Abstract
Background
Laparoscopic sleeve gastrectomy is increasingly being used as a stand-alone procedure in bariatric surgery, with medium-term follow-up data now emerging. We present our early experience in patients with a mean body mass index (BMI) in the super-obese range.
Methods
Review of prospectively collected data for the first 100 patients who underwent laparoscopic sleeve gastrectomy at Counties Manukau District Health Board between March 2007 and July 2008.
Results
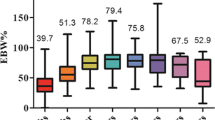
One hundred patients were identified, with a mean age of 43 years (range, 20–60 years). Maori and Pacific Islanders made up 31% of the patient subset. Patients had a mean BMI of 50.3 kg/m2 (range, 34.5–72.8 kg/m2). Forty-five patients were super-obese. The median hospital stay was 2 days (range, 1–7 days). Mean follow-up was 12.0 months (range, 0.9–23.3 months). Mean excess weight loss was 62.9% (range, 7.2–129.0%). Twenty-five percent of patients were diabetic and 45% of patients were hypertensive pre-operatively. Diabetics and hypertension resolved or improved in 72% and 60% of patients, respectively. There was a major complication rate of 7%, including three staple-line leaks (one requiring laparotomy), two staple-line bleeds (one requiring laparotomy) and one infected haematoma. There were no deaths.
Conclusions
In this public hospital setting, laparoscopic sleeve gastrectomy has achieved satisfactory weight loss results with an acceptable complication rate in the medium-term.

Similar content being viewed by others
References
Frezza EE. Laparoscopic vertical sleeve gastrectomy for morbid obesity. The future procedure of choice? Surg Tod. 2007;37:275–81.
Frezza EE, Barton A, Herbert H, et al. Laparoscopic sleeve gastrectomy with endoscopic guidance in morbid obesity. Surg Obes Rel Dis. 2008;4:575–9.
Frezza EE, Chiriva-Internati M, Wachtel MS. Analysis of the results of sleeve gastrectomy for morbid obesity and the role of ghrelin. Surg Tod. 2008;38:481–3.
Akkary E, Duffy A, Bell R. Deciphering the sleeve: technique, indications, efficacy, and safety of sleeve gastrectomy. Obes Surg. 2008;18:1323–9.
Cottam D, Qureshi FG, Mattar SG, et al. Laparoscopic sleeve gastrectomy as an initial weight-loss procedure for high-risk patients with morbid obesity. Surg End. 2006;20:859–63.
Langer FB, Reza Hoda MA, Bohdjalian A, et al. Sleeve gastrectomy and gastric banding: effects on plasma ghrelin levels. Obes Surg. 2005;15:1024–9.
Himpens J, Dapri G, Cadiere GB. A prospective randomized study between laparoscopic gastric banding and laparoscopic isolated sleeve gastrectomy: results after 1 and 3 years. Obes Surg. 2006;16:1450–6.
Wang Y, Liu J. Plasma ghrelin modulation in gastric band operation and sleeve gastrectomy. Obes Surg. 2009;19:357–62.
Uglioni B, Wolnerhanssen B, Peters T, et al. Midterm results of primary vs. secondary laparoscopic sleeve gastrectomy (LSG) as an isolated operation. Obes Surg. 2009;19:401–6.
Gumbs AA, Gagner M, Dakin G, et al. Sleeve gastrectomy for morbid obesity. Ob Surg. 2007;17:962–9.
A Portrait of Health: Key results of the 2006/07 New Zealand Health Survey. Wellington: Ministry of Health; 2008.
Fried M, Hainer V, Basdevant A, et al. Interdisciplinary European guidelines for surgery for severe (morbid) obesity. Obes Surg. 2007;17:260–70.
Karamanakos SN, Vagenas K, Kalfarentzos F, et al. Weight loss, appetite suppression, and changes in fasting and postprandial ghrelin and peptide-YY levels after Roux-en-Y gastric bypass and sleeve gastrectomy: a prospective, double blind study. Ann Surg. 2008;247:401–7.
Nocca D, Krawczykowsky D, Bomans B, et al. A prospective multicenter study of 163 sleeve gastrectomies: results at 1 and 2 years. Obes Surg. 2008;18:560–5.
Lee CM, Cirangle PT, Jossart GH. Vertical gastrectomy for morbid obesity in 216 patients: report of two-year results. Surg Endosc. 2007;21:1810–6.
Rubin M, Yehoshua RT, Stein M, et al. Laparoscopic sleeve gastrectomy with minimal morbidity. Early results in 120 morbidly obese patients. Obes Surg. 2008;18:1567–70.
Fuks D, Verhaeghe P, Brehant O, et al. Results of laparoscopic sleeve gastrectomy: a prospective study in 135 patients with morbid obesity. Surgery. 2009;145:106–13.
Sources of Funding
Tarik Sammour (the corresponding author) is supported by the Surgeon Scientist Scholarship 2009, administered through the Royal Australasian College of Surgeons.
Conflict of Interest
There is no conflict of interest pertaining to this publication from the point of view of the authors or the institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sammour, T., Hill, A.G., Singh, P. et al. Laparoscopic Sleeve Gastrectomy as a Single-Stage Bariatric Procedure. OBES SURG 20, 271–275 (2010). https://doi.org/10.1007/s11695-009-0038-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-009-0038-x