Abstract
Purpose
In Japan, due to the increased incidence of cancer among the working population, it has become more important to support employees to achieve a balance between cancer treatment and work. This study aimed to clarify the predictors of resigning from employment after being diagnosed with cancer (post-cancer diagnosis [PCD] resignation) among Japanese employees.
Methods
As part of a Japanese national research project (Endo-Han), the investigators conducted a web-based survey of cancer survivors (CSs) in 2017. The investigators analyzed the risk factors for PCD resignation using a logistic regression model, including age at diagnosis, sex, cancer type, cancer stage, year of diagnosis, whether the patient held a managerial role, type of employment, and company size.
Results
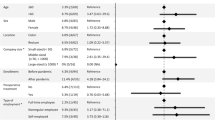
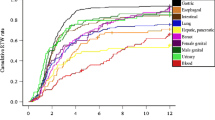
Of 750 employed Japanese CSs, 93 (12.4%) resigned from their jobs. The non-managers resigned more often (14.6%) than the managers (7.6%) (p = 0.007). The temporary workers exhibited the highest PCD resignation rates (22.2%), while the PCD resignation rates of the self-employed workers and permanent workers were 15.2% and 7.6%, respectively (p < 0.001). As the result of multivariate analysis, being female (odds ratio [OR], 3.67; 95%CI, 1.71–7.87), having hematological cancer (OR, 4.23; 95%CI, 1.37–13.04), having advanced cancer (OR, 2.48; 95%CI, 1.52–4.03), and being a temporary worker (OR, 2.51; 95%CI, 1.40–4.50) were identified as predictors of PCD resignation.
Conclusions
In total, 12.4% of Japanese employees quit their jobs after being diagnosed with cancer. Being female or a temporary worker and having advanced cancer were identified as predictors of PCD resignation. Regarding cancer type, hematological cancer was most strongly associated with PCD resignation.
Implication of Cancer Survivors
CSs who are females and temporary workers and have advanced cancer should be followed-up more carefully after cancer diagnosis for their work sustainability, by medical professionals, companies, and society.
Similar content being viewed by others
References
Verdecchia A, Francisci S, Brenner H, Gatta G, Micheli A, Mangone L, et al. Recent cancer survival in Europe: a 2000-02 period analysis of EUROCARE-4 data. Lancet Oncol. 2007;8(9):784–96.
Ito Y, Miyashiro I, Ito H, Hosono S, Chihara D, Nakata-Yamada K, et al. Long-term survival and conditional survival of cancer patients in Japan using population-based cancer registry data. Cancer Sci. 2014;105(11):1480–6.
Aziz NM. Cancer survivorship research: state of knowledge, challenges and opportunities. Acta Oncol. 2007;46(4):417–32.
Pryce J, Munir F, Haslam C. Cancer survivorship and work: symptoms, supervisor response, co-worker disclosure and work adjustment. J Occup Rehabil. 2007;17(1):83–92.
Ministry of Health L, Welfare, Japan. Report of Japanese goverment comittee for work support among Japanese cancer survivors “Gankanja keikensya no syurousien no arikata ni kansuru kentoukai houkokusyo” (in Japanese). 2014.
National Cancer Center J. Cancer registry and statistics. Cancer information service. 2014.
Mehnert A. Employment and work-related issues in cancer survivors. Crit Rev Oncol Hematol. 2011;77(2):109–30.
Endo M, Haruyama Y, Takahashi M, Nishiura C, Kojimahara N, Yamaguchi N. Returning to work after sick leave due to cancer: a 365-day cohort study of Japanese cancer survivors. J Cancer Surviv. 2015.
Ministry of Health Labor W, Japan. Jigyojou ni okeru tiryo to syokugyouseikatu ni okeru ryouritusien ni okeru gaidorain (Guideline for support for therapy and work life in Japanese workforce). 2016.
Amir Z, Moran T, Walsh L, Iddenden R, Luker K. Return to paid work after cancer: a British experience. J Cancer Surviv. 2007;1(2):129–36.
van Muijen P, Weevers NL, Snels IA, Duijts SF, Bruinvels DJ, Schellart AJ, et al. Predictors of return to work and employment in cancer survivors: a systematic review. Eur J Cancer Care (Engl). 2013;22(2):144–60.
Taskila T, Martikainen R, Hietanen P, Lindbohm ML. Comparative study of work ability between cancer survivors and their referents. Eur J Cancer. 2007;43(5):914–20.
Clarke TC, Christ SL, Soler-Vila H, Lee DJ, Arheart KL, Prado G, et al. Working with cancer: health and employment among cancer survivors. Ann Epidemiol. 2015;25(11):832–8.
Tamminga SJ, de Boer AG, Verbeek JH, Frings-Dresen MH. Return-to-work interventions integrated into cancer care: a systematic review. Occup Environ Med. 2010;67(9):639–48.
Feuerstein M, Todd BL, Moskowitz MC, Bruns GL, Stoler MR, Nassif T, et al. Work in cancer survivors: a model for practice and research. J Cancer Surviv. 2010;4(4):415–37.
de Boer AG, Taskila T, Ojajarvi A, van Dijk FJ, Verbeek JH. Cancer survivors and unemployment: a meta-analysis and meta-regression. JAMA. 2009;301(7):753–62.
Bradley CJ, Bednarek HL, Neumark D. Breast cancer survival, work, and earnings. J Health Econ. 2002;21(5):757–79.
Yabroff KR, Lawrence WF, Clauser S, Davis WW, Brown ML. Burden of illness in cancer survivors: findings from a population-based national sample. J Natl Cancer Inst. 2004;96(17):1322–30.
Taskila-Abrandt T, Pukkala E, Martikainen R, Karjalainen A, Hietanen P. Employment status of Finnish cancer patients in 1997. Psychooncology. 2005;14(3):221–6.
Ministry of Health L, Welfare, Japan. Labor Contract Act. Ministry of Health, Labor, Welfare, Japan; 2007.
Nilsson M, Olsson M, Wennman-Larsen A, Petersson LM, Alexanderson K. Return to work after breast cancer: women’s experiences of encounters with different stakeholders. Eur J Oncol Nurs. 2011;15(3):267–74.
Satariano WA, DeLorenze GN. The likelihood of returning to work after breast cancer. Public Health Rep. 1996;111(3):236–41.
Sampere M, Gimeno D, Serra C, Plana M, Martinez JM, Delclos GL, et al. Organizational return to work support and sick leave duration: a cohort of Spanish workers with a long-term non-work-related sick leave episode. J Occup Environ Med. 2011;53(6):674–9.
Short PF, Vasey JJ, Tunceli K. Employment pathways in a large cohort of adult cancer survivors. Cancer. 2005;103(6):1292–301.
Roelen CA, Koopmans PC, Groothoff JW, van der Klink JJ, Bultmann U. Sickness absence and full return to work after cancer: 2-year follow-up of register data for different cancer sites. Psychooncology. 2011;20(9):1001–6.
Park JH, Park EC, Park JH, Kim SG, Lee SY. Job loss and re-employment of cancer patients in Korean employees: a nationwide retrospective cohort study. J Clin Oncol. 2008;26(8):1302–9.
van Egmond MP, Anema JR, Singh A, van der Beek AJ, Duijts SF. Factors associated with (non-)participation of cancer survivors with job loss in a supportive return to work program. Support Care Cancer. 2016;24(7):3175–84.
Fiva JH, Haegeland T, Ronning M. Health status after cancer: does it matter which hospital you belong to? BMC Health Serv Res. 2010;10:204.
Tracy JK, Falk D, Thompson RJ, Scheindlin L, Adetunji F, Swanberg JE. Managing the cancer-work interface: the effect of cancer survivorship on unemployment. Cancer Manag Res. 2018;10:6479–87.
Inhestern L, Beierlein V, Bultmann JC, Moller B, Romer G, Koch U, et al. Anxiety and depression in working-age cancer survivors: a register-based study. BMC Cancer. 2017;17(1):347.
de Boer AG, Verbeek JH, Spelten ER, Uitterhoeve AL, Ansink AC, de Reijke TM, et al. Work ability and return-to-work in cancer patients. Br J Cancer. 2008;98(8):1342–7.
Lee S, McHale SM, Crouter AC, Hammer LB, Almeida DM. Finding time over time: longitudinal links between employed mothers’ work-family conflict and time profiles. J Fam Psychol. 2017;31(5):604–15.
Ministry of Internal Affairs and Communications J. Survey on time use and leisure activities “Syakaiseikatsukihontyosa” (in Japanese). 2016.
Spelten ER, Verbeek JH, Uitterhoeve AL, Ansink AC, van der Lelie J, de Reijke TM, et al. Cancer, fatigue and the return of patients to work-a prospective cohort study. Eur J Cancer. 2003;39(11):1562–7.
Horsboel TA, Nielsen CV, Andersen NT, Nielsen B, de Thurah A. Risk of disability pension for patients diagnosed with haematological malignancies: a register-based cohort study. Acta Oncol. 2014;53(6):724–34.
Joachim Weis MH. Cancer-related fatigue. 2015.
Hematology JSo. The clinical guideline of haematological malignancies (in Japanese). 2018.
Ahn E, Cho J, Shin DW, Park BW, Ahn SH, Noh DY, et al. Impact of breast cancer diagnosis and treatment on work-related life and factors affecting them. Breast Cancer Res Treat. 2009;116(3):609–16.
Mehnert A, Koch U. Predictors of employment among cancer survivors after medical rehabilitation--a prospective study. Scand J Work Environ Health. 2013;39(1):76–87.
Rottenberg Y, Ratzon NZ, Cohen M, Hubert A, Uziely B, de Boer AG. Unemployment risk at 2 and 4 years following colorectal cancer diagnosis: a population based study. Eur J Cancer. 2016;69:70–6.
Bennett S, Pigott A, Beller EM, Haines T, Meredith P, Delaney C. Educational interventions for the management of cancer-related fatigue in adults. Cochrane Database Syst Rev. 2016;11:CD008144.
Paltrinieri S, Vicentini M, Mazzini E, Ricchi E, Fugazzaro S, Mancuso P, et al. Factors influencing return to work of cancer survivors: a population-based study in Italy. Support Care Cancer. 2019.
Statistic Bureau MoIAaC, Japan. Statistical handbook of Japan. 2018.
Brady S, O’Connell T. Review of Irish Civil Service sickness absence referrals 2008-10. Occup Med (Lond). 2013;63(5):365–8.
Funding
This study was funded by grants from the Japanese Ministry of Health, Labour and Welfare (Research Grant: Gan-taisaku-ippan-012) to Motoki Endo. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Endo, M., Muto, G., Imai, Y. et al. Predictors of post-cancer diagnosis resignation among Japanese cancer survivors. J Cancer Surviv 14, 106–113 (2020). https://doi.org/10.1007/s11764-019-00827-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-019-00827-0