Abstract
Background
Laparoscopic sleeve gastrectomy (LSG) has been validated as a safe and effective treatment for morbid obesity. However, data of the long-term outcome remains lacking.
Methods
A total of 1759 LSG was performed as primary bariatric procedure from 2005 to 2017 with mean age of 35.2 ± 10.3 years old (14–71), female 69.7%, mean body mass index (BMI) 37.9 ± 7.7 kg/m2, and mean waist width 113.7 ± 17.9 cm. All patients were evaluated and managed under a strict multidisciplinary team approach. A retrospective analysis of a prospective bariatric database and telephone interview of patients who defaulted clinic follow-up at 10 years was conducted.
Results
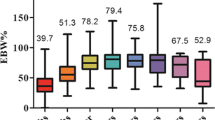
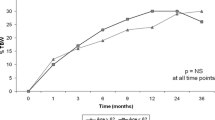
The mean operating time, intraoperative blood, and hospital stay of LSG were 121.5 ± 36.5 min, 40.8 ± 69.7 ml, and 2.8 ± 2.7 days, respectively. The 30-day postoperative major complication occurred in 25 (1.4%) patients. The major complication rate was 15% at first year and 0% at the last year. The follow-up rate at 1, 5 and 10 years were 89.3%, 52.1 and 64.4%. At postoperative 1, 5, and 10 years, the mean percentage of total weight loss (%TWL) and excess weight loss (EWL%) of LSG patients were 33.4, 28.3, and 26.6% and 92.2, 80.1, and 70.5%, respectively. The mean BMI became 27, 26.2, and 27.1 kg/m2 at postoperative 1, 5, and 10 years. At follow-up, a total 69 patients needed surgical revision due to reflux disease (n = 45), weight regain (n = 19), persistent diabetes (n = 2), and chronic fistula (n = 3). The type of revision procedures were hiatal repair and gastropexy (n = 29), Roux-en Y gastric bypass (RYGB) (n = 23), and single anastomosis bypass (n = 17) with median time to revision 33 months (range 3–62). At 10 years, the overall revision rate was 21.5% (14/65) and 11(16.9%) of 65 patients were converted to RYGB. The other 54 patients remained at LSG anatomy, but 45% of them required proton pump inhibitor for reflux symptoms.
Conclusions
Our results showed that primary LSG is a durable primary bariatric procedure with sustained weight loss and a high resolution of comorbidities at 10 years, but about half the patients had de novo GERD. The need for conversion to RYGB was 16.9% at 10 years.


Similar content being viewed by others
References
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery worldwide 2013. Obes Surg. 2015;25:1822–32.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery and endoliminal procedure: IFSO worldwide survey 2014. Obes Surg. 2017;27:2279–89.
Schouten R, Wiryasaputra DC, van Dielen FMH, et al. Long-term results of bariatric restrictive procedures: a prospective study. Obes Surg. 2010;20(12):1617–26.
Marsk R, Jonas E, Gartzios H, et al. High revision rates after laparoscopic vertical banded gastroplasty. Surg Obes Relat Dis. 2009;5(1):94–8.
Lin YH, Lee WJ, Ser KH, et al. 15-year follow-up of vertical banded gastroplasty: comparison with other restrictive procedures. Surg Endosc. 2016;30:489–92.
Van Nieuwenhove Y, Ceelen W, Stockman A, et al. Long-term results of a prospective study on laparoscopic adjustable gastric banding for morbid obesity. ObesSurg. 2011;21(5):582–7.
Chansaenroj P, Aung L, Lee WJ, et al. Revision procedures after failed adjustable gastric banding: comparison of efficacy and safety. Obes Surg. 2017;27:2861–7.
Himpens J, Dobbeleir J, Peeters G. Long-term results of laparoscopic sleeve gastrectomy for obesity. Ann Surg. 2010;252:319–24.
Felsenreich D, Langer FB, Kefurt R, et al. Weight loss, weight regain, and conversions to Roux-en-Y gastric bypass: 10-year results of laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2016;12(9):1655–62.
Arman GA, Himpens J, Dhaenens J, et al. Long-term (11+ years) outcomes in weight, patient satisfaction, comorbidities, and gastroesophageal reflux treatment after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2016;12(10):1778–86.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Ser KH, Lee WJ, Lee YC, et al. Experience in laparoscopic sleeve gastrectomy for morbidly obese Taiwanese: staple-line reinforcement is important for preventing leakage. Surg Endosc. 2010;24(9):2253–9.
Pok EH, Lee WJ, Ser KH, et al. Laparoscopic sleeve gastrectomy in Asia: long term outcome and revisional surgery. Asian J Surg 2016;39:21–8.
Chou JJ, Lee WJ, Almaki O, et al. Dietary intake and weight changes 5 years after laparoscopic sleeve gastrectomy. Obes Surg. 2017;27(12):3240–6.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes—5-year outcomes. N Engl J Med. 2017;376(7):641–51.
Lee WJ, Chong K, Ser KH, et al. Gastric bypass vs sleeve gastrectomy for type 2 diabetes mellitus: a randomized controlled trial. Arch Surg. 2011;146(2):143–8.
Lee WJ, Chong K, Lin YH. Laparoscopic sleeve gastrectomy versus single anastomosis (mini-) gastric bypass for the treatment of type 2 diabetes mellitus: 5-year results of a randomized trial and study of incretin effect. Obes Surg. 2014;24:1552–62.
Thaler JP, Cummings DE. Minireview: Hormononal and metabolic mechanisms of diabetes remission after gastrointestinal surgery. Endocrinology. 2009;150(6):2518–25.
Koner J, Inabnet W, Febres G, et al. Prospective study of gut hormone and metabolic changes after adjustable gastric banding and Roux-en-Y gastric bypass. Int J Obes. 2009;33:786–93.
Lee WJ, Chen CY, Chong K, et al. Changes in postprandial gut hormones after metabolic surgery: a comparison of gastric bypass and sleeve gastrectomy. Surg Obes Relat Dis. 2011;7:683–90.
Lee WJ, Ser KH, Chong K, et al. Laparoscopic sleeve gastrectomy for diabetes treatment in nonmorbidly obese patients: efficacy and change of insulin secretion. Surgery. 2010;147(5):664–9.
Lee WJ, Almulaifi A, Tsou JJ, et al. Laparoscopic sleeve gastrectomy for type 2 diabetes mellitus: predicting the success by ABCD score. Surg Obes Relat Dis. 2015;11:991–7.
Tolone S, Cristiano S, Savarino E, et al. Effects of omega-loop bypass on esophagogastric junction. Surg Obes Relat Dis. 2016;12(1):62–9.
Chuffart E, Sodji M, Dalmay F, et al. Long-term results after sleeve gastrectomy for gastroesophageal disease. Obes Surg. 2017;27(11):2890–7.
Felsenreich DM, Kefurt R, Schermann M, et al. Reflux, sleeve dilatation, and Barrett’s esophagus after laparoscopic sleeve gastrectomy: long-term follow-up. Obes Surg. 2017;27:3092–101.
Genco A, Soricelli E, Casella G, et al. Gastroesophageal reflux disease and Barrett’s esophagus after laparoscopic sleeve gastrectomy: a possible, underestimated longterm complication. Surg Obes Relat Dis. 2017;13(4):568–74.
Hawasli A, Bush A, Hare B, et al. Laparoscopic management of severe reflux after sleeve gastrectomy, in selected patients, without conversion to Roux-en-Y gastric bypass. J Laparoendosc Adv Surg Tech A. 2015;25:631–5.
Desart K, Rossidis G, Michel M, et al. Gastroesophageal reflux management with the LINX® system for gastroesophageal reflux disease following laparoscopic sleeve gastrectomy. J Gastrointest Surg. 2015;19:1782–6.
Gálvez-Valdovinos R, Cruz-Vigo JL, Marín-Santillán E, et al. Cardiopexy with ligamentum teres in patients with hiatal hernia and previous sleeve gastrectomy: an alternative treatment for gastroesophageal reflux disease. Obes Surg. 2015;25:1539–43.
Sanchez-Pernaute A, Talavera P, Perez-Aguirre E, et al. Technique of Hill’s gastropexy combined with sleeve gastrectomy for patients with morbid obesity and gastroesophageal reflux disease or hiatal hernia. Obes Surg. 2016;26:910–2.
Macedo FIB, Mowzoon M, Mittal VK, et al. Outcomes of laparoscopic hiatal hernia repair in nine bariatric patients with prior sleeve gastrectomy. Obes Surg. 2017;27:2768–72.
Acknowledgments
The authors would like to thank the entire staff of the Bariatric Surgery Center, Ming-Shen Hospital, Taiwan, for their help in obtaining the necessary information required for this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
This article does not contain any studies with human participants or animal performed by any of the authors. For this type of study, formal consent is not required. Informed consent does not apply to the submission.
Rights and permissions
About this article
Cite this article
Chang, DM., Lee, WJ., Chen, JC. et al. Thirteen-Year Experience of Laparoscopic Sleeve Gastrectomy: Surgical Risk, Weight Loss, and Revision Procedures. OBES SURG 28, 2991–2997 (2018). https://doi.org/10.1007/s11695-018-3344-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3344-3