Abstract
Introduction
Endoscopic bariatric therapies (EBT) have emerged as effective options for weight loss. While the benefits of EBT have been documented, data regarding such therapies among minority populations remains scant. We aim to investigate EBT trends and outcomes in minority populations.
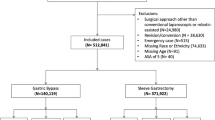
Methods
Data were extracted from the 2015 to 2019 Metabolic and Bariatric Surgery Accreditation and Quality Improvement Project (MBSAQIP) databases. Intragastric balloon (IGB) and endoscopic sleeve gastroplasty (ESG) cases were identified, and procedure volume assessed by year and race/ethnicity. Measures of interest included year-to-year mortality, surgical complications, and 30-day adverse outcomes.
Results
Of 966,646 cases in the MBSAQIP databases, 5209 (0.54%) IGB and ESG cases were included. 10.7% were black, and 81.6% were female patients. Compared to white patients, black and Hispanic patients were younger (p < 0.01) with a higher body mass index (p < 0.001). Mortality (0.03% vs. 0% vs. 0%, p = 0.99), reoperation (1.1% vs. 0.8% vs. 0.6%, p = 0.30), and reintervention (3.9% vs. 3.2% vs. 2.3%, p = 0.09) rates were similar between racial/ethnic cohorts. All complications were similar between racial/ethnic cohorts, except a higher rate of venous thromboembolism, in Hispanic (1.04%, p < 0.01) compared to black (0.18%) and white (0.21%) patients. IGB and ESG were predominantly performed in white and Hispanic patients, respectively. ESG was associated with a higher leak (0.6% vs. 0.02%, p < 0.01) and venous thromboembolism (VTE) (1.0% vs. 0.12%, p < 0.01) rate.
Conclusion
While EBTs have increased annually, they are performed less in black patients. Future studies are needed to identify access barriers for black patients. They are safely performed with similar outcomes in racial/ethnic cohorts, except for a higher VTE rate in Hispanic patients.
Graphical Abstract




Similar content being viewed by others
References
Afshin A, Forouzanfar MH, Reitsma MB, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377(1):13–27.
Gadde KM, Martin CK, Berthoud HR, et al. Obesity: pathophysiology and management. J Am Coll Cardiol. 2018;71(1):69–84.
Wardle J, Carnell S, Haworth CM, et al. Evidence for a strong genetic influence on childhood adiposity despite the force of the obesogenic environment. Am J Clin Nutr. 2008;87(2):398–404.
Locke AE, Kahali B, Berndt SI, et al. Genetic studies of body mass index yield new insights for obesity biology. Nature. 2015;518(7538):197–206.
Silventoinen K, Konttinen H. Obesity and eating behavior from the perspective of twin and genetic research. Neurosci Biobehav Rev. 2020;109:150–65.
WHO. Obesity 2022 [Available from: https://www.who.int/health-topics/obesity#tab=tab_1.
Meldrum DR, Morris MA, Gambone JC. Obesity pandemic: causes, consequences, and solutions-but do we have the will? Fertil Steril. 2017;107(4):833–9.
Buffington CK, Marema RT. Ethnic differences in obesity and surgical weight loss between African-American and Caucasian females. Obes Surg. 2006;16(2):159–65.
Bray GA, Frühbeck G, Ryan DH, et al. Management of obesity. Lancet. 2016;387(10031):1947–56.
Brethauer SA, Hammel JP, Schauer PR. Systematic review of sleeve gastrectomy as staging and primary bariatric procedure. Surg Obes Relat Dis. 2009;5(4):469–75.
Buchwald H, Estok R, Fahrbach K, et al. Trends in mortality in bariatric surgery: a systematic review and meta-analysis. Surgery. 2007;142(4):621–32; discussion 32–5.
Morino M, Toppino M, Forestieri P, et al. Mortality after bariatric surgery: analysis of 13,871 morbidly obese patients from a national registry. Ann Surg. 2007;246(6):1002–7; discussion 7–9.
Flum DR, Belle SH, King WC, et al. Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med. 2009;361(5):445–54.
Hedjoudje A, Abu Dayyeh BK, Cheskin LJ, et al. Efficacy and safety of endoscopic sleeve gastroplasty: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2020;18(5):1043-53.e4.
Thompson CC, Abu Dayyeh BK, Kushner R, et al. Percutaneous gastrostomy device for the treatment of class II and class III obesity: results of a randomized controlled trial. Am J Gastroenterol. 2017;112(3):447–57.
Garrido MMKA, Paris J, et al. Methods for constructing and assessing propensity scores. Health Serv Res. 2014;49(5):1701–20.
Reeve BB, Smith AW, Arora NK, Hays RD. Reducing bias in cancer research: application of propensity score matching. Health Care Financ Rev. 2008;29(4):69–80.
Garrido MM, Kelley AS, Paris J, et al. Methods for constructing and assessing propensity scores. Health Serv Res. 2014;49(5):1701–20.
Sullivan S, Edmundowicz SA, Thompson CC. Endoscopic bariatric and metabolic therapies: new and emerging technologies. Gastroenterology. 2017;152(7):1791–801.
Wing RR, Hill JO. Successful weight loss maintenance. Annu Rev Nutr. 2001;21:323–41.
Marrero Torres RJ, Gregory F, Micames CG. Fluid-filled intragastric balloons are an effective and safe weight loss option across BMI and age ranges. Surg Endosc. 2021;36(7):5160–6.
Vilar-Gomez E, Martinez-Perez Y, Calzadilla-Bertot L, et al. Weight loss through lifestyle modification significantly reduces features of nonalcoholic steatohepatitis. Gastroenterology. 2015;149(2):367–78.e5; quiz e14–5.
Administration FaD. FDA Approval for IGB [Available from: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpma/pma.cfm?id=p140008.
Kim SH, Chun HJ, Choi HS, et al. Current status of intragastric balloon for obesity treatment. World J Gastroenterol. 2016;22(24):5495–504.
Abu Dayyeh BK, Rajan E, Gostout CJ. Endoscopic sleeve gastroplasty: a potential endoscopic alternative to surgical sleeve gastrectomy for treatment of obesity. Gastrointest Endosc. 2013;78(3):530–5.
Matteo MV, D’Oria M, Bove V, et al. Personalized approach for obese patients undergoing endoscopic sleeve gastroplasty. J Pers Med. 2021;11(12):1–14.
Ginsberg GG, Chand B, Cote GA, et al. A pathway to endoscopic bariatric therapies. Gastrointest Endosc. 2011;74(5):943–53.
Ryou M, McQuaid KR, Thompson CC, et al. ASGE EndoVators Summit: defining the role and value of endoscopic therapies in obesity management. Surg Endosc. 2018;32(1):1–13.
Sheka AC, Kizy S, Wirth K, et al. Racial disparities in perioperative outcomes after bariatric surgery. Surg Obes Relat Dis. 2019;15(5):786–93.
Nguyen GC, Patel AM. Racial disparities in mortality in patients undergoing bariatric surgery in the U.S.A. Obes Surg. 2013;23(10):1508–14.
Amirian H, Torquati A, Omotosho P. Racial disparity in 30-day outcomes of metabolic and bariatric surgery. Obes Surg. 2020;30(3):1011–20.
Edwards MA, Bruff A, Mazzei M, et al. Racial disparities in perioperative outcomes after metabolic and bariatric surgery: a case-control matched study. Surg Obes Relat Dis. 2020;16(8):1111–23.
Edwards MA, Agarwal S, Mazzei M. Racial disparities in bariatric perioperative outcomes among the elderly. Surg Obes Relat Dis. 2022;18(1):62–70.
Agarwal S, Bruff A, Mazzei M, et al. Exploring racial disparity in perioperative outcomes following revisional bariatric surgery: a case-control matched analysis. Am J Surg. 2021;221(4):741–8.
Acevedo E Jr, Lu X, Zhao H, et al. Outcomes in racial minorities after robotic Roux-en-Y gastric bypass and sleeve gastrectomy: a retrospective review of the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database. Surg Obes Relat Dis. 2021;17(3):595–605.
Balduf LM, Farrell TM. Attitudes, beliefs, and referral patterns of PCPs to bariatric surgeons. J Surg Res. 2008;144(1):49–58.
Ames GE, Maynard JR, Collazo-Clavell ML, et al. Rethinking patient and medical professional perspectives on bariatric surgery as a medically necessary treatment. Mayo Clin Proc. 2020;95(3):527–40.
Wee CC, Huskey KW, Bolcic-Jankovic D, et al. Sex, race, and consideration of bariatric surgery among primary care patients with moderate to severe obesity. J Gen Intern Med. 2014;29(1):68–75.
Edwards MA, Muraleedharan D, Spaulding A. Racial disparities in reasons for mortality following bariatric surgery. J Racial Ethn Health Disparities. 2022. https://doi.org/10.1007/s40615-022-01242-5.
Mital S, Nguyen HV. Cost-effectiveness of procedure-less intragastric balloon therapy as substitute or complement to bariatric surgery. PLoS ONE. 2021;16(7):e0254063.
Melissas J, Mouzas J, Filis D, et al. The intragastric balloon - smoothing the path to bariatric surgery. Obes Surg. 2006;16(7):897–902.
Liu N, Funk LM. Bariatric surgery trends in the U.S.: 1% is the loneliest number. Ann Surg. 2020;271(2):210–1.
Ribeiro da Silva J, Proença L, Rodrigues A, et al. Intragastric balloon for obesity treatment: safety, tolerance, and efficacy. GE Port J Gastroenterol. 2018;25(5):236–42.
Lopez-Nava G, Sharaiha RZ, Vargas EJ, et al. Endoscopic sleeve gastroplasty for obesity: a multicenter study of 248 patients with 24 months follow-up. Obes Surg. 2017;27(10):2649–55.
Stavrou G, Tsaousi G, Kotzampassi K. Life-threatening visceral complications after intragastric balloon insertion: is the device, the patient or the doctor to blame? Endosc Int Open. 2019;7(2):E122–9.
Sartoretto A, Sui Z, Hill C, et al. Endoscopic sleeve gastroplasty (ESG) is a reproducible and effective endoscopic bariatric therapy suitable for widespread clinical adoption: a large, international multicenter study. Obes Surg. 2018;28(7):1812–21.
Abu Dayyeh BK, Bazerbachi F, Vargas EJ, et al. Endoscopic sleeve gastroplasty for treatment of class 1 and 2 obesity (MERIT): a prospective, multicentre, randomised trial. Lancet. 2022;400(10350):441–51.
Ouni A, Khosla AA, Gómez V. Perception of bariatric surgery and endoscopic bariatric therapies among primary care physicians. Obes Surg. 2022;32(10):3384–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
For this type of study, formal consent is not required.
Informed Consent
Informed consent does not apply.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Endoscopic bariatric therapies have increased annually.
• Endoscopic bariatric therapies are performed with low mortality and morbidity.
• Endoscopic bariatric therapies are performed less in minority patients, representing an access gap.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ouni, A., Spaulding, A., Khosla, A.A. et al. Outcomes and Trends of Endoscopic Bariatric Therapies (EBT) Among Minority Populations. OBES SURG 33, 513–522 (2023). https://doi.org/10.1007/s11695-022-06399-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06399-w