Abstract
Background
Reports of long-term (> 5–15-year) outcomes assessing the safety and efficacy of primary revisional laparoscopic sleeve gastrectomy (LSG) are few.
Methods
Retrospective long-term comparisons of primary (pLSG) and revisional (rLSG) procedures were matched for gender, age ± 5 years, and body mass index (BMI) ± 5 kg/m2. Weight loss, associated medical condition status, and patient satisfaction were evaluated.
Results
Between May 1, 2006, and December 31, 2016, 194 matched patients with severe obesity (mean BMI 44.1 ± 6.7 kg/m2; age 44.2 ± 10.0 years, 67.0% female) underwent pLSG (n = 97) or rLSG (n = 97) and were followed for a mean 12.1 ± 1.5 vs 7.6 ± 2.1 years. Respective mean weight regain from nadir was 15.0 ± 14.4 kg vs 11.9 ± 12.2 kg. Respective percent mean total weight loss and excess weight loss were 20.9 ± 12.7% and 51.8 ± 33.1%, and 18.3 ± 12.8% and 43.4 ± 31.6% at last follow-up, with no significant difference between groups. Resolution of type 2 diabetes (HbA1C < 6.5%, off medications) was 23.1% vs 11.1%; hypertension 36.0% vs 16.0%; and hyperlipidemia 37.1% vs 35.3%. Patients in the pLSG group were significantly more satisfied with LSG (59.8% vs 43.3%, p < 0.05) and more likely to choose the procedure again.
Conclusions
There were no significant differences in long-term weight loss or associated medical condition outcomes in matched pLSG and rLSG patients.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic sleeve gastrectomy (LSG) is a well-accepted metabolic/bariatric (MBS) procedure. It has gained popularity since its introduction by Gagner et al. as a putative first step of the biliopancreatic diversion with duodenal switch (BPD-DS) or Roux-en-Y gastric bypass (RYGB) in 2003 [1]. LSG requires a relatively simple surgical technique, entails minimal alteration of normal anatomy, introduces no foreign body or gastrointestinal anastomoses, and maintains normal gastrointestinal continuity [2, 3]. Drawbacks of LSG are its irreversible nature and the inherent complications associated with its very long staple line [4, 5]. In a position statement summarizing three randomized controlled trials of LSG, the American Society for Metabolic and Bariatric Surgery (ASMBS) observed mid-term total body weight loss of 18.6–28.4% in patients with severe obesity and found weight loss and associated medical problem (AMP) improvement equivalent to that RYGB at 1-year follow-up [6,7,8,9]. Between 2016 and 2020, primary LSG (pLSG) overtook all other MBS operations in global prevalence (50.2%) [10, 11]. However, a shortfall of long-term evidence inhibits evaluation of pLSG as a durably effective MBS procedure.
Adjustable gastric banding (AGB) was introduced in the late 1980s and gained popularity throughout the 1990s as a minimally invasive and reversible operation effective over early and medium terms [12,13,14,15]. As follow-up progressed into the long term, it was found unsuccessful in > 50.0% of cases [16, 17]. Band-related complications including slippage, erosion, esophageal dilation, food intolerance, reflux, and vomiting in up to 60.0% of patients increasingly necessitated revision of the AGB to RYGB or to LSG [18,19,20,21]. Revisional LSG (rLSG) has been found safe in both one- and two-step operative approaches to AGB conversion, with very low 30-day adverse event rates and good medium-term excess weight loss (EWL) between 59.9 and 78.5% [22,23,24,25,26,27].
Analyses of > 5–15-year results of pLSG and rLSG are lacking. Long-term evidence is crucial in the decision-making process of procedure choice for both primary and revisional surgery, especially in the “post-banding era,” with a growing number of patients with ineffective AGB operations [28, 29]. The objective of this matched retrospective cohort study was to compare long-term outcomes of primary vs revisional LSG with respect to weight loss, AMP resolution, and patient satisfaction.
Methods
Study Design
A retrospective, long-term, matched cohort study of patients with obesity who underwent rLSG after an ineffective AGB and a control group of patients who underwent pLSG. All in the rLSG cohort are post-AGB patients and their request was examined and approved by the Exceptions Committee and the Bariatric Committee. The criteria for rLSG surgery are weight regain, leak from the gastric band, disconnection of the gastric band, or lack of adaptation to the gastric band. Data were drawn from a prospectively maintained database of bariatric procedures performed.
All patients met the local and US National Institutes of Health inclusion criteria for MBS [30]. Patients were excluded if they had poorly controlled mental illness, or were pregnant or lactating females at the time of enrollment. Patients were also excluded if they had previously undergone bariatric surgery other than AGB. Specific history of AGB failure was not collected or used as exclusion criteria, e.g., band migration, slippage, or esophageal dilation.
The investigation was authorized by the hospital institutional review board (Approval #2,012,021-ASMC). The standards for patient care described in the 1964 Helsinki Declaration and its amendments were ensured throughout the study [31].
Hospital data included height, weight, body mass index (BMI), and baseline obesity AMP status (e.g., type 2 diabetes mellitus [T2DM], hypertension, and hyperlipidemia). LSG was performed as previously described [20]. Postoperative effectiveness endpoints, including %EWL and percentage of total weight loss (%TWL), were calculated. Percentage EWL was calculated by the formula: ([initial weight − follow-up weight] / [initial weight − ideal body weight]) × 100. TWL was calculated by the formula: ([initial weight − follow-up weight] / [initial weight]) × 100. Weight regain was assessed as the proportion of patients that initially achieved ≥ 50.0% EWL at nadir, but then fell below 50.0% EWL at long-term follow-up. In addition, weight regain was reported as weight gain post nadir (kg) and percentage of maximum weight lost. Resolution of T2DM was defined as HbA1C ≤ 6.5% and a fasting plasma glucose ≤ 100 mg/dL without antidiabetic medication for at least 1 year. Resolution of hypertension was defined as normalization of systolic blood pressure, or diastolic blood pressure without use of antihypertensive medication. Obstructive sleep apnea resolution was defined as an apnea–hypopnea index of < 5 events/hour on polysomnography, symptom relief, and cessation of continuous positive airway pressure use. Gastroesophageal reflux disease (GERD) resolution was defined as symptomatic relief during interruption of treatment with proton-pump inhibitors (PPIs), whereas improvement was defined as lessening or absence of symptoms with a lower PPI dosage. Resolution of hyperlipidemia was defined as fasting lipid profile of HDL > 40 mg for men and > 50 mg for women, and/or TG < 150, and/or LDL < 100 mg/dL without lipid-lowering agents.
During long-term follow-up, patient-reported outcomes were collected through a detailed online questionnaire. This included questions regarding current weight and nadir weight, AMP status, complications (including de novo GERD, infertility, cholelithiasis, and gastrointestinal malignancies), post-LSG hospitalizations, emergency room visits, gastroscopy and non-bariatric procedures, frequency of dietitian follow-up and blood tests, reasons for weight regain, and post-procedure satisfaction. A patient telephone interview followed questionnaire completion as needed, particularly for detailed assessment of AMP resolution criteria.
Statistical Analysis
Analyses were performed using the SPSS Statistics for Windows package, version 26.0 (IBM Corp. Released 2019, Armonk, NY). Data normality was evaluated using the Kolmogorov–Smirnov test; normality assessments were supplemented by visual inspection of histograms and Q-Q plots. Normally distributed continuous variables were reported as mean and standard deviation (SD); otherwise, as median and interquartile range (IQR). Between-group differences were assessed using the dependent samples t-test or the Wilcoxon test for paired samples. Qualitative variables were reported as frequencies and percentages, and evaluated using the McNemar test for correlated proportions. All statistical tests were two-tailed and statistical significance was set at p < 0.05.
Results
Patient Baseline Characteristics
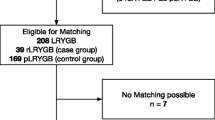
Patient characteristics and operative data from a retrospective examination of a prospectively maintained database containing records of 2289 sleeve gastrectomy patients were reviewed. Questionnaires were distributed to all, and 727 patients responded (611 pLSG, 116 rLSG) (Fig. 1). Following a cross-matching procedure according to baseline BMI, gender, and age, 194 patients with > 5-year follow-up data who had undergone pLSG (n = 97) or rLSG (n = 97) between May 1, 2006, and December 31, 2016, were identified and included in the analysis of long-term outcomes. Of 98 eligible rLSG patients, one male patient was excluded due to an extremely high BMI (67.0 kg/m2) with no appropriate match in the pLSG group.
Patient characteristics from the matched groups are presented in Table 1. Mean baseline BMI and age for both groups were 44.1 kg/m2 and 44.2 years. Each group was comprised of 67.0% females. There were no significant between-group differences in smoking or marital status, with most patients in each group married at the time of LSG (71.1% vs 72.2%, p = 0.160). Primary LSG patients had undergone significantly more laparoscopic cholecystectomies relative to revisional patients (10.3% vs 2.1%, p < 0.05), and 69.1% of revisional patients had a failed band removed during LSG.
Long-Term Weight Loss and Weight Regain
Primary LSG patients had a significantly longer mean follow-up period than rLSG patients (12.1 ± 5.6 vs 7.6 ± 2.1 years; p < 0.001) (Table 2). Both groups reached their nadir weights at an average of 1.3 years post-LSG. Mean baseline BMI of 44.1 kg/m2 was reduced to a nadir BMI of 29.2 ± 5.7 kg/m2 and 31.2 ± 5.6 kg/m2 with corresponding nadir EWL of 79.6% and 67.7% in pLSG and rLSG patients, respectively (p < 0.05 for both). Insufficient weight loss at nadir (e.g., < 50.0% EWL) was observed in 10.3% and 26.8% in pLSG and rLSG patients, respectively (p < 0.005). Long-term follow-up mean BMI was not significantly different between groups (34.5 ± 8.4 kg/m2 vs 35.4 ± 7.2 kg/m2, p = 0.262) despite the longer mean follow-up time in the pLSG group.
Conversely, the vast majority of patients reported weight regain (85.6% and 81.4% of pLSG and rLSG patients, respectively [p = 0.562]). Still, at long-term follow-up, both groups showed significant excess weight loss of 51.8% and 43.4%, respectively. There was a significant trend towards earlier weight regain in revisional patients (3.4 ± 2.2 vs 2.6 ± 1.7 years, in pLSG and rLSG, respectively; p < 0.05). This was accompanied by a slightly higher percentage regain of the maximum weight lost in revisional patients (37.2% vs 40.0%). There was no significant difference in the proportion of patients in each group experiencing weight regain since nadir (Table 2, Fig. 2).
Patient-reported reasons for weight regain are presented in Table 3. Of patients reporting weight regain, approximately half acknowledged that they “did not follow recommended guidelines” (59.8% and 47.4% of pLSG and rLSG, respectively; p = 0.113). Subjective feeling of “sleeve enlargement” was also frequently reported as a reason for weight regain by both groups (43.3% vs 37.1%, respectively; p = 0.464). Significant between-group differences of reported reasons for weight regain were “lack of exercise” (39.2% vs 57.7%, respectively; p < 0.05) and “did not meet with dietitian” (22.7% vs 44.3%, respectively; p < 0.01), with revisional patients reporting significantly greater insufficiencies (Fig. 3). Surprisingly, restrictions associated with the COVID-19 pandemic (e.g., lockdown with more time spent at home, inability to exercise outdoors, and anxiety and mood disturbances) [32, 33] were not considered a factor in weight regain by either group.
Ultimately, 85.6% of pLSG patients reported at least some weight regain from nadir; 59.8% of primary patients were sufficiently satisfied with the procedure and would choose LSG again. Conversely, despite similar levels of weight regain, revisional patients were significantly less satisfied (43.3%; p < 0.05) with LSG.
Post-LSG Hospitalizations, Procedures, and Clinical Follow-Up
Following LSG, approximately 10.0% of patients from both groups visited the emergency room (Table 4); only 12.4% and 9.3% of pLSG and rLSG, respectively, were re-hospitalized (p = 0.645). A total of 50 (51.5%) primary patients and 25 revisional (25.8%) (p < 0.001) had additional non-bariatric intervention at some point during follow-up. A listing of types and frequencies of additional procedures is presented in Table 5; gastroscopic findings are presented in Table 6.
Adherence to dietitian follow-up was similar between groups but extremely rare through last follow-up. Interestingly, 48.5% of primary patients reported that they did not routinely follow-up with a dietitian post-LSG compared with 30.9% of revisional patients (p = 0.052). It is disappointing to report that only 4.1% of primary patients and 5.2% of revisional patients reported routine follow-up with a dietitian. The majority of LSG patients (66.0% primary, 53.6% revisional) attended routine clinical appointments and had blood tests performed (Table 4).
Patient-Reported Post-LSG Change in Obesity-Related Conditions
Rates of “remission,” “improvement,” and “no change” for selected conditions are presented in Table 7. Although 33.0% of all LSG patients included in the current study regained ≥ 50.0% of maximum weight lost by long-term follow-up (Table 2, Fig. 2), both primary and revisional groups maintained AMP resolution/improvement rates ranging from 50.0 to 100.0% (i.e., T2DM, hyperlipidemia, hypertension, obstructive sleep apnea, fatty liver, and GERD), with no significant difference between groups. Although a precise correlation has not been presented, the rates of weight loss and AMP resolution correspond reasonably closely to reported TWL and EWL rates.
Discussion
In our comparative study of pLSG and rLSG, we found that both weight loss and AMP reduction were statistically similar between groups at long-term follow-up. This finding was in agreement with some but not all prior researchers’ outcomes. In the first systematic review comparing outcomes of revisional LSG and RYGB to their primary procedures, Mahawar and co-workers found rLSG to have acceptable safety and significant but somewhat reduced weight loss [34]. Although some observational rLSG studies reported very high rates of weight loss reaching 70.0–75.0% EWL, these findings apply to results in the early and intermediate time frames (≤ 5 years) [35, 36]. To our knowledge, the number of directly comparative studies of pLSG and rLSG in patients with severe obesity with long-term ≥ 5-year follow-up similar to the current study (combined mean 9.8 years) number only three: Carandina et al. (6 years), Kraljevic et al. (7.5 years), and de Angelis et al. (8 years) [37,38,39].
Weight Loss
Regarding long-term weight loss, the current study’s findings for pLSG (51.8% EWL) were relatively similar to those of Carandina et al. (57.2%), who studied a consecutive series of 601 pLSG and 100 rLSG patients with severe obesity after a two-step AGB conversion procedure [37]. However, the current study’s rLSG group EWL was substantially greater than that of Carandina et al.’s (43.4% vs 29.8%). Kraljević et al. studied 262 pLSG patients and 45 rLSG patients with severe obesity who underwent one-step AGB conversion due to band intolerance, slippage, or insufficient weight loss [38]. At mean follow-up time of 7.5 ± 3.4 years, both pLSG and rLSG groups appeared to have lost relatively more weight than in the current study. De Angelis and colleagues compared 56 pLSG and 44 rLSG patients converted from AGB in a two-step process [39]. At 8-year follow-up, as in our own and the other two investigations, weight loss was significantly greater in pLSG than in rLSG patients.
In addition to the three currently available long-term reports of post-LSG weight loss [37,38,39], the current study’s primary group EWL outcomes were > 50.0%, falling within the range of the four study results (51.0 to 67.0%). The current study’s revisional group EWL outcomes also fell within the range of the four studies (29.8 to 53.0% EWL). The majority of our patients in both the primary and revisional groups (> 81.0%) experienced at least some weight regain. A meaningful number of patients with successful weight loss after primary and revisional LSG were not able to maintain > 50.0% weight loss at long-term follow-up (46.0% pLSG, 40.8% rLSG); yet, importantly, very good weight loss results were achieved and maintained at long-term for > 50.0% of patients.
Frustratingly, in findings reported by our patients, approximately half conveyed that they did not follow the recommended weight loss and maintenance behavioral guidelines. The pLSG group reported significantly fewer shortfalls than the rLSG group in adherence to specific behaviors including engaging in regular exercise, and meeting with the dietitian for counsel and support. Despite regaining weight in similar proportions to pLSG patients, the rLSG cohort was significantly less satisfied with the procedure. In general, patients do not expect to regain weight after the LSG procedure; so at times they are not satisfied with the surgery when they realize that the procedure is not a “magic pill” and they are required to adjust to a healthier lifestyle following surgery. After a first procedure, patients who regain weight tend to blame themselves if they did not fully follow recommended guidelines. However, after revisional surgery, patients who regain weight tend to blame the surgery, resulting in even greater disappointment with the surgery compared to that of the primary patient.
An interesting finding was that a noteworthy proportion of patients in both groups (43.3% and 37.1%, respectively) reported the marked subjective sensation of enlargement of their gastric sleeve and associated it with their weight regain. However, medical records demonstrated that only 1/43 pLSG patients who underwent gastroscopy was found to have developed an enlarged sleeve, and 0/35 among rLSG patients. It should be noted that gastroscopy is not an accurate test for evaluating sleeve dilation. A further investigation into patient perceptions in relation to their altered gastric anatomy may be of value to both patients and physicians.
Re-hospitalization and Other Procedures
The rate of re-hospitalization was slightly higher in our pLSG group (12.4%) vs rLSG group (9.3%). Also, more than half of this study’s pLSG patients and one-quarter of rLSG patients underwent additional non-bariatric intervention over the course of long-term follow-up. Additional post-LSG procedures were highly varied in both groups including, predominantly, abdominal wall hernia repair, cholecystectomy, abdominoplasty, and orthopedic procedures; in the rLSG group, gynecologic and cesarean procedures were among the most prevalent.
AMP Improvement
While Carandina et al.’s study suggested that rLSG resulted in somewhat lower AMP remission/improvement than pLSG, our study more closely mirrored the findings of Kraljevic et al. and De Angelis et al. [37,38,39], which reported equally durable weight loss and AMP control between pLSG and rLSG patients. Kraljević et al.’s study showed considerable AMP improvement in pLSG and rLSG patients combined: T2DM 61.0%, hypertension 60.5%, and hyperlipidemia 46.0%, findings comparable to our own study.
With respect to GERD outcomes at long term, De Angelis et al. saw greater prevalence of the disease in rLSG vs pLSG patients (9.0% vs 1.8% mild GERD, and 23.0 vs 3.0% severe GERD) and found that it was the main reason for revision in both groups. In the current study, GERD was significantly more prevalent at baseline in rLSG vs pLSG patients (27.4% vs 6.2%; p < 0.001); yet, our rLSG patients experienced a 70.0% remission/improvement rate vs 50.0% in pLSG patients at long-term follow-up. It is noteworthy that, among patients who underwent upper gastrointestinal endoscopy, no patient in the pLSG group with a mean follow-up of 12.1 years and only one patient in the rLSG group with mean follow-up of 6.7 years developed severe esophagitis. LSG may not be a long-term reflux-prone operation; however, the current study cannot draw this conclusion. Further long-term studies are needed to provide additional evidence of this relationship.
Our rLSG cohort demonstrated acceptable safety, significant sufficient weight loss, and adequate improvement of their AMPs. There were no statistically significant differences between groups in AMP outcomes in our study at the combined mean follow-up of 9.8 years. Two-thirds of all LSG patients in our study maintained > 50.0% of their weight loss at long-term follow-up and maintained 50.0–100.0% remission/improvement of their AMPs.
Limitations and Strengths
This study was somewhat limited by its retrospective design and relatively small sample size. However, the study design with paired matching of pLSG with rLSG patient cohorts may afford more equipoise in comparing outcomes than an unmatched control group. The primary pitfall of the study may be that patient self-reported data (both subjective [patient satisfaction and reasons for revision] and objective [mainly, present weight and comorbidities]) potentially lack rigor, and thus, may result in information bias and significantly reduce the reliability of the findings. We trust that our patients do not report untrue values when specifically asked by their caregivers about their weight, but obviously these numbers cannot be scientifically validated. Though we believe them to be accurate, the reader should consider them with caution. Moreover, since the matching process was conducted only by gender, age, and baseline BMI, it may have resulted in a potential selection bias of the matched cohort, including a significant difference in the follow-up period of the two study groups. Further, it may be interesting to evaluate patient’s quality of life post-LSG and the difference between the groups. Future studies are needed to investigate this outcome by validated questionnaires.
Conclusions
There were no significant differences in weight loss or AMP remission/improvement following rLSG when compared to a matched pLSG cohort. Investigations reporting long-term LSG outcomes remain limited. Additional studies and those with larger samples are needed to assess outcomes of primary and revisional LSG over the long term.
Data Availability
Data available on request due to privacy/ethical restrictions.
References
Regan JP, Inabnet WB, Gagner M, et al. Early experience with two-stage laparoscopic Roux-en-Y gastric bypass as an alternative in the super-super obese patient. Obes Surg. 2003;13(6):861–4.
Aurora AR, Khaitan L, Saber AA. Sleeve gastrectomy and the risk of leak: a systematic analysis of 4,888 patients. Surg Endosc. 2012;26(6):1509–15.
Buchwald H. The evolution of metabolic/bariatric surgery. Obes Surg. 2014;24(8):1126–35.
Gagner M, Buchwald JN. Comparison of laparoscopic sleeve gastrectomy leak rates in four staple-line reinforcement options: a systematic review. Surg Obes Relat Dis. 2014;10(4):713–23.
Sakran N, Goitein D, Raziel A, et al. Gastric leaks after sleeve gastrectomy: a multicenter experience with 2,834 patients. Surg Endosc. 2013;27(1):240–5.
Ali M, El Chaar M, Ghiassi S, et al. American Society for Metabolic and Bariatric Surgery updated position statement on sleeve gastrectomy as a bariatric procedure. Surg Obes Relat Dis. 2017;13(10):1652–7.
Keidar A, Hershkop KJ, Marko L, et al. Roux-en-Y gastric bypass vs sleeve gastrectomy for obese patients with type 2 diabetes: a randomised trial. Diabetologia. 2013;56(9):1914–8.
Peterli R, Borbely Y, Kern B, et al. Early results of the Swiss Multicentre Bypass or Sleeve Study (SM-BOSS): a prospective randomized trial comparing laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass. Annals Surg. 2013;258(5):690–4 (discussion 5).
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med. 2014;370(21):2002–13.
Angrisani L, Santonicola A, Iovino P, Vitiello A, Higa K, Himpens J, Buchwald H, Scopinaro N. IFSO Worldwide Survey 2016: primary, endoluminal, and revisional procedures. Obes Surg. 2018;28(12):3783–3794.
Brown WA, Kow L, Shikora SA, et al. Sixth IFSO globar registry report. Dendrite clinical systems Ltd; 2021 [cited 2022]. Available from: https://www.e-dendrite.com/IFSO6.
Boza C, Gamboa C, Perez G, et al. Laparoscopic adjustable gastric banding (LAGB): surgical results and 5-year follow-up. Surg Endosc. 2011;25(1):292–7.
Chapman AE, Kiroff G, Game P, et al. Laparoscopic adjustable gastric banding in the treatment of obesity: a systematic literature review. Surgery. 2004;135(3):326–51.
Forsell P, Hallberg D, Hellers G. Gastric banding for morbid obesity: initial experience with a new adjustable band. Obes Surg. 1993;3(4):369–74.
Kuzmak LI. A review of seven years’ experience with silicone gastric banding. Obes Surg. 1991;1(4):403–8.
Di Lorenzo N, Antoniou SA, Batterham RL, et al. Clinical practice guidelines of the European Association for Endoscopic Surgery (EAES) on bariatric surgery: update 2020 endorsed by IFSO-EC EASO and ESPCOP. Surg Endosc. 2020;34(6):2332–58.
Tsai C, Zehetner J, Beel J, et al. Long-term outcomes and frequency of reoperative bariatric surgery beyond 15 years after gastric banding: a high band failure rate with safe revisions. Surg Obes Relat Dis. 2019;15(6):900–7.
Berende CA, de Zoete JP, Smulders JF, et al. Laparoscopic sleeve gastrectomy feasible for bariatric revision surgery. Obes Surg. 2012;22(2):330–4.
Foletto M, Prevedello L, Bernante P, et al. Sleeve gastrectomy as revisional procedure for failed gastric banding or gastroplasty. Surg Obes Relat Dis. 2010;6(2):146–51.
Sakran N, Raziel A, Goitein O, et al. Laparoscopic sleeve gastrectomy for morbid obesity in 3003 patients: results at a high-volume bariatric center. Obes Surg. 2016;26(9):2045–50.
Yazbek T, Safa N, Denis R, et al. Laparoscopic sleeve gastrectomy (LSG)—a good bariatric option for failed laparoscopic adjustable gastric banding (LAGB): a review of 90 patients. Obes Surg. 2013;23(3):300–5.
Dang JT, Switzer NJ, Wu J, et al. Gastric band removal in revisional bariatric surgery, one-step versus two-step: a systematic review and meta-analysis. Obes Surg. 2016;26(4):866–73.
Janik M, Ibikunle C, Khan A, et al. Safety of single stage revision laparoscopic sleeve gastrectomy compared to laparoscopic Roux-Y gastric bypass after failed gastric banding. Obes Surg. 2021;31(2):588–96.
Perry Z, Romano-Zelekha O, Sakran N, et al. Laparoscopic sleeve gastrectomy following failed laparoscopic adjustable gastric banding—a comparison between one- and two-stage procedures, an Israeli National Database Study. Obes Surg. 2021;31(6):2364–72.
Silecchia G, Rizzello M, De Angelis F, et al. Laparoscopic sleeve gastrectomy as a revisional procedure for failed laparoscopic gastric banding with a “2-step approach”: a multicenter study. Surg Obes Relat Dis. 2014;10(4):626–31.
Carandina S, Maldonado PS, Tabbara M, et al. Two-step conversion surgery after failed laparoscopic adjustable gastric banding. Comparison between laparoscopic Roux-en-Y gastric bypass and laparoscopic gastric sleeve. Surg Obes Relat Dis. 2014;10(6):1085–91.
Spaniolas K, Bates AT, Docimo S Jr. Single stage conversion from adjustable gastric banding to sleeve gastrectomy or Roux-en-Y gastric bypass: an analysis of 4875 patients. Surg Obes Relat Dis. 2017;13(11):1880–4.
Fiorani C, Coles SR, Kulendran M, et al. Long-term quality of life outcomes after laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass—a comparative study. Obes Surg. 2021;31(3):1376–80.
Akpinar EO, Liem RSL, Nienhuijs SW. Metabolic effects of bariatric surgery on patients with type 2 diabetes: a population-based study. Surg Obes Relat Dis. 2021;17(7):1349–58.
NIH conference. Gastrointestinal surgery for severe obesity. Consensus Development Conference Panel. Ann Intern Med. 1991;115(12):956–61.
World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–4.
Bellicha A, Lassen PB, Poitou C, Genser L, Marchelli F, Aron-Wisnewsky J, Ciangura C, Jacques F, Moreau P; NutriOmics Investigators, Clément K, Oppert JM. Effect of COVID-19 lockdowns on physical activity, eating behavior, body weight and psychological outcomes in a Post-Bariatric Cohort. Obes Surg. 2022;32(7):1–9.
Andreu A, Flores L, Molero J, et al. Patients undergoing bariatric surgery: a special risk group for lifestyle, emotional and behavioral adaptations during the COVID-19 lockdown. Lessons from the first wave. Obes Surg. 2022;32(2):441–9.
Mahawar KK, Graham Y, Carr WR, et al. Revisional Roux-en-Y gastric bypass and sleeve gastrectomy: a systematic review of comparative outcomes with respective primary procedures. Obes Surg. 2015;25(7):1271–80.
Alqahtani AR, Elahmedi MO, Al Qahtani AR, et al. 5-Year outcomes of 1-stage gastric band removal and sleeve gastrectomy. Surg Obes Relat Dis. 2016;12(10):1769–76.
Noel P, Schneck AS, Nedelcu M, et al. Laparoscopic sleeve gastrectomy as a revisional procedure for failed gastric banding: lessons from 300 consecutive cases. Surg Obes Relat Dis. 2014;10(6):1116–22.
Carandina S, Genser L, Bossi M, et al. Laparoscopic sleeve gastrectomy after failed gastric banding: is it really effective? Six years of follow-up. Surg Obes Relat Dis. 2017;13(7):1165–73.
Kraljevic M, Cordasco V, Schneider R, et al. Long-term effects of laparoscopic sleeve gastrectomy: what are the results beyond 10 years? Obes Surg. 2021;31(8):3427–33.
de Angelis F, Boru CE, Iossa A, et al. Long-term outcomes of sleeve gastrectomy as a revisional procedure after failed gastric band: a multicenter cross-matched cohort study. Updates Surg. 2022;74(2):709–13.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Standards/Human and Animal Rights
The study was performed in accord with the ethical standards of the Declaration of Helsinki.
Informed Consent
Informed consent was obtained from all participants.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sakran, N., Soued, S., Hod, K. et al. Long-Term Matched Comparison of Primary and Revisional Laparoscopic Sleeve Gastrectomy. OBES SURG 33, 695–705 (2023). https://doi.org/10.1007/s11695-022-06436-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06436-8