Abstract
Background and aim
The latest Barcelona Clinic Liver Cancer (BCLC) staging system suggests considering surgery in patients with resectable BCLC stage 0/A hepatocellular carcinoma (HCC) and clinically significant portal hypertension (CSPH). This study aimed to evaluate the safety and short- and long-term outcomes of laparoscopic hepatectomy for BCLC stage 0/A HCC patients with CSPH.
Methods
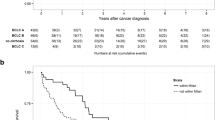
We retrospectively reviewed the medical records of 647 HCC patients in BCLC stage 0/A who were treated at five centers between January 2010 and January 2019. Among these patients, 434 underwent laparoscopic hepatectomy, and 213 underwent open hepatectomy. We used Kaplan–Meier analysis to compare the overall survival (OS) rate and recurrence-free survival (RFS) rate between patients with and without CSPH before and after propensity score matching (PSM). Multivariate Cox regression analysis was performed to identify prognostic factors for BCLC stage 0/A patients, and subgroup analyses were also conducted.
Results
Among the 434 patients who underwent laparoscopic hepatectomy, 186 had CSPH and 248 did not. The Kaplan–Meier analysis showed that the OS and RFS rates were significantly worse in the CSPH group before and after PSM. Multivariate Cox regression analyses identified CSPH as a prognostic factor for poor OS and RFS after laparoscopic hepatectomy. However, CSPH patients treated laparoscopically had a better short- and long-term prognosis than those treated with open surgery.
Conclusions
CSPH has a negative impact on the prognosis of BCLC stage 0/A HCC patients after laparoscopic hepatectomy. Laparoscopic hepatectomy is still recommended for treatment, but careful patient selection is essential.


Similar content being viewed by others
Data availability
The datasets generated and/or analyzed in the current study are not publicly available [These data are used in other studies by our team] but are available from the corresponding author on reasonable request.
Abbreviations
- CSPH:
-
Clinically significant portal hypertension
- BCLC:
-
Barcelona clinic liver cancer
- AFP:
-
Alpha-fetoprotein
- HCC:
-
Hepatocellular carcinoma
- RFA:
-
Radiofrequency ablation
- PHLF:
-
Posthepatectomy liver failure
- TACE:
-
Transcatheter arterial chemoembolization
- OS:
-
Overall survival
- RFS:
-
Recurrence-free survival
- MVI:
-
Microvascular invasion.
- HBsAg:
-
Hepatitis B surface antigen
- ALB:
-
Albumin
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- ALP:
-
Alkaline phosphatase
- GGT:
-
γ-Glutamyl transpeptidase
References
Chen Z et al (2020) Recent progress in treatment of hepatocellular carcinoma. Am J Cancer Res 10:2993–3036
Couri T, Pillai A (2019) Goals and targets for personalized therapy for HCC. Hepatol Int 13:125–137
Gunarathne LS et al (2020) Cirrhotic portal hypertension: from pathophysiology to novel therapeutics. World J Gastroenterol 26:6111–6140
Iwakiri Y, Trebicka J (2021) Portal hypertension in cirrhosis: pathophysiological mechanisms and therapy. JHEP Rep: Innov Hepatol 3:100316
Reig M et al (2022) BCLC strategy for prognosis prediction and treatment recommendation: the 2022 update. J Hepatol 76:681–693
Choi GH et al (2011) Predictive factors for long-term survival in patients with clinically significant portal hypertension following resection of hepatocellular carcinoma. Liver Int 31:485–493
Casellas-Robert M et al (2020) Laparoscopic Liver resection for hepatocellular carcinoma in Child-Pugh a patients with and without portal hypertension: a multicentre study. World J Surg 44:3915–3922
D’Silva M et al (2022) Limited liver resections in the posterosuperior segments: international multicentre propensity score-matched and coarsened exact-matched analysis comparing the laparoscopic and robotic approaches. Br J Surg 109(11):1140–1149
Aghayan DL et al (2019) Laparoscopic versus open liver resection in the posterosuperior segments: a sub-group analysis from the OSLO-COMET randomized controlled trial. HPB (Oxford) 21:1485–1490
El-Gendi A et al (2018) Laparoscopic versus open hepatic resection for solitary hepatocellular carcinoma less than 5 cm in cirrhotic patients: a randomized controlled study. J Laparoendosc Adv Surg Tech A 28:302–310
Fretland ÅA et al (2018) Laparoscopic versus open resection for colorectal liver metastases: the OSLO-COMET randomized controlled trial. Ann Surg 267:199–207
Robles-Campos R et al (2019) Open versus minimally invasive liver surgery for colorectal liver metastases (LapOpHuva): a prospective randomized controlled trial. Surg Endosc 33:3926–3936
Xia F et al (2023) Clinically Significant Portal Hypertension (CSPH) on early-stage HCC following hepatectomy: what’s the impact? Eur J Surg Oncol 49:771–779
EASL Clinical Practice Guidelines (2018) Management of hepatocellular carcinoma. J Hepatol 69:182–236
Vogel A et al (2018) Hepatocellular carcinoma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 29:iv238–iv255
Pang YY (2002) The Brisbane 2000 terminology of liver anatomy and resections. HPB 4:99–100
Rahbari NN et al (2011) Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 149:713–724
Slankamenac K et al (2013) The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg 258:1–7
Barron JO et al (2022) Validation of the IWATE criteria as a laparoscopic liver resection difficulty score in a single North American cohort. Surg Endosc 36:3601–3609
Labadie KP et al (2022) IWATE criteria are associated with perioperative outcomes in robotic hepatectomy: a retrospective review of 225 resections. Surg Endosc 36:889–895
Ishizawa T et al (2012) Laparoscopic segmentectomy of the liver: from segment I to VIII. Ann Surg 256:959–964
Azoulay D et al (2021) Liver resection for hepatocellular carcinoma in patients with clinically significant portal hypertension. JHEP Rep: Innov Hepatol 3:100190
Choi SB et al (2014) Influence of clinically significant portal hypertension on surgical outcomes and survival following hepatectomy for hepatocellular carcinoma: a systematic review and meta-analysis. J Hepatobiliary Pancreat Sci 21:639–647
Zheng J et al (2021) Safety and feasibility of laparoscopic liver resection for hepatocellular carcinoma with clinically significant portal hypertension: a propensity score-matched study. Surg Endosc 35:3267–3278
Giannini EG et al (2013) Influence of clinically significant portal hypertension on survival after hepatic resection for hepatocellular carcinoma in cirrhotic patients. Liver Int 33:1594–1600
Hobeika C et al (2020) Influence of surgical approach and quality of resection on the probability of cure for early-stage HCC occurring in cirrhosis. JHEP Rep: Innov Hepatol 2:100153
Levi Sandri GB et al (2018) Laparoscopic liver resection for large HCC: short- and long-term outcomes in relation to tumor size. Surg Endosc 32:4772–4779
Reddy SK et al (2011) Laparoscopic liver resection. World J Surg 35:1478–1486
Harada N et al (2016) Laparoscopic liver resection is a feasible treatment for patients with hepatocellular carcinoma and portal hypertension. Anticancer Res 36:3489–3497
Søreide JA, Deshpande R (2021) Post hepatectomy liver failure (PHLF)—recent advances in prevention and clinical management. Eur J Surg Oncol: J Eur Soc Surg Oncol British Assoc Surg Oncol 47:216–224
Sposito C et al (2021) Preoperative predictors of liver decompensation after mini-invasive liver resection. Surg Endosc 35:718–727
Wang YY et al (2021) Development and Validation of a nomogram to preoperatively estimate post-hepatectomy liver dysfunction risk and long-term survival in patients with hepatocellular carcinoma. Ann Surg 274:e1209–e1217
Yu Q et al (2022) An imaging-based artificial intelligence model for non-invasive grading of hepatic venous pressure gradient in cirrhotic portal hypertension. Cell Rep Med 3:100563
Liu Y et al (2020) Deep convolutional neural network-aided detection of portal hypertension in patients with cirrhosis. Clin Gastroenterol Hepatol 18:2998-3007.e5
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Feng Xia, Qiao Zhang, Elijah Ndhlovu, Jun Zheng, Minggang Yuan, Hengyi Gao, and Guobing Xia declare no conflicts of interest.
Ethical approval
The Ethics Committees of Wuhan Tongji Hospital, Zhongshan People’s Hospital, Huangshi Central Hospital, Shenzhen Baoan District People's Hospital, and Shenzhen Longhua District People’s Hospital approved this retrospective observational study.
Informed consent
All patients provided informed consent to the use and publication of their information.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.




Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xia, F., Zhang, Q., Ndhlovu, E. et al. Prognosis and safety of laparoscopic hepatectomy for BCLC stage 0/A hepatocellular carcinoma with clinically significant portal hypertension: a multicenter, propensity score-matched study. Surg Endosc 38, 799–812 (2024). https://doi.org/10.1007/s00464-023-10589-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10589-7