Abstract
Background
Postoperative ascites (POA) is the most common complication after liver surgery for hepatocarcinoma (HCC), but its impact on survival is not reported. The aim of the study is to investigate its impact on overall survival (OS) and disease-free survival (DFS), and secondarily to identify the factors that may predict the occurrence.
Method
Data were collected from 23 centers participating in the Italian Surgical HCC Register (HE.RC.O.LE.S. Group) between 2008 and 2018. POA was defined as ≥500 ml of ascites in the drainage after surgery. Survival analysis was conducted by the Kaplan Meier method. Risk adjustment analysis was conducted by Cox regression to investigate the risk factors for mortality and recurrence.
Results
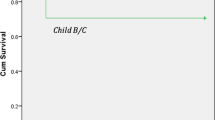
Among 2144 patients resected for HCC, 1871(88.5%) patients did not experience POA while 243(11.5%) had the complication. Median OS for NO-POA group was not reached, while it was 50 months (95%CI = 41–71) for those with POA (p < 0.001). POA independently increased the risk of mortality (HR = 1.696, 95%CI = 1.352–2.129, p < 0.001). Relapse risk after surgery was not predicted by the occurrence of POA. Presence of varices (OR = 2.562, 95%CI = 0.921–1.822, p < 0.001) and bilobar disease (OR = 1.940, 95%CI = 0.921–1.822, p: 0.004) were predictors of POA, while laparoscopic surgery was protective (OR = 0.445, 95%CI = 0.295–0.668, p < 0.001). Ninety-day mortality was higher in the POA group (9.1% vs 1.9% in NO-POA group, p < 0.001).
Conclusion
The occurrence of POA after surgery for HCC strongly increases the risk of long-term mortality and its occurrence is relatively frequent. More efforts in surgical planning should be made to limit its occurrence.


Similar content being viewed by others
References
Torzilli G. No-Mortality Liver Resection for Hepatocellular Carcinoma in Cirrhotic and Noncirrhotic Patients. Archives of Surgery 1999;134:984. https://doi.org/10.1001/archsurg.134.9.984.
Ishizawa T, Hasegawa K, Kokudo N, Sano K, Imamura H, Beck Y, et al. Risk factors and management of ascites after liver resection to treat hepatocellular carcinoma. Arch Surg 2009;144:46–51.
Famularo S, Donadon M, Cipriani F, Ardito F, Carissimi F, Perri P, et al. Hepatocellular carcinoma surgical and oncological trends in a national multicentric population: the HERCOLES experience. Updates Surg 2020. https://doi.org/10.1007/s13304-020-00733-6.
Kikuchi Y, Hiroshima Y, Matsuo K, Kawaguchi D, Murakami T, Yabushita Y, et al. A Randomized Clinical Trial of Preoperative Administration of Branched-Chain Amino Acids to Prevent Postoperative Ascites in Patients with Liver Resection for Hepatocellular Carcinoma. Ann Surg Oncol 2016;23:3727–35.
Hammond JS, Guha IN, Beckingham IJ, Lobo DN. Prediction, prevention and management of postresection liver failure. Br J Surg 2011;98:1188–200.
Citterio D, Facciorusso A, Sposito C, Rota R, Bhoori S, Mazzaferro V. Hierarchic Interaction of Factors Associated With Liver Decompensation After Resection for Hepatocellular Carcinoma. JAMA Surg 2016;151:846–53.
Yoshikawa T, Nomi T, Hokuto D, Yasuda S, Kawaguchi C, Yamada T, et al. Risk Factors for Postoperative Ascites in Patients Undergoing Liver Resection for Hepatocellular Carcinoma. World J Surg 2017;41:2095–100.
Dahm F, Georgiev P, Clavien P-A. Small-for-size syndrome after partial liver transplantation: definition, mechanisms of disease and clinical implications. Am J Transplant 2005;5:2605–10.
Famularo S, Nefotyou K, Fotiadis N, Khan N, Foxton M, Khan AZ. Small-for-Size Liver Syndrome: a Case Series with a Proposal for Management Based on Portal Flow Modulation. J Gastrointest Cancer 2015;46:185–9.
Rajakannu M, Cherqui D, Ciacio O, Golse N, Pittau G, Allard MA, et al. Liver stiffness measurement by transient elastography predicts late posthepatectomy outcomes in patients undergoing resection for hepatocellular carcinoma. Surgery 2017;162:766–74.
Shimizu T, Ishizuka M, Kato M, Aoki T, Kubota K. Hyaluronic Acid Predicts Postoperative Large Amount of Ascites after Liver Resection for Patients with Hepatocellular Carcinoma. Digestive Surgery 2016;33:520–8. https://doi.org/10.1159/000447131.
Huang L, Li J, Yan J-J, Liu C-F, Wu M-C, Yan Y-Q. Prealbumin is predictive for postoperative liver insufficiency in patients undergoing liver resection. World J Gastroenterol 2012;18:7021–5.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. PLoS Med 2007;4:e296.
Azoulay D, Eshkenazy R, Andreani P, Castaing D, Adam R, Ichai P, et al. In situ hypothermic perfusion of the liver versus standard total vascular exclusion for complex liver resection. Ann Surg 2005;241:277–85.
Chan K-M, Lee C-F, Wu T-J, Chou H-S, Yu M-C, Lee W-C, et al. Adverse outcomes in patients with postoperative ascites after liver resection for hepatocellular carcinoma. World J Surg 2012;36:392–400.
European Association for the Study of the Liver. Electronic address: easloffice@easloffice.eu, European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. J Hepatol 2018;69:406–60.
Strasberg SM, Belghiti J, Clavien P-A, Gadzijev E, Garden JO, Lau W-Y, et al. The Brisbane 2000 Terminology of Liver Anatomy and Resections. HPB 2000;2:333–9.
Balzan S, Belghiti J, Farges O, Ogata S, Sauvanet A, Delefosse D, et al. The “50-50 criteria” on postoperative day 5: an accurate predictor of liver failure and death after hepatectomy. Ann Surg 2005;242:824–8, discussion 828–9.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo Classification of Surgical Complications. Annals of Surgery 2009;250:187–96. https://doi.org/10.1097/sla.0b013e3181b13ca2.
European Association for the Study of the Liver. Electronic address: easloffice@easloffice.eu, European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol 2018;69:182–236.
Famularo S, Di Sandro S, Giani A, Lauterio A, Sandini M, De Carlis R, et al. Recurrence Patterns After Anatomic or Parenchyma-Sparing Liver Resection for Hepatocarcinoma in a Western Population of Cirrhotic Patients. Ann Surg Oncol 2018;25:3974–81.
Fernández-Esparrach G, Sánchez-Fueyo A, Ginès P, Uriz J, Quintó L, Ventura P-J, et al. A prognostic model for predicting survival in cirrhosis with ascites. Journal of Hepatology 2001;34:46–52. https://doi.org/10.1016/s0168-8278(00)00011-8.
Skrzypczyk C, Truant S, Duhamel A, Langlois C, Boleslawski E, Koriche D, et al. Relevance of the ISGLS Definition of Posthepatectomy Liver Failure in Early Prediction of Poor Outcome After Liver Resection. Annals of Surgery 2014;260:865–70. https://doi.org/10.1097/sla.0000000000000944.
Ippolito D, Famularo S, Giani A, Orsini EB, Pecorelli A, Pinotti E, et al. Estimating liver function in a large cirrhotic cohort: Signal intensity of gadolinium-ethoxybenzyl-diethylenetriamine penta-acetic acid-enhanced MRI. Dig Liver Dis 2019;51:1438–45.
Donadon M, Lanza E, Branciforte B, Muglia R, Lisi C, Pedicini V, et al. Hepatic uptake index in the hepatobiliary phase of gadolinium ethoxybenzyl diethylenetriamine penta acetic acid-enhanced magnetic resonance imaging estimates functional liver reserve and predicts post-hepatectomy liver failure. Surgery 2020;168:419–25.
Kwee SA, Wong L, Chan OTM, Kalathil S, Tsai N. PET/CT with 18F Fluorocholine as an Imaging Biomarker for Chronic Liver Disease: A Preliminary Radiopathologic Correspondence Study in Patients with Liver Cancer. Radiology 2018;287:294–302. https://doi.org/10.1148/radiol.2018171333.
Chan AWH, Zhong J, Berhane S, Toyoda H, Cucchetti A, Shi K, et al. Development of pre and post-operative models to predict early recurrence of hepatocellular carcinoma after surgical resection. J Hepatol 2018;69:1284–93.
Melloul E, Hübner M, Scott M, Snowden C, Prentis J, Dejong CHC, et al. Guidelines for Perioperative Care for Liver Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations. World J Surg 2016;40:2425–40.
Ginès P, Cárdenas A, Arroyo V, Rodés J. Management of Cirrhosis and Ascites. New England Journal of Medicine 2004;350:1646–54. https://doi.org/10.1056/nejmra035021.
Bruix J, Sherman M, American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology 2011;53:1020–2.
Santambrogio R, Kluger MD, Costa M, Belli A, Barabino M, Laurent A, et al. Hepatic resection for hepatocellular carcinoma in patients with Child–Pugh’s A cirrhosis: is clinical evidence of portal hypertension a contraindication? HPB 2013;15:78–84. https://doi.org/10.1111/j.1477-2574.2012.00594.x.
Yamashita Y-I, Ikeda T, Kurihara T, Yoshida Y, Takeishi K, Itoh S, et al. Long-Term Favorable Surgical Results of Laparoscopic Hepatic Resection for Hepatocellular Carcinoma in Patients with Cirrhosis: A Single-Center Experience over a 10-Year Period. Journal of the American College of Surgeons 2014;219:1117–23. https://doi.org/10.1016/j.jamcollsurg.2014.09.003.
Torzilli G. Minimal access liver surgery: from the escalation, to the boundaries, searching for the rules. Hepatobiliary Surg Nutr 2019;8:637–9.
Berardi G, Morise Z, Wakabayashi G, Troisi R. Propensity Score Matching Study on Laparoscopic Versus Open Resection for Hepatocellular Carcinoma in Patients with Child-Pugh Class B Liver Cirrhosis: An International Multicenter Study. HPB 2019;21:S192. https://doi.org/10.1016/j.hpb.2019.10.1542.
Buerk CA, Putnam CW, Starzl TE. Major hepatic resection and portal pressure. Surg Gynecol Obstet 1977;144:853–4.
Kanematsu T. Acute Portal Hypertension Associated With Liver Resection. Archives of Surgery 1985;120:1303. https://doi.org/10.1001/archsurg.1985.01390350083017.
Asencio JM, Vaquero J, Olmedilla L, García Sabrido JL. “Small-for-flow” syndrome: shifting the “size” paradigm. Med Hypotheses 2013;80:573–7.
Famularo S, Gianotti L, Riggio O. Small-for-flow liver failure after extended hepatectomy: hot questions and an update. Gastroenterology Insights 2017;8. https://doi.org/10.4081/gi.2017.6968.
Trutmann M, Sasse D. The lymphatics of the liver. Anatomy and Embryology 1994;190. https://doi.org/10.1007/bf00234299.
Ohtani O, Ohtani Y. Lymph circulation in the liver. Anat Rec 2008;291:643–52.
Itoh S, Uchiyama H, Ikeda Y, Morita K, Harada N, Sugimachi K, et al. Post-hepatectomy Refractory Ascites in Cirrhotic Patients with Hepatocellular Carcinoma: Risk Factor Analysis to Overcome this Problematic Complication. Anticancer Res 2017;37:1381–5.
Acknowledgments
HE.RC.O.LE.S Group Contributors: Guido Costa2; Cristina Ciulli1,6; Alessandro Giani1,6; Francesca Ratti3; Manuela Bellobono4; Elena Cremaschi5; Maria Grazia Valsecchi23; Valerio De Peppo7; Francesco Calabrese8; Giuseppina DeSario9; Giovanni Lazzari10; Alessandro Cucchetti12; Davide Cosola13; Andrea Percivale14; Michele Ciola15; Mauro Montuori16; Silvia Frassani17; Alberto Manzoni18; Luca Salvador19; Luca Pennacchi20; Pio Corleone13; Maria Conticchio21.
All authors have read and agreed to the published version of the manuscript. Conceptualization, Simone Famularo, Matteo Donadon, Fabrizio Romano, and Guido Torzilli; data curation, Guido Costa, Cristina Ciulli, Alessandro Giani, Francesca Ratti, Manuela Bellobono, Elena Cremaschi, Valerio De Peppo, Francesco Calabrese, Giuseppina DeSario, Giovanni Lazzari, Alessandro Cucchetti, Davide Cosola, Andrea Percivale, Michele Ciola, Mauro Montuori, Silvia Frassani, Alberto Manzoni, Luca Salvador, Luca Pennacchi, Pio Corleone, and Maria Conticchio; formal analysis, Simone Famularo, Davide Paolo Bernasconi, and MariaGrazia Valsecchi; investigation, Simone Famularo, Matteo Donadon, Federica Cipriani, Francesco Ardito, Maurizio Iaria, Francesca Carissimi, Pasquale Perri, Tommaso Dominioni, Matteo Zanello, Simone Conci, Sarah Molfio, Fabrizio D’Acapito, Paola Germani, Cecilia Ferrari, Stefan Patauner, Enrico Pinotti, Ivano Sciannamea, Marco Garatti, Enrico Lodo, Albert Troci, Antonella Del Vecchio, Antonio Floridi, Davide Paolo Bernasconi, Luca Fumagalli, Marco Chiarelli, Riccardo Memeo, Michele Crespi, Giacomo Zanus, Giuseppe Zimmitti, Adelmo Antonucci, Mauro Zago, Antonio Frena, Guido Griseri, Paola Tarchi, Giorgio Ercolani, Gian Luca Baiocchi, Andrea Ruzzenente, Elio Jovine, Marcello Maestri, GianLuca Grazi, Raffaele Dalla Valle, Felice Giuliante, Luca Aldrighetti, Fabrizio Romano, Guido Torzilli, Guido Costa, Cristina Ciulli, Alessandro Giani, Francesca Ratti, Manuela Bellobono, Elena Cremaschi, Valerio De Peppo, Francesco Calabrese, Giuseppina DeSario, Giovanni Lazzari, Alessandro Cucchetti, Davide Cosola, Andrea Percivale, Michele Ciola, Mauro Montuori, Silvia Frassani, Alberto Manzoni, Luca Salvador, Luca Pennacchi, Pio Corleone, and Maria Conticchio; methodology, Simone Famularo, Matteo Donadon, Davide Paolo Bernasconi, and MariaGrazia Valsecchi; project administration, Simone Famularo, Matteo Donadon, Fabrizio Romano, Guido Torzilli, and MariaGrazia Valsecchi; supervision, Marco Chiarelli, Riccardo Memeo, Michele Crespi, Giacomo Zanus, Giuseppe Zimmitti, Adelmo Antonucci, Mauro Zago, Antonio Frena, Guido Griseri, Paola Tarchi, Giorgio Ercolani, Gian Luca Baiocchi, Andrea Ruzzenente, Elio Jovine, Marcello Maestri, GianLuca Grazi, Raffaele Dalla Valle, Felice Giuliante, Luca Aldrighetti, Fabrizio Romano, Guido Torzilli, and MariaGrazia Valsecchi; writing – original draft, Simone Famularo, Matteo Donadon, Federica Cipriani, Francesco Ardito, Maurizio Iaria, Francesca Carissimi, Pasquale Perri, Tommaso Dominioni, Matteo Zanello, Simone Conci, Sarah Molfio, Fabrizio D’Acapito, Paola Germani, Cecilia Ferrari, Stefan Patauner, Enrico Pinotti, Ivano Sciannamea, Marco Garatti, Enrico Lodo, Albert Troci, Antonella Del Vecchio, Antonio Floridi, Davide Paolo Bernasconi and Luca Fumagalli; writing – review and editing, Marco Chiarelli, Riccardo Memeo, Michele Crespi, Giacomo Zanus, Giuseppe Zimmitti, Adelmo Antonucci, Mauro Zago, Antonio Frena, Guido Griseri, Paola Tarchi, Giorgio Ercolani, Gian Luca Baiocchi, Andrea Ruzzenente, Elio Jovine, Marcello Maestri, GianLuca Grazi, Raffaele Dalla Valle, Felice Giuliante, Luca Aldrighetti, Fabrizio Romano, and Guido Torzilli.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Part of the present study has been awarded with the Young Investigator Award during the Liver Cancer Summit 2020 of the European Association for the Study of the Liver (Prague, 6-8/02/2020).
Rights and permissions
About this article
Cite this article
Famularo, S., Donadon, M., Cipriani, F. et al. The Impact of Postoperative Ascites on Survival After Surgery for Hepatocellular Carcinoma: a National Study. J Gastrointest Surg 25, 2823–2834 (2021). https://doi.org/10.1007/s11605-021-04952-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-021-04952-z