Abstract
Background
Approximately 14% of Austria’s 8.5 million inhabitants have a body mass index (BMI) > 30 kg/m2. The laparoscopic adjustable gastric banding (LAGB) was introduced in Austria in 1994, where about 10.300 patients have received it so far. One of our LAGB patients developed an adenocarcinoma of the distal esophagus 13 years after implantation.
Objectives
In order to calculate whether after LAGB patients are at higher risk for carcinoma of the esophagus, we performed a nationwide survey.
Methods
A questionnaire was sent to all surgical departments in Austria, primarily in order to detect cases with esophageal carcinoma after LAGB, but also to evaluate the policy in Austria concerning preoperative work-up, operation, and follow-up in LAGB patients.
Results
Since 1994, 37 of the 119 surgical departments in Austria have performed a total of about 10.300 LAGB implantations. Six patients have been identified with esophageal cancer following LAGB. The WHO statistical report on esophageal cancer shows an incidence of 2.8/100.000 per year in Austria, about 1/3 of which cases are adenocarcinoma of the distal esophagus.
Conclusion
Following LAGB, the incidence of esophageal cancer might be up to fivefold higher than the aged standardized overall population of Austria.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The development of malignant tumors of the esophagus and stomach following laparoscopic gastric banding is a rare event. Until today, fewer than 15 cases have been published [1,2,3,4,5,6]. Our deep understanding of the pathophysiology of gastroesophageal reflux disease (GERD) and the pathophysiology of esophageal cancer alerted us when we operated a patient who developed Barrett’s cancer years after laparoscopic adjustable gastric banding (LAGB) [7,8,9,10].
GERD is the most common foregut disorder in the western world with an enormous impact on quality of life and costs for medication [11, 12]. Obese patients are prone to suffer from GERD and all its consequences more frequently than are persons with normal body weight [13, 14]. In the long term, some of the patients develop intestinal metaplasia with goblet cells (Barrett’s esophagus) with a higher risk for esophageal adenocarcinoma (“Barrett’s cancer”) [15,16,17]. Frequent overeating of the LAGB pouch and a poorly managed gastric band with suboptimal follow-up may cause pouch distention and in some cases (e.g., persistence of a hiatal hernia) dilatation of the lower esophageal sphincter (LES). Taken together, the integrity of the esophagogastric junction, the angle of His and the LES are altered and this causes permanent exposure of gastric content to the esophagus. In the long term, this might lead to stasis esophagitis and also cause cancer [9, 18].
In order to estimate the impact of LAGB on the development of esophageal cancer in the population of Austria, we performed a nationwide survey.
Methods
In this cohort study, a questionnaire was sent to all surgical departments in Austria (119), primarily to detect cases with esophageal carcinoma after LAGB, but also to evaluate the policy in Austria concerning preoperative work-up, operation, and follow-up in LAGB patients. In detail, the survey questions focused on the number of patients and the time when LAGBs were implanted at the various surgical departments. Furthermore, we asked the departments if they performed esophageal resection and whether they had LAGB patients who had developed esophageal cancer. Moreover, we asked for preoperative diagnoses and postoperative follow-up strategies. Rate of return was 95.8% (114). All university hospitals and all other public hospitals as well as most private hospitals were addressed. Of the 114 responding departments, eight (7%) reported performing resective esophageal cancer surgery and were therefore contacted again for further investigation.
The collected data were compared with an Austrian national reporting system and proofed for plausibility [19]. The study was approved by the local Ethics Committee, No. 1015/2017.
Results
From 1994 to 2013, 36 (31.6%) of the 114 surgical departments in Austria performed a total of approximately 10.300 LAGB implantations.
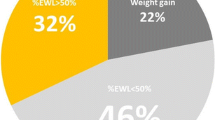
All surgical departments followed a standardized protocol for indication and preoperative diagnosis prior to LAGB implantation, namely quite similar to the IFSO recommendations. Whereas in most surgical departments (91.4%), a preoperative esophago-gastro-duodenoscopy was performed, only about a quarter (22.9%) of the departments considered preoperative esophageal manometry to be their standard. Esophageal manometry and combined 24-h pH impedance monitoring were routinely performed at 11.7% of the surgical departments prior to LAGB, whereas 28.6% of all departments performed an upper GI series with reflux provocation tests. In at least one third (34.1%) of the departments an extensive psychiatric work-up and in nearly a quarter (22.9%), a dietician was routinely included in the preoperative work-up. In 28.6% of the departments, a preoperative abdominal ultrasound examination was performed and at one surgical department (2.9%), a dexamethasone suppression test was routinely performed (Fig. 1). The follow-up policy in the various surgical departments was not standardized. The majority recommended a postoperative visit 3, 6, and 9 months after surgery followed by annual metabolic monitoring.
Of the 10.300 LAGB patients, six (0.58‰) developed a malignant neoplasia of the esophagogastric junction in median 14 (range 3–18) years after LAGB. In four (0.38‰) of them, this was an adenocarcinoma of the distal esophagus; in one patient (0.09‰), a completely dedifferentiated carcinoma of the lower esophagus (G4, UICC IV, no immunohistochemical work-up); and in one patient (0.09‰), an adenocarcinoma of the esophagogastric junction (AEG I) with peritoneal carcinosis.
Moreover, in a seventh patient, Barrett’s metaplasia with low-grade dysplasia and p53 mutation was detected.
The surgical approach was dependent on the suggestion made by the local tumor board, the clinical appearance of the patient, and the experience of the particular surgical department. A right thoracic esophageal resection with esophago-gastrostomy (Ivor Lewis procedure) was the method of choice in all surgical departments. Patients in UICC stage IV received palliative chemotherapy and best supportive care. The patient with Barrett’s metaplasia and low-grade dysplasia underwent endoscopic radiofrequency ablation. In the subsequent biopsies, no Barrett’s metaplasia and no dysplasia were detected. The band was removed endoscopically due to band erosion (Table 1).
Discussion
In our study, we interestingly found a four to fivefold risk of developing esophageal cancer after LAGB.
In the “normal” population of Austria, the incidence of esophageal cancer is currently 5/100.000 per year. About 48% of the malignant tumors of the esophagus are squamous cell carcinomas (male, 47.6%; female, 48.3%), whereas about 30% are adenocarcinomas (male, 32.6%; female, 25.3%) [20]. The WHO statistical report on esophageal cancer shows an incidence of 2.8/100.000 per year in Austria, about 1/3 of which cases are adenocarcinoma of the distal esophagus [21].
We detected six patients out of 10.300 LAGB interventions, who developed an adenocarcinoma of the lower esophagus and one patient who developed Barrett’s metaplasia with low-grade dysplasia in median 14 (range 3–18) years after LAGB. Therefore, the cumulative incidence of malignant esophageal neoplasia after LAGB might be four- to fivefold higher.
We did not focus on the individual cases and their medical history, but primarily aimed to find esophageal malignancies following LAGB. Furthermore, we aimed to evaluate the policy in Austria concerning preoperative work-up, operation, and follow-up of LAGB patients. Recent studies have attempted to focus on the development of esophageal cancer after bariatric surgery. Most of them are case reports or retrospective single-center analyses [1, 4, 6, 9, 22]. Our study includes 10.300 patients following LAGB out of the overall population of Austria (8.5 million). With 10.300 included patients and a maximum follow-up of 24 years, this is—to our knowledge—the most comprehensive study to date of the development of esophageal malignancies following LAGB.
Calculation of the risk for developing esophageal malignancies after LAGB is difficult. In our study, we compare the cumulative incidence of esophageal cancer in patients with LAGB and the incidence of esophageal cancer in the age-standardized overall population of Austria in the observation period. The weakness of the study is its retrospective design with its underreporting bias. A rare event, like the incidence of esophageal cancer in Austria as compared to a rare event like the development of esophageal cancer following LAGB, always involves a bias. Using questionnaires as a means of collecting data is far inferior to a registry. Since the Austrian National Cancer Registry [20] does not include the situation after bariatric surgery, this was the only efficient means of obtaining these data.
Furthermore, the inclusion criteria (patients who received a LAGB and subsequently developed esophageal cancer) are very broad and do not refer to any patient characteristics (e.g., age, BMI, sex).
In our social healthcare system, the threshold for undergoing bariatric surgery is quite low. Moreover, people in Austria have a low migration rate compared to, e.g., the USA. Therefore, patient migration can be neglected in our study.
So far, fewer than 15 cases of esophageal cancer after LAGB implantation have been described, but there is sound evidence that the development of Barrett’s metaplasia following LAGB is much higher [1, 2, 4, 9]. The development of esophageal cancer might be based on frequent overeating and a poorly managed gastric band with suboptimal follow-up leading to dilatation of the proximal gastric pouch. This together with the band acting as an artificial outlet obstruction leads to distension of the LES with subsequent development of a common cavity including gastric pouch and esophagus (Fig. 2). This consistently exposes the distal esophagus to gastric content like permanent reflux [9].
a The stomach after LAGB. b The stomach after LAGB with dilatation of the proximal gastric pouch. This together with the band acting as an artificial outlet obstruction leads to distension of the LES with subsequent development of a common cavity including gastric pouch and esophagus. Consequently, a combination of stasis and exposure to gastric content lead to GERD
The development of motility disorders after LAGB was already discussed a decade ago [23, 24]. However, the impact of the GERD-like situation on the esophagus after LAGB was never targeted before although the reflux-induced carcinogenesis via an esophagitis metaplasia dysplasia carcinoma sequence has already been described extensively [25,26,27].
In patients with a normal esophageal peristalsis and a competent LES, the LAGB may provide a sufficient antireflux barrier [28]. However, patients with any defect in the complex antireflux mechanism may develop GERD symptoms or pouch dilatation and show markedly elevated esophageal acidification [28, 29]. Therefore, gastroscopy with biopsy of the Z line and exclusion of motility disorders with esophageal manometry is advised prior to operation. As a consequence, the existence of Barrett’s esophagus is a commonly accepted contraindication for LAGB. Moreover, in patients with hiatal hernia, it seems logical to perform a hiatal hernia repair during LAGB. Unfortunately, according to the bariatric outcomes longitudinal database, the repair of a hiatal hernia during LAGB has minimal effect on postoperative improvement of reflux symptoms [27].
However, in gastric sleeve resection (SR), a gastric high-pressure procedure GERD may also become a serious problem. In a recent Italian cohort study, the rate of development of de novo Barrett’s metaplasia after SR was considerably higher than that reported in the current bariatric literature. This was not related to GERD symptoms [30]. Taken together, the evidence of GERD after SR is under discussion. In a review article of 2015, there was an increase in GERD symptoms after SR reported in four studies with a prevalence of about 12% while seven cohort studies reported a reduction of GERD symptoms postoperatively [31]. Interestingly, the gastric emptying time after SR is accelerated, the intragastric pressure is elevated, and the LES resting pressure is decreased [31,32,33]. However, only one single patient who developed esophageal cancer after gastric SR has been described so far [34]. Further cases might be expected in the future.
In general, bariatric surgery is associated with a decreased risk of cancers as compared to obese patients not undergoing a bariatric procedure [35,36,37].
In an English cohort study (n = 716.960), a gastric bypass resulted in the largest risk reduction for hormone-related cancers (breast, endometrium, prostate) as compared to nonoperative treatment of obesity. Nevertheless, gastric bypass, but not gastric banding or gastric SR, was associated with an increased risk for colorectal cancer. In this study, none of the bariatric procedures demonstrated a significant change in risk for esophageal cancer. However, the incidence of esophageal cancer was too low to perform a time-dependent analysis [35].
The one anastomosis gastric bypass (OAGB) is rapidly gaining acceptance and has become a mainstream bariatric procedure. In a recent systematic review, the postoperative de novo rate for GERD was about 2%. So far, there has been no report of esophageal cancer following OAGB [38].
The development of an esophageal carcinoma is a multifactorial sequence and takes time. In our six patients with esophageal carcinoma and the one patient with low-grade dysplasia, it took in median 14 (range 3–18) years from LAGB implant until cancer detection. There was no association between weight regain and esophageal cancer development.
In Austria, the number of LAGB operations per year varied over the investigated period. In the early pioneer years from 1992 to 1995, up to 550 bands were implanted with a significant increase in the following years, peaking in 2002 with 1345 operations annually. Since then, LAGB has become less popular in Austria and also worldwide weight regain, increased complications (e.g., GERD, dysphagia, stasis esophagitis, erosion) and the better outcome of alternative operations (e.g., laparoscopic gastric SR and gastric bypass), resulted in a change in procedure selection [19, 39]. This means that today, we might face a higher incidence of esophageal neoplasia 10–20 years after the maximum number of annually implanted LAGBs (Fig. 3).
Numbers of implanted LAGB over the period (in years) according to the Austrian Society for Bariatric Surgery and the national IFSO report [19]
Nevertheless, LAGB remains an important tool in bariatric surgery [40]. Selected patients without GERD, Barrett’s metaplasia, and motility disorder combined with an optimal follow-up may still take advantage of a band.
In a recent Australian cohort study, LAGB was shown to be a safe and effective treatment option for obesity also in the long term. The high frequency of late adverse events in Australian LAGB patients has been reduced following improvements made in the band, the technique of band placement, and the quality of patient education [41].
In order to avoid carcinogenesis following LAGB, accurate preoperative work-up is advisable including gastroscopy with biopsies as well as the exclusion of esophageal motility disorders.
In patients with GERD symptoms, morphological and histological changes, or impaired esophageal motility, LAGB might not be the best choice for surgical weight loss. However, in those patients, a “low-resistance” procedure, such as a gastric bypass, seems to be the better choice.
Furthermore, aggressive follow-up after LAGB in patients at risk including gastroscopy and esophageal manometry seems reasonable. In incompliant patients with frequent overeating or for poorly managed gastric bands with suboptimal follow-up, early conversion to a laparoscopic gastric bypass should be discussed.
Conclusion
The incidence of esophageal and esophagogastric junction cancer appears to be four- to fivefold higher in patients following LAGB.
References
Korswagen LA, Schrama JG, Bruins Slot W, et al. Adenocarcinoma of the lower esophagus after placement of a gastric band. Obes Surg. 2009;19(3):389–92.
Melstrom LG, Bentrem DJ, Salvino MJ, et al. Adenocarcinoma of the gastroesophageal junction after bariatric surgery. Am J Surg. 2008;196(1):135–8.
Kuruba R, Jawad M, Karl RC, et al. Technique of resection of esophageal adenocarcinoma after Roux-en-Y gastric bypass and literature review of esophagogastric tumors after bariatric procedures. Surg Obes Relat Dis. 2009;5(5):576–81.
Stauffer JA, Mathew J, Odell JA. Esophageal adenocarcinoma after laparoscopic gastric band placement for obesity. Dis Esophagus. 2011;24(1):E8–10.
Szewczyk T, Janczak P, Modzelewski B. Gastric cancer after laparoscopic adjustable gastric banding: case report. Wideochir Inne Tech Maloinwazyjne. 2012;7(3):210–2.
Scozzari G, Trapani R, Toppino M, et al. Esophagogastric cancer after bariatric surgery: systematic review of the literature. Surg Obes Relat Dis. 2013;9(1):133–42.
Wetscher GJ, Gadenstaetter M, Klingler PJ, et al. Efficacy of medical therapy and antireflux surgery to prevent Barrett’s metaplasia in patients with gastroesophageal reflux disease. Ann Surg. 2001;234(5):627–32.
Wykypiel H, Kamolz T, Steiner P, et al. Austrian experiences with redo antireflux surgery. Surg Endosc. 2005;19(10):1315–9.
Gehwolf P, Bodner J, Augustin F, et al. Swedish adjustable gastric banding – an underestimated risk factor for the development of esophageal cancer? Eur Surg. 2011;43(6):387–9.
Gehwolf P, Hinder RA, DeVault KR, et al. Significant pressure differences between solid-state and water-perfused systems in lower esophageal sphincter measurement. Surg Endosc. 2015;29(12):3565–9.
Reavis KM. Management of the obese patient with gastroesophageal reflux disease. Thorac Surg Clin. 2011;21(4):489–98.
Weitzendorfer M, Köhler G, Antoniou SA, et al. Preoperative diagnosis of hiatal hernia: barium swallow X-ray, high-resolution manometry, or endoscopy? Eur Surg. 2017;49(5):210–7.
Friedenberg FK, Xanthopoulos M, Foster GD, et al. The association between gastroesophageal reflux disease and obesity. Am J Gastroenterol. 2008;103(8):2111–22.
Nadaleto BF, Herbella FA, Patti MG. Gastroesophageal reflux disease in the obese: pathophysiology and treatment. Surgery. 2016;159(2):475–86.
Hampel H, Abraham NS, El-Serag HB. Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann Intern Med. 2005;143(3):199–211.
Lenglinger J, Izay B, Eisler M, et al. Barrett’s esophagus: size of the problem and diagnostic value of a novel histopathology classification. Eur Surg. 2009;41(1):26–39.
Koch OO, Antoniou SA. Advances in diagnosing GERD. Which examinations should be performed before interventional therapy? Eur Surg. 2016;48(4):203–8.
Antoniou SA, Anastasiadou A, Antoniou GA, et al. Preoperative nutritional counseling versus standard care prior to bariatric surgery. Eur Surg. 2017;49(3):113–7.
Beckerhinn P, Loibner-Ott N. österreichische Gesellschaft für Adipositaschirurgie. 2017 [cited 2018-08-01]; Available from: http://www.obesityteam.com/at/.
Statistik_Austria. Krebserkrankungen/Speiseröhre. 2015 [cited 2018-08-01]; Available from: http://www.statistik.at/web_de/statistiken/menschen_und_gesellschaft/gesundheit/krebserkrankungen/speiseroehre/index.html.
World Health Organization. International Agency for Reaserch on Cancer 2018 [cited 2018-08-01]; Available from: http://gco.iarc.fr/today/online-analysis-map?mode=population&mode_population=continents&population=900&sex=0&cancer=4&type=0&statistic=0&prevalence=0&color_palette=default&projection=natural-earth.
Casagrande DS, Rosa DD, Umpierre D, et al. Incidence of cancer following bariatric surgery: systematic review and meta-analysis. Obes Surg. 2014;24(9):1499–509.
Pescarus R, Sharata A, Shlomovitz E, et al. Endoscopic treatment for iatrogenic achalasia post-laparoscopic adjustable gastric banding. Surg Endosc. 2016;30(7):3099.
Wykypiel H. Pathophysiology of gastro-oesophageal reflux disease (GERD) with respect to reflux-induced carcinogenesis. Eur Surg. 2002;34:296–302.
Shaheen N, Ransohoff DF. Gastroesophageal reflux, barrett esophagus, and esophageal cancer: scientific review. JAMA. 2002;287(15):1972–81.
Nason KS et al. Gastroesophageal reflux disease symptom severity, proton pump inhibitor use, and esophageal carcinogenesis. Arch Surg. 2011;146(7):851–8.
Ardestani A, Tavakkoli A. Hiatal hernia repair and gastroesophageal reflux disease in gastric banding patients: analysis of a national database. Surg Obes Relat Dis. 2014;10(3):438–43.
Klaus A et al. Prevalent esophageal body motility disorders underlie aggravation of GERD symptoms in morbidly obese patients following adjustable gastric banding. Arch Surg. 2006;141(3):247–51.
Chen RY, Burton PR, Ooi GJ, et al. The physiology and pathophysiology of gastroesophageal reflux in patients with laparoscopic adjustable gastric band. Obes Surg. 2017;27(9):2434–43.
Genco A, Soricelli E, Casella G, et al. Gastroesophageal reflux disease and Barrett’s esophagus after laparoscopic sleeve gastrectomy: a possible, underestimated long-term complication. Surg Obes Relat Dis. 2017;13(4):568–74.
Melissas J, Braghetto I, Molina JC, et al. Gastroesophageal reflux disease and sleeve gastrectomy. Obes Surg. 2015;25(12):2430–5.
Mion F, Tolone S, Garros A, et al. High-resolution impedance manometry after sleeve gastrectomy: increased intragastric pressure and reflux are frequent events. Obes Surg. 2016;26(10):2449–56.
Melissas J, Daskalakis M, Koukouraki S, et al. Sleeve gastrectomy-a “food limiting” operation. Obes Surg. 2008;18(10):1251–6.
Scheepers AF, Schoon EJ, Nienhuijs SW. Esophageal carcinoma after sleeve gastrectomy. Surg Obes Relat Dis. 2011;7(4):e11–2.
Mackenzie H, Markar SR, Askari A, et al. Obesity surgery and risk of cancer. Br J Surg. 2018;105:1650–7.
De Pergola G, Silvestris F. Obesity as a major risk factor for cancer. J Obes. 2013;2013:291546.
Renehan AG, Soerjomataram I. Obesity as an avoidable cause of cancer (attributable risks). Recent Results Cancer Res. 2016;208:243–56.
Parmar CD, Mahawar KK. One anastomosis (mini) gastric bypass is now an established bariatric procedure: a systematic review of 12,807 patients. Obes Surg. 2018;28:2956–67.
Dargent J. Laparoscopic gastric banding: game over? Obes Surg. 2017;27(8):1914–6.
Brown WA, O’Brien PE. The band must not be abandoned. Obes Surg. 2017;27(8):1911–3.
O’Brien PE et al. Long-term outcomes after bariatric surgery: fifteen-year follow-up of adjustable gastric banding and a systematic review of the bariatric surgical literature. Ann Surg. 2013;257(1):87–94.
Funding
This study is financially supported by the Innsbruck Medical University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Statements Regarding Ethics and Consent
The study was approved by the local Ethics Committee, No. 1015/2017.
Informed Consent Statement
Does not apply.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Gehwolf, P., Kienzl-Wagner, K., Cakar-Beck, F. et al. Laparoscopic Adjustable Gastric Banding: an Underestimated Risk Factor for the Development of Esophageal Cancer?—a Nationwide Survey. OBES SURG 29, 626–631 (2019). https://doi.org/10.1007/s11695-018-3576-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3576-2