Abstract
Purpose
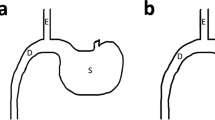
Roux-en-Y gastric bypass (RYGB) has superior long-term diabetes remission outcomes to sleeve gastrectomy (SG). However, in regions with a high prevalence of gastric cancer, RYGB may not be the best option. This study aimed to investigate the anti-diabetic effect of SG with transit bipartition (SG-TB) compared with SG and RYGB.
Materials and Methods
A total of 32 diabetic Sprague-Dawley rat models were assigned to one of four groups: SG (n = 8), RYGB (n = 8), SG-TB (n = 8), and SHAM (n = 8). Body weight, food intake, blood glucose, and hormonal changes (glucagon-like peptide-1 (GLP-1), insulin, and glucagon) were measured to investigate the effect of surgery in all groups. Oral glucose tolerance test and insulin tolerance test were performed before and 8 weeks after surgery.
Results
There were no significant differences in the postoperative changes in body weight and food intake among the SG, RYGB, and SG-TB groups. Postoperatively, the RYGB and SG-TB groups had significantly higher GLP-1 levels and lower insulin levels than the SG group. Further, RYGB and SG-TB had significantly better glucose control improvements than SG. There were no significant differences in GLP-1, insulin, glucagon, and homeostasis model assessment of insulin resistance levels between RYGB and SG-TB. The preoperative and postoperative values of all variables in the SHAM group did not show significant differences.
Conclusion
In this study using a diabetes-induced rodent model, we found that the anti-diabetic effect of SG-TB is superior to that of SG and non-inferior to that of RYGB.




Similar content being viewed by others
References
Wu J, Xu H, He X, et al. Six-year changes in the prevalence of obesity and obesity-related diseases in Northeastern China from 2007 to 2013. Sci Rep. 2017;7:41518.
Zhang L, Wang Z, Wang X, et al. Prevalence of abdominal obesity in China: results from a cross-sectional study of nearly half a million participants. Obesity (Silver Spring). 2019;27(11):1898–905.
Ma RCW. Epidemiology of diabetes and diabetic complications in China. Diabetologia. 2018;61(6):1249–60.
Du X, Dai R, Zhou HX, et al. Bariatric surgery in china: how is this new concept going? Obes Surg. 2016;26(12):2906–12.
Welbourn R, Hollyman M, Kinsman R, et al. Bariatric surgery worldwide: baseline demographic description and one-year outcomes from the Fourth IFSO Global Registry Report 2018. Obes Surg. 2019;29(3):782–95.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes - 5-year outcomes. N Engl J Med. 2017;376(7):641–51.
Salminen P, Helmiö M, Ovaska J, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss at 5 years among patients with morbid obesity: the SLEEVEPASS randomized clinical trial. JAMA. 2018;319(3):241–54.
Peterli R, Wölnerhanssen BK, Peters T, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity: the SM-BOSS randomized clinical trial. JAMA. 2018;319(3):255–65.
Shoar S, Saber AA. Long-term and midterm outcomes of laparoscopic sleeve gastrectomy versus Roux-en-Y gastric bypass: a systematic review and meta-analysis of comparative studies. Surg Obes Relat Dis. 2017;13(2):170–80.
Golzarand M, Toolabi K, Farid R. The bariatric surgery and weight losing: a meta-analysis in the long- and very long-term effects of laparoscopic adjustable gastric banding, laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy on weight loss in adults. Surg Endosc. 2017;31(11):4331–45.
Yang P, Chen B, Xiang S, et al. Long-term outcomes of laparoscopic sleeve gastrectomy versus Roux-en-Y gastric bypass for morbid obesity: results from a meta-analysis of randomized controlled trials. Surg Obes Relat Dis. 2019;15(4):546–55.
Balakrishnan M, George R, Sharma A, et al. Changing trends in stomach cancer throughout the world. Curr Gastroenterol Rep. 2017;19(8):36.
Lyons K, Le LC, Pham YT, et al. Gastric cancer: epidemiology, biology, and prevention: a mini review. Eur J Cancer Prev. 2019;28(5):397–412.
Santoro S, Castro LC, Velhote MC, et al. Sleeve gastrectomy with transit bipartition: a potent intervention for metabolic syndrome and obesity. Ann Surg. 2012;256(1):104–10.
Yormaz S, Yılmaz H, Ece I, et al. Laparoscopic ileal interposition with diverted sleeve gastrectomy versus laparoscopic transit bipartition with sleeve gastrectomy for better glycemic outcomes in T2DM patients. Obes Surg. 2018;28(1):77–86.
Azevedo FR, Santoro S, Correa-Giannella ML, et al. A prospective randomized controlled trial of the metabolic effects of sleeve gastrectomy with transit bipartition. Obes Surg. 2018;28(10):3012–9.
Bilecik T. Metabolic effects of sleeve gastrectomy with transit bipartition in obese females with type 2 diabetes mellitus: results after 1-year follow-up. Obes Surg. 2019;29(3):805–10.
Topart P, Becouarn G, Finel JB. Is transit bipartition a better alternative to biliopancreatic diversion with duodenal switch for superobesity? Comparison of the early results of both procedures. Surg Obes Relat Dis. 2020;16(4):497–502.
Karaca FC. Effects of sleeve gastrectomy with transit bipartition on glycemic variables, lipid profile, liver enzymes, and nutritional status in type 2 diabetes mellitus patients. Obes Surg. 2020;30(4):1437–45.
Topart P, Becouarn G, Finel JB. Comparison of 2-year results of Roux-en-Y gastric bypass and transit bipartition with sleeve gastrectomy for superobesity. Obes Surg. 2020;30(9):3402–7.
Widjaja J, Dolo PR, Zhang Q, et al. Bypassed and preserved stomach resulted in superior glucose control in Sprague-Dawley rats with streptozotocin-induced diabetes. Sci Rep. 2019;9(1):9981.
Dolo PR, Yao L, Li C, et al. Preserving duodenal-jejunal (foregut) transit does not impair glucose tolerance and diabetes remission following gastric bypass in type 2 diabetes Sprague-Dawley rat model. Obes Surg. 2018;28(5):1313–20.
Meier JJ. GLP-1 receptor agonists for individualized treatment of type 2 diabetes mellitus. Nat Rev Endocrinol. 2012;8(12):728–42.
Hutch CR, Sandoval D. The role of GLP-1 in the metabolic success of bariatric surgery. Endocrinology. 2017;158(12):4139–51.
Smith EP, Polanco G, Yaqub A, et al. Altered glucose metabolism after bariatric surgery: what’s GLP-1 got to do with it? Metabolism. 2018;83:159–66.
Egerod KL, Engelstoft MS, Grunddal KV, et al. A major lineage of enteroendocrine cells coexpress CCK, secretin, GIP, GLP-1, PYY, and neurotensin but not somatostatin. Endocrinology. 2012;153(12):5782–95.
Chambers AP, Jessen L, Ryan KK, et al. Weight-independent changes in blood glucose homeostasis after gastric bypass or vertical sleeve gastrectomy in rats. Gastroenterology. 2011;141(3):950–8.
Nosso G, Griffo E, Cotugno M, et al. Comparative effects of Roux-en-Y gastric bypass and sleeve gastrectomy on glucose homeostasis and incretin hormones in obese type 2 diabetic patients: a one-year prospective study. Horm Metab Res. 2016;48(5):312–7.
Castagneto Gissey L, Casella Mariolo J, Mingrone G. Intestinal peptide changes after bariatric and minimally invasive surgery: relation to diabetes remission. Peptides. 2018 Feb;100:114–22.
Melissas J, Koukouraki S, Askoxylakis J, et al. Sleeve gastrectomy: a restrictive procedure? Obes Surg. 2007;17(1):57–62.
Yin DP, Gao Q, Ma LL, et al. Assessment of different bariatric surgeries in the treatment of obesity and insulin resistance in mice. Ann Surg. 2011;254(1):73–82.
Mingrone G, Cummings DE. Changes of insulin sensitivity and secretion after bariatric/metabolic surgery. Surg Obes Relat Dis. 2016;12(6):1199–205.
Vrbikova J, Kunesova M, Kyrou I, et al. Insulin sensitivity and secretion in obese type 2 diabetic women after various bariatric operations. Obes Facts. 2016;9(6):410–23.
Shi X, Chacko S, Li F, et al. Acute activation of GLP-1-expressing neurons promotes glucose homeostasis and insulin sensitivity. Mol Metab. 2017;6(11):1350–9.
Rebelos E, Astiarraga B, Bizzotto R, et al. GLP-1 response to sequential mixed meals: influence of insulin resistance. Clin Sci (Lond). 2017;131(24):2901–10.
Yaribeygi H, Sathyapalan T, Sahebkar A. Molecular mechanisms by which GLP-1 RA and DPP-4i induce insulin sensitivity. Life Sci. 2019;234:116776.
Dimitriadis GK, Randeva MS, Miras AD. Potential hormone mechanisms of bariatric surgery. Curr Obes Rep. 2017;6(3):253–65.
Kulina GR, Rayfield EJ. The role of glucagon in the pathophysiology and management of diabetes. Endocr Pract. 2016;22(5):612–21.
Lee YH, Wang MY, Yu XX, et al. Glucagon is the key factor in the development of diabetes. Diabetologia. 2016;59(7):1372–5.
Hædersdal S, Lund A, Knop FK, et al. The role of glucagon in the pathophysiology and treatment of type 2 diabetes. Mayo Clin Proc. 2018;93(2):217–39.
Duca FA, Côté CD, Rasmussen BA, et al. Metformin activates a duodenal Ampk-dependent pathway to lower hepatic glucose production in rats. Nat Med. 2015;21(5):506–11.
Murphy R, Clarke MG, Evennett NJ, et al. Laparoscopic sleeve gastrectomy versus banded Roux-en-Y gastric bypass for diabetes and obesity: a prospective randomized double-blind trial. Obes Surg. 2018;28(2):293–302.
Widjaja J, Pan H, Dolo PR, et al. Short-term diabetes remission outcomes in patients with BMI ≤ 30 kg/m2 following sleeve gastrectomy. Obes Surg. 2020;30(1):18–22.
Aminian A, Brethauer SA, Andalib A, et al. Can sleeve gastrectomy “cure” diabetes? Long-term metabolic effects of sleeve gastrectomy in patients with type 2 diabetes. Ann Surg. 2016;264(4):674–81.
Lee MH, Almalki OM, Lee WJ, et al. Laparoscopic sleeve gastrectomy for type 2 diabetes mellitus: long-term result and recurrence of diabetes. Obes Surg. 2020;30(10):3669–74.
Lee WJ, Almuhanna M. Paired editorial: effects of sleeve gastrectomy with transit bipartition on glycemic variables, lipid profile, liver enzymes and nutritional status in type 2 diabetes mellitus patients: a 1-year follow-up study. Obes Surg. 2020;30(3):1128–9.
Funding
This study was supported by the Science and Technology Program Project of Xuzhou (KC19157).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Statement of Animal Right
All applicable institutional and national guidelines of the People’s Republic of China for the care and use of animals were followed.
Statement of Informed Consent
Informed consent does not apply.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, P., Widjaja, J., Dolo, P.R. et al. Comparing the Anti-diabetic Effect of Sleeve Gastrectomy with Transit Bipartition Against Sleeve Gastrectomy and Roux-en-Y Gastric Bypass Using a Diabetic Rodent Model. OBES SURG 31, 2203–2210 (2021). https://doi.org/10.1007/s11695-021-05256-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05256-6