Abstract
In the context of the COVID-19 pandemic and overloaded hospitals, a central issue is the need to define reliable and consensual criteria for hospitalization or outpatient management in mild cases of COVID-19. Our aim was to define an easy-to-use clinical rule aiming to help emergency physicians in hospitalization or outpatient management decision-making for patients with suspected or confirmed SARS-CoV-2 infection (the HOME-CoV rule). The Delphi method was used to reach a consensus of a large panel of 51 experts: emergency physicians, geriatricians, infectious disease specialists, and ethical consultants. A preliminary list of eligible criteria was compiled based on a literature review. Four rounds of anonymized expert consultations were performed. The experts were asked to score each item as relevant, possibly relevant and non-relevant, as major or minor, and to choose the cut-off. They were also able make suggestions and remarks. Eight criteria constituting the HOME-CoV were selected: six correspond to the severity of clinical signs, one to the clinical course (clinically significant worsening within the last 24 h), and the last corresponds to the association of a severe comorbidity and an inadequate living context. Hospitalization is deemed necessary if a patient meets one or more of the criteria. In the end, 94.4% of the experts agreed with the defined rule. Thanks to the Delphi method, an absolute consensus was obtained of a large panel of experts on the HOME-CoV rule, a decision-making support mechanism for clinicians to target patients with suspected or confirmed COVID-19 requiring hospitalization.
Trial registration: NCT04338841.
Similar content being viewed by others
Introduction
The novel coronavirus (SARS-CoV-2) has spread worldwide and the coronavirus disease (COVID-19) is responsible for more than 2.5 million cases globally (04/23/2020) [1]. The classification of COVID-19 as a pandemic by the World Health Organization on 11 March 2020 alerted every country-specific health care system to the need for an urgent response to the requirements and challenges of this unprecedented situation. Because the spectrum of forms of the disease varies from asymptomatic to severe, public health systems have been mobilized at all levels [2]. Most cases during the outbreak of COVID-19 in China were reported by the Chinese Center for Disease Control and Prevention (CDC) team in a large cohort of 72,314 patients and 81% were classified as mild (non-pneumonia and mild pneumonia) and 14% were severe [3]. There is growing concern that the healthcare system, and intensive care units (ICU) and emergency departments (ED) in particular, will not be able to cope with the scale of the outbreak. Many models have predicted demand would rapidly exceed hospital capacities in most countries [4,5,6]. The excessive hospitalization of patients with only mild symptoms may lead to overloaded hospitals. In this context, the decision between hospitalization or outpatient management in cases of mild COVID-19 in ED is crucial.
In pneumonia patients or in patients with sepsis, many risk assessment score matrices and decision-making tools, such as the Pulmonary Severity Index (PSI), CRB 65, CURB65, sequential organ failure assessment (SOFA) and quick sequential organ failure assessment (qSOFA), exist to identify low-risk patients [7,8,9,10]. However, most of them cannot be used to quickly identify low-risk patients in ED because they incorporate biological or imaging parameters (PSI, CURB-65, SOFA). In addition, they do not integrate all pragmatic elements that are taken into account in an orientation decision such as decompensated comorbidity or inability to take medication or inadequate follow-up care once the patient has been discharged.
Our aim was to define an easy-to-use clinical rule aiming to help emergency physicians decide between hospitalization or outpatient management for patients with suspected or confirmed SARS-CoV-2 infection (the HOME-CoV rule: Hospitalization or Outpatient ManagEment of patients with SARS-CoV-2 infection).
Methods
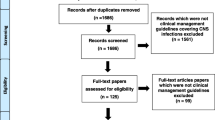
A Delphi method was used to develop a list of items that will constitute the HOME-CoV rule. In short, the Delphi method consists of a multiple-round questionnaire sent to a panel of experts who, through participating in a series of rounds, collectively identify relevant candidate items [11]. After each round, the experts are given results of the group trends and are asked to reconsider their initial opinion for items with low agreements (< 75%) in the light of these trends. A consensus for decision-making is usually obtained by four rounds. We used an electronical survey through the built-in tools GoogleForms® website with the aim to finish the process in less than 2 weeks.
Preliminary phase
The main investigators (DD, RM and PMR) began by reviewing the literature on the characteristics of COVID-19 patients at high risk of progression to a severe illness. Because of the limited published data, pre-print studies were also considered. A preliminary list of pre-existing conditions and clinical characteristics associated with a greater risk of disease progression to a severe illness was defined by the study’s scientific committee composed of 7 experts in emergency medicine, infectious diseases, geriatrics, and ethics. The preliminary list included 10 clinical and disease course criteria, 22 comorbidities and treatments, and 3 living conditions (Table 1).
Delphi panel
An invitation to participate to the Delphi method was sent to 64 French and Belgian physicians working in ED, infectious diseases departments, ICU and geriatric medicine and two experts in ethics. They were selected according to their clinical experience in rule-based decision-making and their interest in the field of COVID-19. The main investigators were not included in the panel of experts for the subsequent Delphi method questionnaire. The experts were asked to respond to each item in regard to the purpose of the HOME-CoV rule.
Data collection
The four-round Delphi method took place between April 4 and April 16, 2020. Experts were asked to rate each criterion for its relevance (relevant, possibly relevant, non-relevant), for the best cut-off value (1–4 proposed cut-off value if applicable) and for its level of significance (major or minor criteria) (Table 1). One major criterion or two combined minor criteria will require hospitalization.
For the first round, a questionnaire was sent through an electronic survey with the preliminary list of criteria selected by the scientific committee. The experts were asked to score each item into 3 categories of relevance (relevant, possibly relevant, and non-relevant) and 2 categories of significance (major or minor). For non-binary items (ordinal or continuous variables), the experts had to select a “cut-off value” among 1–4 proposals sourced from research literature. They could also propose additional criteria or other cut-off values and make anonymous comments. The duration of each round was 72 h with an electronic reminder every 24 h. The results were analyzed by the main investigators, with details of the experts who made suggestions or comments anonymized. At the end of the first and the second rounds, items considered as relevant with a strong agreement between experts (≥ 75%) were selected and incorporated in the rule. Items considered as non-relevant or facultative by 75% of the experts were excluded. The same rule was applied to consider each item as major or minor and to define the cut-off. Values that achieved an agreement ≥ 75% were selected. Criteria that did not fulfill these conditions were subjected to the next round. On the basis of the comments of the experts, the main investigators proposed some groupings and/or clarifications and submitted them to the experts again.
In the second round, the experts were asked to reconsider their opinions and to score the new proposals taking into account the results of the last step, the group trends, and the anonymized comments of the others.
In the third round, the option “possibly relevant” was removed as well as the cut-off value with the lowest agreement for those items concerned. The experts were so asked to make a choice between only two options for the remaining criteria: relevant or non-relevant; major or minor; cut-off 1 or cut-off 2.
Finally, in the last round, the experts were asked to validate or reject the overall criteria constituting the HOME-CoV rule.
Ethics
This research project is part of an important trial that obtained approval from the Comité de Protection des Personnes Ouest IV—Nantes on 4th March 2020 (36/20_2). The sponsor of the study is CHU d’Angers (Angers University Hospital), Delegation for Clinical Research and Innovation. Approval for this study was obtained from all participants who gave their written informed consent.
Results
Among the 64 who were approached to participate, 51 experts agreed (80%). Among them, 47 experts participated in the first and the second rounds (92%), 42 (82%) in the third, and 37 (72.5%) in the fourth round of the Delphi method.
In the first round, among the 35 items of the preliminary list, seven items were classified as relevant (i.e., respiratory rate, peripheral capillary oxygen saturation, ability to speak, blood pressure, consciousness or confusion, home follow-up impossible, and clinically significant worsening within 24 h). Twelve items were rejected. Details, and particularly those pertaining to the classification as major or minor and the cut-off values, are mentioned (Supplementary Table 1).
In the second round, 18 unclassified items were proposed to the experts and 3 more items were classified as relevant (i.e., chronic severe respiratory disease, inappropriate dwelling in which containment is complicated, and lack of support person), and 3 items were rejected (Supplementary Table 2).
In the third round all remaining items were classified: 3 as relevant (i.e., severe cognitive disorder, chronic heart failure, and immunodepression); and 1 was rejected. Grouping severe comorbidity and inadequate living conditions together in one criterion was proposed. Severe comorbidity includes severe chronic respiratory disease (unstable asthma, chronic obstructive pulmonary disease (COPD) stage III or IV, and respiratory failure with continuous oxygen therapy), chronic heart failure (NYHA ≥ III), severe cognitive disorder, or immunodepression (primary immunodeficiency, uncontrolled HIV, immunosuppressive drug, or chemotherapy). Inadequate living conditions include inappropriate dwelling (homeless, frail relative at home, long term care institution), lack of support person (family member or friend), or home follow-up impossible (Supplementary Table 3).
The final rule includes 8 criteria: 6 items correspond to clinical signs of severity, 1 to the disease course and the last 1 to the association of a severe comorbidity and an inappropriate living condition (Table 2). The presence of one or more criteria should lead the physician to consider hospitalization.
In the last round, the final HOME-CoV rule was submitted to the experts and achieved an agreement of 94.4% of the experts (n = 34/36).
Discussion
Using a Delphi method, the panel of 51 experts designed the HOME-CoV rule based on 8 clinical criteria to help physicians decide between hospitalizing patients with mild COVID-19 symptoms or treating them as outpatients. Hospitalization is deemed necessary if a patient with COVID-19 meets one or more criteria consisting of 6 major clinical signs, has experienced clinically significant worsening within the last 24 h, or has a severe comorbidity and inadequate living conditions. Conversely, when no criteria of the rule are met, outpatient management should be considered. For example, a 54-year-old man presenting to the ED with symptoms consistent with COVID-19 (ageusia, myalgia, and fever) and unable to speak or to count without taking a breath more than 6 s should need hospitalization. A 78-year-old woman with chronic heart failure (NYHA III) presenting mild dyspnea but no desaturation or other clinical signs of severity and who lives with her husband in a reassuring environment can be treated on an outpatient basis with instructions on warning signs to watch.
Due to the rapid spread of the novel coronavirus SARS-CoV-2, no high-grade recommendation is yet available for management of COVID-19 patients. Most guidelines are based on expert opinion with a very low certainty of evidence. Almost all suggest that the decision to manage a patient as an inpatient or an outpatient should be made on a case-by-case basis or recommend applying a triage tool all the while without specifying which one to use [12,13,14]. SOFA score on admission, age, gender, d-dimer, serum lactate dehydrogenase, C-reactive protein level, the coefficient of variation of red blood cell distribution width, lymphocyte count, blood urea nitrogen, direct bilirubin, albumin, and quantitative evaluation on CT scan have all been associated with severe forms of COVID-19 and mortality [3, 15,16,17,18,19]. However, these risk factors were identified in cohorts of patients with COVID-19 who had been hospitalized and none of them has been evaluated to guide the management of suspected COVID-19 patients on admission in the ED. Moreover, like most previous risk assessment scores for sepsis or pneumonia incorporating biological or imaging parameters, they cannot be used to quickly identify low-risk patients in ED [7,8,9].
The best methodology for developing a decision rule is to perform multivariate logistic regression on a derivation important cohort of patients and to validate the rule in another important cohort. This was not possible for our purpose in lack of large data basis of COVID-19 patients including patients hospitalized as well as patients managed at home. The Delphi method is widely used to provide an expert consensus based on available data and expert experiences through a multiple-round questionnaire [20]. This method is recommended when scientific data are limited. For example, it has been previously used for building SEPSIS-3 consensus, for the definition of appropriate management of outpatient parenteral antimicrobial therapy, and for elaborating a consensual definition of de-escalation of beta-lactams [21,22,23]. The use of an Internet-based version of the Delphi process allowed us to complete the fourth round in less than two weeks. This “electronic Delphi” method was motivated by the sanitary context of containment and the urgent need for COVID-19 management guidelines while allowing for the recruitment of a large panel of experts. Despite the exceptional sanitary situation, the high level of participation and the almost absolute expert consensus on the final rule (94.4%) are a pledge of quality and may assure a high level of acceptance of this guideline by physicians.
The HOME-CoV rule incorporates 6 major clinical signs, 3 concerning respiratory status, 2 hemodynamic status, and one neurological status. Most of them were taken into account in previous severity rules for sepsis and/or pneumonia (respiratory rate, pulse oxygen saturation, systolic blood pressure, heart rate, confusion, or impaired consciousness). Nevertheless, the cut-offs were debated between experts. Most of the time, the consensus was reached on an attitude that should be adopted with care with the aim to apply the rule as a guide for the majority of patients but not as an absolute decision-making rule. For example, SpO2 at 94% in ambient air is a severity criterion for a young person without comorbidity but may be a usual feature for an old person or a patient with chronic respiratory disease. The cut-off for the respiratory rate decided upon (≥ 25/min) may appear as an intermediate choice in comparison to other rules [7, 9, 21]. However, it corresponds to the value found in the epidemiological study of COVID-19 patients in China [17]. The ability to talk or to count without breathing is a less common criterion but currently used in the unformal assessment of dyspneic patients [24, 25]. By defining 8 s as the time cut-off, the HOME-CoV rule proposes a standardization of this criterion. From the outset, the experts considered a clinically significant worsening within the last 24 h to be a major criterion. This criterion may appear, at least partly, subjective. However, the clinical course of COVID-19 may be a good indicator of the short-term risk of complication, as rapid progressions to severe hypoxemia have been observed [26].
The HOME-CoV rule may be an important help in decision-making for physicians. Faced with a lack of reliable criteria and recommendations, physicians use their individual gestalt perception to decide whom to hospitalize or to manage as an outpatient. However, gestalt evaluation is associated with a great variability among physicians and an overestimation of patients’ short-term risk of adverse outcome [27, 28]. In the specific field of the COVID-19 pandemic, gestalt accuracy may be even lower than expected in other circumstances and hospitalizing patients when there is “any concern for rapid deterioration or an inability to return promptly to hospital” may underestimate the number of patients who can be managed at home and lead to hospitals becoming overcrowded. Indeed, among 1099 patients hospitalized in China for COVID-19, 6.1% required mechanical ventilation and 41.3% needed oxygen therapy, indicating that a significant proportion would not have required specific in-hospital care [2]. In cases of pneumonia, the use of a clinical prediction rule has been proven to improve the identification of low-risk patients, to increase the rate of patients managed at home, and to reduce costs of medical care [27, 28]. At least the same benefit could be expected as a result of deploying the HOME-CoV rule in ED. This rule could be also useful for general practitioners and physicians in older nursing home.
Nevertheless, our study has some limitations. Most of the experts consulted were French and their personal experiences in COVID-19 management were recent and varied. The rule does not apply to patients with rare and/or very specific comorbidity or in specific clinical situations. It does not take into account some criteria that appear, in recent data, to be death risk factors for SARS-CoV-2 infection, such as obesity, diabetes, and hypertension [29, 30]. Indeed, the real direct impact of these factors is still unknown, as there has still been no large-scale international epidemiological study providing multivariate analysis of all possible risk factors. The decision of the expert panel may facilitate the deployment of the rule in many countries and for other viral pneumonia. Finally, in the absence of systematic screening, the rule may only apply to symptomatic patients for whom the search for infection has been carried out in the ED or prior to admission, and not to all asymptomatic patients or those without suggestive symptoms.
The HOME-CoV rule achieved by a Delphi method provides an easy-to-use clinical tool for physicians in deciding between hospitalization or outpatient management for patients with suspected or confirmed SARS-CoV-2 infection.
References
WHO situation reports. Novel Coronavirus (2019-nCoV) situation reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. Accessed 17 Apr 2020
Guan W-J, Ni Z-Y, Hu Y et al (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. https://doi.org/10.1056/NEJMoa2002032
Wu Z, McGoogan JM (2020) Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. JAMA. https://doi.org/10.1001/jama.2020.2648
Massonnaud C, Roux J, Crépey P (2020) COVID-19: Forecasting short term hospital needs in France. medRxiv. https://doi.org/10.1101/2020.03.16.20036939
Remuzzi A, Remuzzi G (2020) COVID-19 and Italy: what next? Lancet. https://doi.org/10.1016/S0140-6736(20)30627-9
Gilbert M, Pullano G, Pinotti F et al (2020) Preparedness and vulnerability of African countries against importations of COVID-19: a modelling study. Lancet 395:871–877. https://doi.org/10.1016/S0140-6736(20)30411-6
Fine MJ, Auble TE, Yealy DM et al (1997) A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 336:243–250. https://doi.org/10.1056/NEJM199701233360402
Marti C, Garin N, Grosgurin O et al (2012) Prediction of severe community-acquired pneumonia: a systematic review and meta-analysis. Crit Care 16:R141. https://doi.org/10.1186/cc11447
Aujesky D, Auble TE, Yealy DM et al (2005) Prospective comparison of three validated prediction rules for prognosis in community-acquired pneumonia. Am J Med 118:384–392. https://doi.org/10.1016/j.amjmed.2005.01.006
Vincent JL, Moreno R, Takala J et al (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710. https://doi.org/10.1007/BF01709751
Kötter T, Blozik E, Scherer M (2012) Methods for the guideline-based development of quality indicators—a systematic review. Implement Sci 7:21. https://doi.org/10.1186/1748-5908-7-21
Infectious Diseases Society of America Guidelines on the Treatment and Management of Patients with COVID-19. https://www.idsociety.org/practice-guideline/covid-19-guideline-treatment-and-management/. Accessed 17 Apr 2020
Canada PHA (2020) Clinical management of patients with moderate to severe COVID-19—Interim Guidance. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/clinical-management-covid-19.html. Accessed 17 Apr 2020
CDC (2020) Coronavirus Disease 2019 (COVID-19). https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html. Accessed 21 Apr 2020
Ji D, Zhang D, Xu J et al (2020) Prediction for progression risk in patients with COVID-19 pneumonia: the CALL Score. Clin Infect Dis. https://doi.org/10.1093/cid/ciaa414
Gong J, Ou J, Qiu X et al (2019) A tool to early predict severe corona virus disease 2019 (COVID-19) : a multicenter study using the risk nomogram in Wuhan and Guangdong, China. Clin Infect Dis. https://doi.org/10.1093/cid/ciaa443
Zhou F, Yu T, Du R et al (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. https://doi.org/10.1016/S0140-6736(20)30566-3
Mo P, Xing Y, Xiao Y et al (2020) Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clin Infect Dis. https://doi.org/10.1093/cid/ciaa270
Li K, Fang Y, Li W et al (2020) CT image visual quantitative evaluation and clinical classification of coronavirus disease (COVID-19). Eur Radiol. https://doi.org/10.1007/s00330-020-06817-6
Diamond IR, Grant RC, Feldman BM et al (2014) Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol 67:401–409. https://doi.org/10.1016/j.jclinepi.2013.12.002
Singer M, Deutschman CS, Seymour CW et al (2016) The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315:801–810. https://doi.org/10.1001/jama.2016.0287
Berrevoets MAH, Ten Oever J, Oerlemans AJM, Kullberg BJ, Hulscher ME, Schouten JA (2020) Quality indicators for appropriate outpatient parenteral antimicrobial therapy in adults: a systematic review and RAND-modified Delphi procedure. Clin Infect Dis 70:1075–1082. https://doi.org/10.1093/cid/ciz362
Weiss E, Zahar J-R, Lesprit P et al (2015) Elaboration of a consensual definition of de-escalation allowing a ranking of β-lactams. Clin Microbiol Infect 21:649. https://doi.org/10.1016/j.cmi.2015.03.013
Reddel HK, FitzGerald JM, Bateman ED et al (2019) GINA 2019: a fundamental change in asthma management: treatment of asthma with short-acting bronchodilators alone is no longer recommended for adults and adolescents. Eur Respir J. https://doi.org/10.1183/13993003.01046-2019
Chorin E, Padegimas A, Havakuk O et al (2016) Assessment of respiratory distress by the Roth Score. Clin Cardiol 39:636–639. https://doi.org/10.1002/clc.22586
Lescure F-X, Bouadma L, Nguyen D et al (2020) Clinical and virological data of the first cases of COVID-19 in Europe: a case series. Lancet Infect Dis. https://doi.org/10.1016/S1473-3099(20)30200-0
Poses RM, McClish DK, Bekes C, Scott WE, Morley JN (1991) Ego bias, reverse ego bias, and physicians’ prognostic. Crit Care Med 19:1533–1539. https://doi.org/10.1097/00003246-199112000-00016
Fine MJ, Hough LJ, Medsger AR et al (1997) The hospital admission decision for patients with community-acquired pneumonia. Results from the pneumonia Patient Outcomes Research Team cohort study. Arch Intern Med 157:36–44
Simonnet A, Chetboun M, Poissy J et al (2020) High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity (Silver Spring). https://doi.org/10.1002/oby.22831
Guo W, Li M, Dong Y et al (2020) Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes Metab Res Rev. https://doi.org/10.1002/dmrr.3319
Acknowledgements
HOME-CoV scientific committee and expert group: Andrianjafy H., Emergency Department, GH Nord-Essonne, Longjumeau, France; Annweiler C., Geriatric Department, CHU Angers, Angers, France; Armand A., Emergency Department, CHU Angers, Angers, France; Baudin L., Emergency Department, CH Cholet, Cholet, France; Bekhir L., Emergency Department, Cliniques universitaires saint Luc, Bruxelles, Belgium; Benezit F., Department of infectious disease, CHU Rennes, Rennes, France; Benhammouda K., Emergency Department, CH Colmar, Colmar, France; Bissolokele P., Emergency Department, CH Libourne, Libourne, France; Blanchi S., Department of infectious disease, CH Le Mans, Le Mans, France; Boiveau V., Emergency Department, CHU Angers, Angers, France; Bouiller K., Department of infectious disease, CHU Besançon, Besançon, France; Bouillon J.-B., Emergency Department, CHU Clermont Ferrand, Clermont Ferrand, France; Brice C., Emergency Department, CH Saint Brieuc, Saint Brieuc, France; Brunel A.-S., Department of infectious disease, CHU Besançon, Besançon, France; Cayeux C., Emergency Department, CH Remiremont, Remiremont, France; Cazenave B., Department of infectious disease, GHT Yvelines-Nord, Saint Germain en Laye, France; Chauvin A., Emergency Department, APHP – Hôpital Lariboisière, Paris, France; Claessens Y-E., Emergency Department, Princess Grace Hospital, Monte Carlo, Monaco; Cormier H., Department of infectious disease, CHU Angers, Angers, France; Coustilleres F., Department of infectious disease, CHU Tours, Tours, France; Crochette N., Department of infectious disease, CH Le Mans, Le Mans, France; Dall Acqua D., Emergency Department, CH Vichy, Vichy, France; Douillet D., Emergency Department, CHU Angers, Angers, France; Dupriez F., Emergency Department, Cliniques universitaires saint Luc, Bruxelles, Belgium; Friou E., Emergency Department, CHU Angers, Angers, France; Gangloff C., Emergency Department, CHU Rennes, Rennes, France; Gennai S., Emergency Department, CHU Reims, Reims, France; Joly L.-M., Emergency Department, CHU Rouen, Rouen, France; Karam H.-H., Emergency Department, CHU Limoges, Limoges, France; Le Bot A., Department of infectious disease, CHU Rennes, Rennes, France; Lemaignen A., Department of infectious disease, CHU Tours, Tours, France; Leroy A., Emergency Department, CH Troyes, Troyes, France; Mahieu R., Department of infectious disease, CHU Angers, Angers, France; Marchant N., Emergency Department, CH Alpes Lemant, Contamine sur Avre, France; Marjanovic N., Emergency Department, CHU Poitiers, Poitiers, France; Montassier E., Emergency Department, CHU Nantes, Nantes, France; Morin F., Emergency Department, CHU Angers, Angers, France; Pasquier J., Department of infectious disease, CHU Martinique, Martinique, France; Patrat-Delon S., Department of infectious disease, CHU Rennes, Rennes, France; Penaloza A., Emergency Department, Cliniques universitaires saint Luc, Bruxelles, Belgium; Plantefeve G., Emergency Department, CH Argenteuil, Argenteuil, France; Roy P.-M., Emergency Department, CHU Angers, Angers, France; Sanderink D., Department of infectious disease, CHU Angers, Angers, France; Savary D., Emergency Department, CHU Angers, Angers, France; Schmidt J., Emergency Department, CHU Clermont Ferrand, Clermont Ferrand, France; Schotte T., Emergency Department, CH Le Mans, Le Mans, France; Soulie C., Emergency Department, CH Cholet, Cholet, France; Tchangai-Kao S., Department of infectious disease, CH Saint Nazaire, Saint Nazaire, France; Thiebaud P.-C., Emergency Department, APHP-Hôpital Saint Antoine, Paris, France; Timsit E., Emergency Department, CHU Dijon, Dijon, France; Trabattoni E., Emergency Department, APHP – Hôpital saint Joseph, Paris, France; Turmel J.-M., Department of infectious disease, CHU Martinique, Martinique, France; Vandamme Y.-M., Department of infectious disease, CHU Angers, Angers, France; Violeau M., Emergency Department, CH Niort, Niort, France; Yombi J.-C., Department of infectious disease, Cliniques universitaires saint Luc, Bruxelles, Belgium.
Author information
Authors and Affiliations
Consortia
Contributions
DD and PMR have designed the study; DD, RM, and PMR elaborated the initial list but did not take part in the Delphi consensus; CA, VB, YMV, and AA were part of the first expert group that compiled the first list of criteria; DD, RM and PMR were moderators of the Delphi method and collected the data. All the authors (except DD, RM, and PMR) were part of the group of experts and contributed greatly to the quality of this work through their valuable comments; DD, RM, and PMR drafted the manuscript and all authors contributed substantially to its revision; DD, RM, and PMR take responsibility for the paper as a whole.
Corresponding author
Ethics declarations
Conflict of interest
We declare no conflicts of interest.
Statements on human and animal rights
This research project is part of an important trial that obtained approval from the Comité de Protection des Personnes Ouest IV—Nantes on 4th March 2020 (36/20_2). The sponsor of the study is CHU d’Angers (Angers University Hospital), Delegation for Clinical Research and Innovation.
Informed consent
Approval for this study was obtained from all participants who gave their written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of the HOME-CoV expert group listed in acknowledgement section.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Douillet, D., Mahieu, R., Boiveau, V. et al. Outpatient management or hospitalization of patients with proven or suspected SARS-CoV-2 infection: the HOME-CoV rule. Intern Emerg Med 15, 1525–1531 (2020). https://doi.org/10.1007/s11739-020-02483-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-020-02483-0