Abstract
Purpose
Various generic and disease-specific quality of life instruments are available to assess outcome following surgery. However, they may not be sensitive to changes in outcome in the early postoperative period, which is important when assessing changes in surgical technique and perioperative care. The Abdominal Surgery Impact Scale (ASIS) is a validated instrument designed to assess short-term outcome following surgery. Thus, the aims of this study were to assess the impact of surgery on patients undergoing ileal pouch anal anastomosis (IPAA), assess factors which might impact on outcome, and lastly, further evaluate the reliability and internal consistency of the ASIS.
Methods
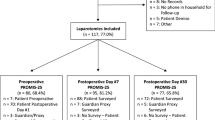
Patients over the age of 18 who had an IPAA between March 2005 and October 2007 completed the ASIS on postoperative day 3 and at the time of discharge. The ASIS contains 18 items within six domains with possible scores ranging from 18 to 126. Demographic, clinical and surgical data, postoperative complications, and length of stay were also recorded. Internal reliability of the ASIS was measured using Cronbach’s alpha coefficient.
Results
Ninety-two patients (36 female, 56 male, mean age = 36.8 ± 10.8) completed the ASIS at two time intervals (mean 3 days and mean 7 days postoperatively). Forty-seven patients had an IPAA performed with an ileostomy; 11 patients had the IPAA performed laparoscopically. The mean hospital stay was 10.8 days. The overall mean ASIS score significantly increased over the two time periods (mean 56.9 ± 18.3 vs. 81.8 ± 17.3, p < 0.001). Patients who had an ileostomy had a significantly lower mean score at discharge (77.32 vs. 86.82), secondary to lower scores on the physical limitations, functional impairment, and visceral function domains. Seven (7.8%) patients had ileo-anal anastomotic leaks, and seven (7.8%) patients had small bowel obstructions. These patients had an increased length of stay, whereas patients having laparoscopic surgery had a significantly shorter length of stay (8.8 days vs. 11.1 days), but there was no significant difference in mean ASIS scores. Cronbach’s alpha coefficient was 0.94 overall and ranged from 0.69 to 0.91 for subscales indicating internal reliability.
Conclusions
ASIS is a valid instrument for measuring quality of life in the postoperative period and is responsive to changes over time. Although quality of life increases postoperatively during hospital stay, at discharge, patients with IPAA still have decreased quality of life. Patients with ileostomies have further decreased scores.
Similar content being viewed by others
References
Parks AG, Nicholls RJ. Proctocolectomy without ileostomy for ulcerative colitis. BMJ 1978;2(6130):85–88.
Fazio VW, Ziv Y, Church JM, Oakley JR, Lavery IC, Milsom JW, Schroeder TK. Ileal pouch–anal anastomoses complications and function in 1005 patients. Ann Surg 1995;222(2):120–127. doi:10.1097/00000658-199508000-00003.
Meagher AP, Farouk R, Dozois RR, Kelly KA, Pemberton JH. J ileal pouch–anal anastomosis for chronic ulcerative colitis: complications and long-term outcome in 1310 patients. Br J Surg 1998;85(6):800–803. doi:10.1046/j.1365-2168.1998.00689.x.
McMullen K, Hicks T, Ray J, Gathright JB, Timmcke AE. Complications associated with ileal pouch–anal anastomosis. World J Surg 1991;15:763–766. doi:10.1007/BF01665312.
Oresland T, Fasth S, Nordgren S, Hulten L. The clinical and functional outcome after restorative proctocolectomy. A prospective study in 100 patients. Int J Colorectal Dis 1989;4(1):50–56.
Pemberton JH, Kelly KA, Beart RW Jr, Dozois RR, Wolff BG, Ilstrup DM. Ileal pouch–anal anastomosis for chronic ulcerative colitis. Long-term results. Ann Surg 1987;206(4):504–513. doi:10.1097/00000658-198710000-00011.
Poppen B, Svenberg T, Bark T, Sjogren B, Rubio C, Drakenberg B, Slezak P. Colectomy–proctomucosectomy with S-pouch: operative procedures, complications, and functional outcome in 69 consecutive patients. Dis Colon Rectum 1992;35:40–47. doi:10.1007/BF02053337.
Skarsgard ED, Atkinson KG, Bell GA, Pezim ME, Seal AM, Sharp FR. Function and quality of life results after ileal pouch surgery for chronic ulcerative colitis and familial polyposis. Am J Surg 1989;157:467–471. doi:10.1016/0002-9610(89)90636-3.
Delaney CP, Fazio VW, Remzi FH, Hammel J, Church JM, Hull TL, Senagore AJ, Strong SA, Lavery IC. Prospective, age-related analysis of surgical results, functional outcome, and quality of life after ileal pouch–anal anastomosis. Ann Surg 2003;238(2):221–228.
Muir AJ, Edwards LJ, Sanders LL, Bollinger RR, Koruda MJ, Bachwich DR, Provenzale D. A prospective evaluation of health-related quality of life after ileal pouch anal anastomosis for ulcerative colitis. Am J Gastroenterol 2001;96(5):1480–1485. doi:10.1111/j.1572-0241.2001.03801.x.
Urbach DR, Harnish JL, McIlroy JH, Streiner DL. A measure of quality of life after abdominal surgery. Qual Life Res 2006;15(6):1053–1061. doi:10.1007/s11136-006-0047-3.
Huber PJ. Robust regression: asymptotics, conjectures and Monte Carlo. Ann Stat 1973;1(5):1799–1821.
Lee AH, Gracey M, Wang K, Yau KK. A robustified modeling approach to analyze pediatric length of stay. Ann Epidemiol 2005;15(9):673–677. doi:10.1016/j.annepidem.2004.10.001.
Becker JM. Surgical therapy for ulcerative colitis and Crohn’s disease. Gastroenterol Clin North Am 1999;28(2):371–90. viii–ix doi:10.1016/S0889-8553(05)70061-3.
Calman KC. Quality of life in cancer patients—a hypothesis. J Med Ethics. 1984;10(3):124–127. doi:10.1136/jme.10.3.124.
Berndtsson I, Lindholm E, Oresland T, Borjesson L. Long-term outcome after ileal pouch–anal anastomosis: function and health-related quality of life. Dis Colon Rectum 2007;50(10):1545–1552. doi:10.1007/s10350-007-0278-6.
Berndtsson I, Oresland T. Quality of life before and after proctocolectomy and IPAA in patients with ulcerative proctocolitis—a prospective study. Colorectal Dis. 2003;5(2):173–179. doi:10.1046/j.1463-1318.2003.00455.x.
Thirlby RC, Sobrino MA, Randall JB. The long-term benefit of surgery on health-related quality of life in patients with inflammatory bowel disease. Arch Surg. 2001;136(5):521–527. doi:10.1001/archsurg.136.5.521.
Tiainen J, Matikainen M. Health-related quality of life after ileal J-pouch–anal anastomosis for ulcerative colitis: long-term results. Scand J Gastroenterol. 1999;34(6):601–605. doi:10.1080/003655299750026065.
Weeks JC, Nelson H, Gelber S, Sargent D, Schroeder G. Short-term quality-of-life outcomes following laparoscopic-assisted colectomy vs open colectomy for colon cancer: a randomized trial. JAMA 2002;287(3):321–328. doi:10.1001/jama.287.3.321.
Dunker MS, Bemelman WA, Slors JF, van Duijvendijk P, Gouma DJ. Functional outcome, quality of life, body image, and cosmesis in patients after laparoscopic-assisted and conventional restorative proctocolectomy: a comparative study. Dis Colon Rectum 2001;44(12):1800–18007. doi:10.1007/BF02234458.
Urbach DR. Laparoscopic-assisted surgery for colon cancer. JAMA 2002;287(15):1938. author reply 1939 doi:10.1001/jama.287.15.1938.
Camilleri-Brennan J, Munro A, Steele RJ. Does an ileoanal pouch offer a better quality of life than a permanent ileostomy for patients with ulcerative colitis? J Gastrointest Surg 2003;7(6):814–819. doi:10.1016/S1091-255X(03)00103-3.
Farouk R, Pemberton JH, Wolff BG, Dozois RR, Browning S, Larson D. Functional outcomes after ileal pouch-anal anastomosis for chronic ulcerative colitis. Ann Surg 2000;231(6):919–926. doi:10.1097/00000658-200006000-00017.
Author information
Authors and Affiliations
Corresponding author
Appendix 1
Appendix 1
Abdominal Surgery Impact Scale (ASIS)
I cannot climb a flight of stairs | Strongly agree | Agree | Somewhat agree | Neither agree nor disagree | Somewhat disagree | Disagree | Strongly disagree |
I am not able to move easily | Strongly agree | Agree | Somewhat agree | Neither agree nor disagree | Somewhat disagree | Disagree | Strongly disagree |
I am not able to stand comfortably for five minutes | Strongly agree | Agree | Somewhat agree | Neither agree nor disagree | Somewhat disagree | Disagree | Strongly disagree |
It is difficult for me to get dressed | Strongly agree | Agree | Somewhat agree | Neither agree nor disagree | Somewhat disagree | Disagree | Strongly disagree |
I am unable to care for myself | Strongly agree | Agree | Somewhat agree | Neither agree nor disagree | Somewhat disagree | Disagree | Strongly disagree |
I feel dependent on others to care for me | Strongly agree | Agree | Somewhat agree | Neither agree nor disagree | Somewhat disagree | Disagree | Strongly disagree |
I am afraid to move because it might cause pain | Strongly agree | Agree | Somewhat agree | Neither agree nor disagree | Somewhat disagree | Disagree | Strongly disagree |
I have severe pain in and around my abdomen | Strongly agree | Agree | Somewhat agree | Neither agree nor disagree | Somewhat disagree | Disagree | Strongly disagree |
My incision(s) is/are causing me pain | Strongly agree | Agree | Somewhat agree | Neither agree nor disagree | Somewhat disagree | Disagree | Strongly disagree |
I am not able to move my bowels normally | Strongly agree | Agree | Somewhat agree | Neither agree nor disagree | Somewhat disagree | Disagree | Strongly disagree |
I am uncomfortable because I am thirsty | Strongly agree | Agree | Somewhat agree | Neither agree nor disagree | Somewhat disagree | Disagree | Strongly disagree |
I do not have a good appetite | Strongly agree | Agree | Somewhat agree | Neither agree nor disagree | Somewhat disagree | Disagree | Strongly disagree |
I wake up feeling that sleep has not refreshed me | Strongly agree | Agree | Somewhat agree | Neither agree nor disagree | Somewhat disagree | Disagree | Strongly disagree |
I have trouble falling asleep | Strongly agree | Agree | Somewhat agree | Neither agree nor disagree | Somewhat disagree | Disagree | Strongly disagree |
I wake up a lot in the night | Strongly agree | Agree | Somewhat agree | Neither agree nor disagree | Somewhat disagree | Disagree | Strongly disagree |
I have difficulty concentrating on what I am doing (conversation, watching TV, or reading) | Strongly agree | Agree | Somewhat agree | Neither agree nor disagree | Somewhat disagree | Disagree | Strongly disagree |
I feel helpless | Strongly agree | Agree | Somewhat agree | Neither agree nor disagree | Somewhat disagree | Disagree | Strongly disagree |
I feel anxious | Strongly agree | Agree | Somewhat agree | Neither agree nor disagree | Somewhat disagree | Disagree | Strongly disagree |
Rights and permissions
About this article
Cite this article
Datta, I., O’Connor, B., Victor, J.C. et al. Abdominal Surgery Impact Scale (ASIS) is Responsive in Assessing Outcome Following IPAA. J Gastrointest Surg 13, 687–694 (2009). https://doi.org/10.1007/s11605-008-0793-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-008-0793-3