Abstract
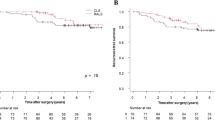
Robotic colorectal surgery is gaining popularity. The objective of this study was to compare clinical and cancer outcomes in propensity-score matched cohorts (PSM-1:1) undergoing colorectal cancer (CRC) surgery performed using laparoscopic or robotic surgery in a single institution. A PSM cohort comparison was performed in a tertiary referral cancer and National accredited rectal cancer surgery centre. Patients with CRC undergoing laparoscopic or robotic resection with curative intent from 2016 to 2019 (inclusive) were assessed for inclusion. Matched cohorts were selected using a 1:1 ratio. Statistical analysis was performed using SPSS, version 22. 128 patients were analysed [laparoscopic (n = 64); robotic (n = 64)]. Median age was 64 years (29–84 years). 55% (n = 70) of patients were male, 45% female (n = 58). SSI rates were slightly lower in the robotic group [10.9% (n = 7) v 12.5% (n = 8) p = 0.40]. Anastomotic leak rates were equal in both groups [5.4% (n = 3)]. All but one patient received an R0 resection in each group, median LNY was 14 in the robotic group and 12 in the laparoscopic group (p = 0.004) and no difference in disease recurrence (p = 0.465) or survival (p = 0.886) was observed. Structured introduction of a robotic colorectal programme over a 3-year period has resulted in equivalent outcomes with an established laparoscopic programme for CRC.


Similar content being viewed by others
References
I. agency for research in Cancer (2019) International agency for research in cancer. [Online]. https://gco.iarc.fr/today/online-analysis-map?v=2018&mode=population&mode_population=continents&population=900&populations=900&key=asr&sex=0&cancer=39&type=0&statistic=5&prevalence=0&population_group=0&ages_group%5B%5D=0&ages_group%5B%5D=17&nb_items=5&grou. Accessed 02 Sep 2019
ASCO “Cancer Net.” [Online]. https://www.cancer.net/cancer-types/colorectal-cancer/statistics. Accessed 2 Sep 2019
Sivathondan PC, Jayne DG (2018) The role of robotics in colorectal surgery. Ann R Coll Surg Engl 100:42–53
Ozben V et al (2020) Robotic complete mesocolic excision for transverse colon cancer can be performed with a morbidity profile similar to that of conventional laparoscopic colectomy. Tech Coloproctol
Sheetz K, Claflin J, Dimick J (2020) Trends in the adoption of robotic surgery for common surgical procedures. JAMA Netw Open 3(1):e1918911
Jayne D et al (2017) Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer the rolarr randomized clinical trial. JAMA J Am Med Assoc 318(16):1569–1580
Stevenson ARL et al (2015) Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA J Am Med Assoc 314(13):1356–1363
Fleshman J, Branda M, Sargent DJ et al (2015) Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA J Am Med Assoc 314(32):1346–1355
Kang SB, Ji WP, Jeong SY et al (2010) Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol 11:637–645
Guillou PJ, Quirke P, Thorpe H et al (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial). Lancet 365(9472):1728–1726
Talamini MA, Hanly EJ (2004) Robotic abdominal surgery. Am J Surg 188(4):19–26
Kim NK, Kim YW, Cho MS (2015) Total mesorectal excision for rectal cancer with emphasis on pelvic autonomic nerve preservation: expert technical tips for robotic surgery. Surg Oncol 24(3):172–180
Panteleimonitis S, Ahmed J, Harper M, Parvaiz A (2016) Critical analysis of the literature investigating urogenital function preservation following robotic rectal cancer surgery. World J Gastrointest Surg 8(11):744
Kim HJ, Choi GS, Park JS, Park SY, Yang CS, Lee HJ (2018) The impact of robotic surgery on quality of life, urinary and sexual function following total mesorectal excision for rectal cancer: a propensity score-matched analysis with laparoscopic surgery. Color Dis 20(5):O103–O113
Luca F et al (2018) Sexual and urinary outcomes in robotic rectal surgery: review of the literature and technical considerations. Updates Surg 70(3):415–421
Miskovic D et al (2019) European consensus on the standardization of robotic total mesorectal excision for rectal cancer. Color Dis 21(3):270–276
Strasberg S, Clavien PA, Sanabria JR (1992) Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery 111(5):518–526
Berriós-Torres SI et al (2017) Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg 152(8):784–791
Rahbari NN, Weitz J, Hohenberger W, Heald RJ, Moran B, Ulrich A, Holm T, Wong WD, Tiret E, Moriya Y, Laurberg S, den Dulk M, van de Velde C (2010) Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery 147(3):339–351
Chapman SJ, Thorpe G, Vallance AE, Harji DP, Lee MJ, Fearnhead NS (2019) Systematic review of definitions and outcome measures for return of bowel function after gastrointestinal surgery. BJS Open 3(1):1–10
Wittekind C, Sobin LH, Gospodarowicz MK (2009) TNM classification of malignant tumours, 7th edn. Wiley-Blackwell
D’Agostino RB Jr (1998) Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med 17:2265–2281
Agha R, Muir G (2003) Does laparoscopic surgery spell the end of the open surgeon? J R Soc Med 96(11):544–546
Connelly TM, Malik Z, Sehgal R, Byrnes G, Coffey JC, Peirce C (2019) The 100 most influential manuscripts in robotic surgery: a bibliometric analysis. J Robot Surg 0123456789
Khan JS, Banerjee AK, Kim S-H, Rockall TA, Jayne DG (2018) Robotic rectal surgery has advantages over laparoscopic surgery in selected patients and centres. Color Dis 20(10):845–853
Broholm M, Pommergaard HC, Gögenür I (2015) Possible benefits of robot-assisted rectal cancer surgery regarding urological and sexual dysfunction: a systematic review and meta-analysis. Color Dis 17(5):375–381
Park SY, Choi GS, Park JS, Kim HJ, Ryuk JP (2014) Urinary and erectile function in men after total mesorectal excision by laparoscopic or robot-assisted methods for the treatment of rectal cancer: a case-matched comparison. World J Surg 38:1834–1842
D’Annibale A, Pernazza G, Monsellato I, Pende V, Lucandri G, Mazzocchi P et al (2013) Total mesorectal excision: a comparison of oncological and functional outcomes between robotic and laparoscopic surgery for rectal cancer. Surg Endosc 27(6):1887e1895
Acknowledgements
I would like to thank all members of the laparoscopic and robotic-assisted surgery programmes at University Hospital Limerick for their contribution to the clinical practice upon which this research was based.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Christina A Fleming, Muhammad F Ullah, Kah Hoong Chang, Emma McNamara, David Waldron, Eoghan Condon, J Calvin Coffey, Colin Peirce declares that s/he has no conflict of interest.
Ethical approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fleming, C.A., Ullah, M.F., Chang, K.H. et al. Propensity score-matched analysis comparing laparoscopic to robotic surgery for colorectal cancer shows comparable clinical and oncological outcomes. J Robotic Surg 15, 389–396 (2021). https://doi.org/10.1007/s11701-020-01116-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-020-01116-0