatory mucosal disease. Clin Microbiol Rev. 2017;30:321–48. This review summarizes the current stage of understanding in the role of viruses in CRS and the current gaps in identifying the viral diversity in CRS microbiome
•• Fokkens WJ, Lund VJ, Mullol J, et al. European position paper on rhinosinusitis and nasal polyps 2012. Rhinology Suppl. 2012;23:1–298. This article is the keynote article on rhinosinusitis and includes the latest understanding, mechanisms, findings, diagnosis and management of ARS and CRS
Li C, Shi L, Yan Y, et al. Gene expression signatures: a new approach to understanding the pathophysiology of chronic rhinosinusitis. Curr Allergy Asthma Rep. 2013;13:209–17.
•• Eloy P, Poirrier AL, De Dorlodot C, et al. Actual concepts in rhinosinusitis: a review of clinical presentations, inflammatory pathways, cytokine profiles, remodeling, and management. Curr Allergy Asthma Rep. 2011;11:146–62. This review summarizes the current understanding of ARS and CRS mechanism of exarcerbation, immune cells’ roles and profiles and the role of different microbes in the exacerbation
Wang DY, Wardani RS, Singh K, et al. A survey on the management of acute rhinosinusitis among Asian physicians. Rhinology. 2011;49:264–71.
Hamilos DL. Chronic rhinosinusitis: epidemiology and medical management. J Allergy Clin Immunol. 2011;128:693–707.
Shi JB, Fu QL, Zhang H, et al. Epidemiology of chronic rhinosinusitis: results from a cross-sectional survey in seven Chinese cities. Allergy. 2015;70:533–9.
Hastan D, Fokkens WJ, Bachert C, et al. Chronic rhinosinusitis in Europe--an underestimated disease. A GA(2)LEN study. Allergy. 2011;66:1216–23.
Orlandi RR, Kingdom TT, Hwang PH, et al. International consensus statement on allergy and rhinology: rhinosinusitis. Int Forum Allergy Rhinol. 2016;6(Suppl 1):S22–209.
Yan Y, Gordon WM, Wang DY. Nasal epithelial repair and remodeling in physical injury, infection, and inflammatory diseases. Curr Opin Otolaryngol Head Neck Surg. 2013;21:263–70.
•• Vareille M, Kieninger E, Edwards MR, Regamey N. The airway epithelium: soldier in the fight against respiratory viruses. Clin Microbiol Rev. 2011;24:210–29. This review comprehensively covers the role of airway epithelial in responses against invading pathogen, and is used to reinforce the understanding of nasal antiviral immune responses in leading to ARS and CRS exacerbation
• Braciale TJ, Sun J, Kim TS. Regulating the adaptive immune response to respiratory virus infection. Nat Rev Immunol. 2012;12:295–305. This review covers the comprehensive overview of innate and adaptive antiviral immune responses against respiratory viruese in the lungs; which were used as a basis to reinforce the understanding of nasal antiviral immune responses
Deng Y, Yan Y, Tan KS, et al. MicroRNA-146a induction during influenza H3N2 virus infection targets and regulates TRAF6 levels in human nasal epithelial cells (hNECs). Exp Cell Res. 2017;352:184–92.
•• Yan Y, Tan KS, Li C, et al. Human nasal epithelial cells derived from multiple subjects exhibit differential responses to H3N2 influenza virus infection in vitro. J Allergy Clin Immunol. 2016;138:276–81. This article provides the pathogenesis of influenza A virus and the mechanism of innate antiviral responses in the nasal epithelium to reinforce the understanding of respiratory viruses’ role in leading to ARS and CRS exacerbation
Mahdavinia M, Keshavarzian A, Tobin MC, et al. A comprehensive review of the nasal microbiome in chronic rhinosinusitis (CRS). Clin Exp Allergy. 2016;46:21–41.
Tacon CE, Wiehler S, Holden NS, et al. Human rhinovirus infection up-regulates MMP-9 production in airway epithelial cells via NF-kappaB. Am J Respir Cell Mol Biol. 2010;43:201–9.
Othumpangat S, Regier M, Piedimonte G. Nerve growth factor modulates human rhinovirus infection in airway epithelial cells by controlling ICAM-1 expression. Am J Physiol Lung Cell Mol Physiol. 2012;302:L1057–66.
van Kempen M, Bachert C, Van Cauwenberge P. An update on the pathophysiology of rhinovirus upper respiratory tract infections. Rhinology. 1999;37:97–103.
Pawelczyk M, Kowalski ML. The role of human parainfluenza virus infections in the immunopathology of the respiratory tract. Curr Allergy Asthma Rep. 2017;17:16.
Bianco A, Whiteman SC, Sethi SK, et al. Expression of intercellular adhesion molecule-1 (ICAM-1) in nasal epithelial cells of atopic subjects: a mechanism for increased rhinovirus infection? Clin Exp Immunol. 2000;121:339–45.
Chuang CY, Kao CL, Huang LM, et al. Human bocavirus as an important cause of respiratory tract infection in Taiwanese children. J Microbiol Immunol Infect. 2011;44:323–7.
Cho GS, Moon BJ, Lee BJ, et al. High rates of detection of respiratory viruses in the nasal washes and mucosae of patients with chronic rhinosinusitis. J Clin Microbiol. 2013;51:979–84.
Costa C, Garzaro M, Boggio V, et al. Detection of herpesviruses 1-6 and community-acquired respiratory viruses in patients with chronic rhinosinusitis with nasal polyposis. Intervirology. 2014;57:101–5.
•• Ginocchio CC, Mc Adam AJ. Current best practices for respiratory virus testing. J Clin Microbiol. 2011;49(Suppl 9):44–8. This review conveyed the different viral diagnostic tools available that can be applied in the diagnosis of respiratory virus type in ARS and CRS exacerbations
McAdam AJ, Riley AM. Developments in tissue culture detection of respiratory viruses. Clin Lab Med. 2009;29:623–34.
Landry ML. Developments in immunologic assays for respiratory viruses. Clin Lab Med. 2009;29:635–47.
Dunn JJ, Ginocchio CC. Can newly developed, rapid immunochromatographic antigen detection tests be reliably used for the laboratory diagnosis of influenza virus infections? J Clin Microbiol. 2015;53:1790–6.
Selvarangan R, Abel D, Hamilton M. Comparison of BD Directigen EZ RSV and Binax NOW RSV tests for rapid detection of respiratory syncytial virus from nasopharyngeal aspirates in a pediatric population. Diagn Microbiol Infect Dis. 2008;62:157–61.
CDC. https://www.cdc.gov/flu/professionals/diagnosis/molecular-assays.htm. (2016).
Mahony JB, Petrich A, Smieja M. Molecular diagnosis of respiratory virus infections. Crit Rev Clin Lab Sci. 2011;48:217–49.
Chen MI, Barr IG, Koh GC, et al. Serological response in RT-PCR confirmed H1N1-2009 influenza a by hemagglutination inhibition and virus neutralization assays: an observational study. PLoS One. 2010;5:e12474.
Cruz AT, Cazacu AC, Greer JM, Demmler GJ. Performance of a rapid assay (Binax NOW) for detection of respiratory syncytial virus at a children’s hospital over a 3-year period. J Clin Microbiol. 2007;45:1993–5.
Borek AP, Clemens SH, Gaskins VK, et al. Respiratory syncytial virus detection by Remel Xpect, Binax now RSV, direct immunofluorescent staining, and tissue culture. J Clin Microbiol. 2006;44:1105–7.
Chan Y, Kuhn FA. An update on the classifications, diagnosis, and treatment of rhinosinusitis. Curr Opin Otolaryngol Head Neck Surg. 2009;17:204–8.
Dong G, Peng C, Luo J, et al. Adamantane-resistant influenza a viruses in the world (1902-2013): frequency and distribution of M2 gene mutations. PLoS One. 2015;10:e0119115.
CDC. https://www.cdc.gov/flu/professionals/antivirals/summary-clinicians.htm. (2017).
• Hayden FG. Advances in antivirals for non-influenza respiratory virus infections. Influenza Other Respir Viruses. 2013;7(Suppl 3):36–43. This review covers the types of treatments available for non-influenza rspiratory viral infections
•• Ison MG. Antiviral treatments. Clin Chest Med. 2017;38:139–53. This review comprehensively covers current available antiviral drugs against respiratory viral infections
Tang PK. Palivizumab prophylaxis in preterm infants. Lancet Respir Med. 2017;5:171.
Sugrue RJ. Interactions between respiratory syncytial virus and the host cell: opportunities for antivirus strategies? Expert Rev Mol Med. 2006;8:1–17.
Beigel J, Bray M. Current and future antiviral therapy of severe seasonal and avian influenza. Antivir Res. 2008;78:91–102.
Kiso M, Takahashi K, Sakai-Tagawa Y, et al. T-705 (favipiravir) activity against lethal H5N1 influenza A viruses. Proc Natl Acad Sci U S A. 2010;107:882–7.
Baranovich T, Wong SS, Armstrong J, et al. T-705 (favipiravir) induces lethal mutagenesis in influenza A H1N1 viruses in vitro. J Virol. 2013;87:3741–51.
Belser JA, Lu X, Szretter KJ, et al. DAS181, a novel sialidase fusion protein, protects mice from lethal avian influenza H5N1 virus infection. J Infect Dis. 2007;196:1493–9.
Moss RB, Hansen C, Sanders RL, et al. A phase II study of DAS181, a novel host directed antiviral for the treatment of influenza infection. J Infect Dis. 2012;206:1844–51.
DeVincenzo JP, Whitley RJ, Mackman RL, et al. Oral GS-5806 activity in a respiratory syncytial virus challenge study. N Engl J Med. 2014;371:711–22.
Mackman RL, Sangi M, Sperandio D, et al. Discovery of an oral respiratory syncytial virus (RSV) fusion inhibitor (GS-5806) and clinical proof of concept in a human RSV challenge study. J Med Chem. 2015;58:1630–43.
Wang G, Deval J, Hong J, et al. Discovery of 4′-chloromethyl-2′-deoxy-3′,5′-di-O-isobutyryl-2′-fluorocytidine (ALS-8176), a first-in-class RSV polymerase inhibitor for treatment of human respiratory syncytial virus infection. J Med Chem. 2015;58:1862–78.
DeVincenzo J, Cehelsky JE, Alvarez R, et al. Evaluation of the safety, tolerability and pharmacokinetics of ALN-RSV01, a novel RNAi antiviral therapeutic directed against respiratory syncytial virus (RSV). Antivir Res. 2008;77:225–31.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Kai Sen Tan, Yan Yan, Hsiao Hui Ong, Vincent T. K. Chow, Li Shi, and De-Yun Wang declare that they have no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Declaration of All Sources of Funding
This study was supported by grants from the National Medical Research Council (NMRC/CIRG/1362/2013 and NMRC/CIRG/1458/2016).
Additional information
This article is part of the Topical Collection on Rhinosinusitis
Rights and permissions
About this article
Cite this article
Tan, K.S., Yan, Y., Ong, H.H. et al. Impact of Respiratory Virus Infections in Exacerbation of Acute and Chronic Rhinosinusitis. Curr Allergy Asthma Rep 17, 24 (2017). https://doi.org/10.1007/s11882-017-0693-2
Published:
DOI: https://doi.org/10.1007/s11882-017-0693-2