Abstract
Introduction
Abdominal wall herniation (AWH) is an increasing problem for patients, surgeons, and healthcare providers. Surgical-site specific outcomes, such as infection, recurrence, and mesh explantation, are improving; however, successful repair still exposes the patient to what is often a complex major operation aimed at improving quality of life. Quality-of-life (QOL) outcomes, such as aesthetics, pain, and physical and emotional functioning, are less often and less well reported. We reviewed QOL tools currently available to evaluate their suitability.
Methods
A systematic review of the literature in compliance with PRISMA guidelines was performed between 1st January 1990 and 1st May 2019. English language studies using validated quality-of-life assessment tool, whereby outcomes using this tool could be assessed were included.
Results
Heterogeneity in the QOL tool used for reporting outcome was evident throughout the articles reviewed. AWH disease-specific tools, hernia-specific tools, and generic tools were used throughout the literature with no obviously preferred or dominant method identified.
Conclusion
Despite increasing acknowledgement of the need to evaluate QOL in patients with AWH, no tool has become dominant in this field. Assessment, therefore, of the impact of certain interventions or techniques on quality of life remains difficult and will continue to do so until an adequate standardised outcome measurement tool is available.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Abdominal wall herniation (AWH) is an increasing problem for patients, surgeons, and healthcare providers. The incidence of ventral incisional hernia (IH) following major abdominal surgery is high, with rates of up to 20% following midline laparotomy [1, 2]. Advances in critical care and surgical technique are leading to improved survival following abdominal catastrophe in patients with multiple co-morbidities, with a resulting increasing burden of complex abdominal wall herniation (CAWH) [3]. Surgeons with a specialist interest in abdominal wall reconstruction within the context of a multi-disciplinary team (MDT), with careful recording of technique and outcomes [4, 5], are best suited to manage these complex patients.
Surgical-site infection, recurrence, length of stay, and mesh explantation are the most commonly utilised outcome measures in abdominal wall surgery, and these are improving, with many patients seeing excellent long-term results [6, 7]. However, a significant proportion of these operations are performed for symptom relief and to improve the quality of life (QOL). Despite this, QOL outcomes are recorded far less frequently than surgeon centred outcomes and surgical-site outcomes form the basis of the majority of publications from centres of excellence.
Assessment of QOL, both pre- and post-surgery, has been shown to be an important patient-reported outcome in all types of abdominal surgery [8, 9] and various tools are used. Generic QOL scoring systems have been used for many years, but disease-specific quality-of-life models are frequently more useful. A few data from specific AWH QOL-related studies exist [10, 11], and consequently, there remains an absence of consensus agreement surrounding the best way to measure QOL in AWH. Consistency in recording allows comparison between centres, techniques, and mesh type and position. The use of both generic and disease-specific QOL assessment tools is the current gold standard in surgery in general, and as such, a singly accepted tool for assessing QOL in AWH would appear to still be lacking. We hypothesise that there is no acceptable QOL assessment tool currently in use for patients undergoing abdominal wall hernia repair. The aim of this review is to systematically evaluate all currently available tools for measuring QOL (both generic and disease-specific) in this patient group to understand more thoroughly why this is the case.
Methods
A focussed, systematic review of the literature was conducted by the first author (T.G.) under the guidance of a qualified medical librarian, in keeping with the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines.
PubMed, MEDLINE, and EMBASE and Trip databases were used to search for comparative literature between 1st January 1990 and 1st May 2019. English language studies using quality-of-life assessment tools in abdominal wall hernias were included. The latest date for this search was 1st May 2019.
Search string
-
1.
To identify studies of AWH disease, we used the MeSH terms “abdominal wall hernia”, “incisional hernia”, “ventral hernia”, “recurrent hernia”, and “post-operative hernia”. There were combined with the keywords “abdominal wall reconstruction”.
-
2.
To identify studies of quality-of-life assessment tools, we used the MeSH terms “Quality of Life”, “Patient recorded outcome(s)” combined with the key words “assessment”, “tool”, and “scale”.
A complete search string is shown in Table 1 in the supplementary material.
Data extraction and review of studies
Articles were split into two groups and reviewers (TNG and LJM) independently extracted the following data points from the included studies: first author, year of publication, primary study centre, study design, type of hernia, quality of life tool, number of patients, percentage of patients with at least 1 year follow-up, type of hernia repair, mesh use, and timing of quality-of-life assessment.
Inclusion criteria
Inclusion required the studies to utilise a formal quality-of-life assessment tool. Included studies must have reported on AWH, including IH and primary ventral hernias (VH). We defined a hernia as a musculofascial defect associated with protrusion of intra-abdominal viscera as described by the European hernia society [12]. This was further defined into primary or incisional and according to anatomical location. Quality-of-life assessment must be an identified outcome measure. Where reported, surgical site outcomes and complications were considered if part of the quality-of-life assessment. We stipulated no minimum follow-up time for inclusion.
Exclusion criteria
Studies reporting groin hernias, lumbar hernias, and para-stomal hernias only were excluded. We excluded any study which reported on mixed hernia types if we were unable to independently extract the data pertaining specifically to AWH. Individual case reports and non-English language studies were excluded. We excluded paediatric studies (studies in patients under the age of 18) and studies focused on specific disease conditions (e.g., colorectal surgery and liver transplantation) other than AWH or VH.
Citation management and screening
Initial search of the relevant databases identified a total of 1502 studies using the keywords outlined. After removal of duplicates and review of the title and the abstract, 95% of articles were excluded. All articles considered unsuitable for review were excluded (e.g., subject not AWH or QOL). Further review of the abstract and application of inclusion and exclusion criteria left 38 papers included for full review. Full article review leads to another 6 papers being excluded (3 groin hernia studies, 2 primary non-English language studies, and 1 study reviewing quality-of-life post-transplantation). A log of the matching process can be seen in the PRISMA flow diagram (see Fig. 1). Mendeley reference manager was used to manage citations (Mendeley Desktop v 1.19.4, UK).
Data management and outcomes
Our primary outcome of interest is QOL assessment method in AWH patients. This will allow us to evaluate the different QOL assessment tools and better understand the current lack of consensus within this field. We extracted the timing of use of QOL assessment tool (preoperatively and postoperatively) for comparison of scores.
To assess participant characteristics, we aimed to identify if basic patient demographics were reported including sex, age, BMI, smoking status, and assessment of co-morbidities. If it was a comparative study, we aimed to identify if intervention and control group participant demographics were comparable. We also aimed to identify hernia size, mesh usage, mesh type, mesh placement, method of securing mesh, and adverse surgical outcomes.
Where there was conflict or disagreement between reviewers, this was resolved in a face-to-face meeting. Identified citations and outcome parameters were entered into a spreadsheet using Microsoft Excel for Mac 2011 (version 14.5.2).
Results
The final review included 32 articles from an initial 1502 search results. The aggregated data from all 32 articles can be seen in Table 2 in the supplementary material.
Case-mix and demographics
Thirty-two articles included a total of 6578 patients with AWH including VH, IH, recurrent ventral (RVH) and recurrent incisional hernia (RIH), across 25 sites in 9 countries. QOL was measured in all of the studies using a formalised assessment tool and was the primary outcome measure in 20 of the 32 included. In nine articles, it was the sole outcome measure. Other outcome measures included, most commonly, surgical site occurrence, and physical function such as strength and flexion. Type of hernia repair varied greatly across the studies and included open repair with and without mesh, laparoscopic repair with and without mesh, and anterior or posterior component separation. Twenty-two papers comment specifically on mesh being used for repair re-enforcement. Hernia size was referenced in 27 of the included studies, although a few studies report on the impact of hernia size on QOL. All studies included in the review assessed both male and female patients.
Quality-of-life assessment tools
We found heterogeneity in the tools for assessment of QOL throughout the included articles. Seven used an abdominal wall-specific QOL tool, 11 used a hernia-specific QOL tool, 16 used a generic validated QOL tool, and 6 used a generic non-validated or independently devised QOL tool. Tool usage varied throughout the studies (see Table 1).
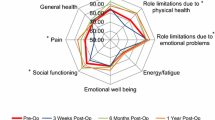
Generic tools
SF-36 provides a QOL score based on mental and physical health and was the most commonly used QOL assessment tool seen in this review (12 studies of 1214 patients). However, only 2 [21, 29] articles used it as their sole method for collecting QOL data. Both saw improvement in mental and physical scores post AWR. SF-36 was used in combination with hernia-specific tools [25,26,27], AWH-specific tools [41], and other generic tools [22, 30,31,32,33]. Co-morbidities, BMI, and smoking status were reported separately.
SF-12 is a truncated version of SF-36 shown to give comparable results [50]. However, it was only used in two included studies [34, 35] (139 patients) for assessing post-operative QOL in AWH repair. Scott-Roth et al. [34] found that morbidity from biological mesh was higher than expected, but SF-12 QOL scores at 12 months were above baseline with 88% follow-up at 12 months. Rosen et al. [35] reported improvements in QOL using SF-12, in combination with an EQ-5D and EQ-VAS, following AWR with biosynthetic mesh in both the mental and physical domains.
EQ-5D is a standardised measurement of health-related QOL consisting of a questionnaire and a visual acuity scale EQ-VAS. It was designed to quantify generic patient-reported outcomes based on mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. QOL scores from EQ-5D have been shown to be comparable to those using a hernia-specific tool (Carolinas Comfort Scale) following component separation (CS) mesh repair [22]. However, only 2 studies [22, 35] included in this review used EQ-5D and EQ-VAS, and although follow-up was good at 1 year (84–100%), the studies only included 138 patients. Furthermore, both used at least one other QOL assessment tool including SF-12 and the Carolinas Comfort Scale (CCS).
Karnofsky performance status (KPS) measures functional impairment due to any disease. Only one study [28] using KPS (in conjunction with SF-36) post-operatively in 71 patients at 1 year found that patients were limited to basic self-care and the inability to return to work was identified using this tool. KPS is not comparable to SF-36 and no pre-operative QOL scores were assessed using this tool.
WHOQOL-BREF provides a short-form QOL assessment in physical health, psychological impact, social relationships, and environment. It was used as the sole method for QOL assessment in one included study in this review [29] of 90 patients undergoing laparoscopic AWR with mesh. No significant improvement in quality of life after surgery was seen. Gender, BMI, smoking status, and time to return to work are not included in the 26-question tool, but are commented on separately by the authors.
Hernia-specific tools
The Carolinas Comfort Scale (CCS) assess QOL based on movement, daily functioning, mesh sensation, and pain across a 6-point scale. Validated in all hernia types undergoing mesh repair; it is the only tool of its type. It was used in 11 studies including 4152 patients. It is the only tool of its type, and although it has been shown to be more sensitive for assessing QOL in hernia than generic tools [9, 10], it was used as the sole QOL assessment tool in only seven articles reviewed (see Table 2).
Heniford et al. [10] assessed QOL using CCS in 3877 hernia patients undergoing repair with mesh in a multinational prospective study; one-third had AWH. With 87% follow-up at 1 year, improvements in QOL were seen across all domains apart from mesh sensation. The study’s ability to compare the relative merits of CCS compared to other tools was limited, as the cohort registry did not complete a generic QOL assessment.
Three articles [25,26,27] used SF-36 and CCS, albeit in only 174 patients. However, all showed correlation in comparative scores in improvement of QOL post-operatively between CCS and SF-36. Nielsen et al. [26] state 79% of patients preferred CCS to SF-36 and 83% considered it a better reflection of their QOL post hernia repair. Hope et al. [27] corroborate this reporting patient preference of CCS in favour of SF-36 at 3:1 in 56 patients. Body mass index, smoking status, and other co-morbidities do not feature in the tool, but were considered important to report by all of the studies.
Abdominal wall hernia-specific tools
The Hernia-related QOL Survey (HerQLes) tool was designed in 2012 to assess QOL specifically in AWH [16]. The 12-point survey allows patients to score their own physical and emotional functioning. HerQLes was the most widely used AWH QOL tool in this review albeit in only five studies. QOL using HerQLes was reported on in 493 patients who underwent AWR with mesh highlighting AWH as a significant barrier to QOL. Feng et al. [15] showed that early hernia repair improves quality of life in cancer survivorship using HerQLes. Krpata et al. [13] also demonstrated improved post-operative QOL scores using HerQLes in AWH. Importantly, four of the five studies used HerQLes as their sole method of QOL assessment. All five studies made separate comments to co-morbidities, age, gender, and smoking status.
The modified activities’ assessment scale (AAS) assesses patient functioning and QOL [41] through questions surveying mood, lifestyle, and physical activity [43]. It was only used for QOL assessment in two of the included studies, both in the last 5 years. Cherla et al. [17] assessed QOL using AAS in patients with AHW undergoing reconstruction.
Post-operatively patients undergoing AWR experienced improved QOL. Some achieving QOL scores similar to the control, no hernia, group on the AAS. However, no use of a generic tool makes interpretation difficult. Langbach et al. [24] used AAS as well as SF-36 to assess QOL in AWH patients undergoing AWR reporting QOL scores using both tools were improved and comparable following mesh repair. Again, body mass index, age, and co-morbidities were matched across the groups and reported separately.
Utilisation of QOL assessment
Fourteen studies included in our review sought to determine whether simply reconstructing an abdominal wall/repairing a hernia would improve QOL using a wide range of QOL tools. Despite this, these 14 studies failed to incorporate the full range of tools available. The remainder of the studies sought to determine the impact of certain pre-and peri-operative variables on hernia repair success and QOL, with a perceived inherent assumption that it would be increased by virtue of surgery. There was again a failure to utilise the range of currently available tools (see Table 3). QOL tools were used alone and in combination with other tools without dominance in one tool or one combination of tools being used within the field.
Tool acceptability, completion rates, and follow-up statistics
Patient participation and follow-up at 1 year were poor throughout the studies. Twenty studies (65%) reported follow-up to 1 year. Follow-up ranged from 3 months up to 14 years [33]. Post-operative follow-up was varied and inconsistent across all the included studies. One study collected pre-operative data only, 21 studies collected pre- and post-operative data and 10 studies collected post-operative data only (see Table 4). The majority of studies (65%) included more women than men and the mean patient age (45.9–64) was above average childbearing age with women of childbearing age significantly underrepresented. Impact of size of hernia was difficult to determine as it does not feature in any QOL assessment tool and hernias of all sizes are included in data sets without discrimination. However, as Nissen et al. have reported, larger hernias are likely negatively impacts on QOL.
Comment on patient post-operative satisfaction was noted in a number of studies [28,29,30,31], but the report on satisfaction with the quality-of-life tool used was sparse. Patient preference for a hernia-specific tool over a generic tool was observed in two studies. Nielsen et al. [26] specifically reported on patient satisfaction and perceived acceptability of tools where 75% of patients included preferred CCS to SF-36 due to ease of understanding and 83% felt it to be more specific to their situation. Hope et al. [27] corroborated this. Patient satisfaction with AWH or preference.
Discussion
Abdominal wall reconstruction as a specialty in its own right is growing rapidly. Unlike other specialities, it mostly consists of elective cases performed to improve quality of life. This allows for thorough pre-operative planning and patient discussion. A systematic review undertaken by Jensen et al. [44] reviewed the then available QOL assessment tools and determined none were universally accepted. Despite the recognised need for a standardised method for quality-of-life assessment in AWR still, no one tool has become dominant. More recently, Sando et al. in 2020 have published a comprehensive systematic review assessing long-term patient-recorded outcomes from ventral hernia repair with mesh specifically. They have shown that some factors used for assessing QOL may have improved following surgery. A wide range and varied use of QOL assessment tools were again noted and drawing strong conclusions is perhaps impeded by difficulties in comparing outcomes because of this. This review was performed to provide up-to-date information with the emphasis on determining the use and acceptability of currently available tools for the AWH population to understand why this is still the case.
We have identified significant heterogeneity within the AWH literature with a total of 14 different QOL tools being used across 32 studies. Furthermore, we have seen two distinct sub-groups of studies; the first are studies using QOL tools to assess if repairing AWHs improves QOL in patients at all. The second utilise QOL tools to measure any difference in outcome between different techniques or interventions. Here, mesh position and plane development were frequently reported in studies comparing operative technique, but analysis of any relationship to QOL is frustrated by the absence of a common nomenclature to describe mesh placement [45]. It is somewhat surprising that this group only includes 14 studies given that presumed improvement in QOL secondary to surgery is one of the key factors in patient and surgeon decision-making. Timing of data collection and follow-up duration varied greatly across the studies, suggesting that optimum follow-up time also remains unclear.
Generic QOL tools provide a general overview of perceived QOL, whereas disease-specific surveys are useful in detecting the change in health and QOL as the result of a specific condition and/or the impact of a given focused treatment [39]. They are long established and widely accepted in their role measuring all health-related QOL. SF-36 and SF-12 have been used in the literature since 1989 with similar results [46]. They are extensively validated and give a ‘common language’ to researchers. They are adaptable and translatable within the general populations. However, their ability to assess specific pathology populations limited [47]. This was further highlighted by the National Health Service in the UK as part of their national patient-recorded outcome measures’ (PROMs) programme. It found, following a survey of 69,677 patients with inguinal hernia in 2016/17, that generic or non-hernia-specific PROMs were of limited value, and consequently, inguinal hernia was removed from the programme. AWH patients have different experiences both pre- and post-operatively compared to the daily lives of the ‘normal population’ [48] and have often suffered a significant surgical history with subsequent psychological impact [23]. Consequently, we have found in the last decade, hernia-specific QOL tools have gained popularity. In particular, CCS has been validated in large cohorts and shown to give a better representation of patients’ quality of life following hernia repair with mesh [11] and is preferable with patients.
Generic tools are still the most commonly used QOL assessment tools within the AWH literature. Where hernia-specific tools are used, it is often in combination with a generic tool; perhaps, to ensure that some comparable data are collected using the more validated, established method. Perhaps also highlighting inadequacies within the available disease-specific tools. General hernia-specific tools may be more focused than generic tools and their use is well established within the groin hernia literature [9]. However, we are concerned that they do not contain some specific domains important in the AWH population. We are also concerned that filling in two questionnaires is time-consuming for patients and may lead to a reduction in engagement and potential misrepresentation of outcomes. This has led to the development of AWH QOL-specific tools. Availability and uptake of AWH-specific tools have also been fairly limited. The European Hernia Society has developed and published the Eura-HSQOL in 2016 designed for use specifically in patients undergoing AWR as it was felt that other tools for evaluating QOL after hernia repair have not proven useful. This would appear to confirm a reluctance to consistently use other available tools. Unfortunately, its uptake has also been limited and it was not used in any identified studies within our review. Why utilisation and uptake remain low is unclear and from our review further research appears still required for using an AWH-specific tool. We suspect that this may be because AWH-specific tools still omit certain factors which may be important in measuring quality of life such as age, sex, co-morbidities, and smoking status. Furthermore, to our knowledge, they have all been developed by surgeons without patient input.
Patient-specific factors, behaviours, and co-morbidities are established contributors to QOL outcomes in major abdominal surgery, such as colorectal resections [48]. In this review, the majority of studies (26 studies) reported patient-specific factors separately including sex, age, BMI, diabetes, smoking, cardio-respiratory function, steroid use, previous surgery, and tobacco smoking. The most commonly used generic QOL tools do not collect these data when assessing quality of life. Whilst these demographics are not quality-of-life measurements in themselves, they can negatively contribute to increased post-operative morbidity, increased length of hospital stay, and increased risk of hernia recurrence [49]. Recurrence significantly negatively affects QOL and can reduce it to below pre-operative baseline [15, 24, 39]. Such factors appear correlated to QOL and measuring them may be useful. The impact of hernia size on QOL was poorly reported. Where compared large hernia size was seen to negatively impact on QOL. However, the literature is heterogeneous and often patients with different size hernias are bundled together. Patients with different hernia sizes have different expectations and experiences, and therefore, how their hernia impacts their QOL will differ. Current AWH QOL tools do not take into account hernia size or hernia defect size meaning that we cannot discriminate when comparing the tools. This makes interpreting results difficult and is a limitation of the currently available tools. Patient satisfaction is not included in QOL assessment tools, but has been reported in a number of included studies. While measuring patient satisfaction as a proxy of QOL may not be ideal, a satisfied patient may have perceived improvement in QOL relative to a dissatisfied patient. How a patient feels about their surgery could also introduce bias into their responses when completing a QOL assessment and as such should perhaps be accounted for.
Ability to work, and time to return to work are an important outcome measure for many patients and wider society as a whole. Many AWH patients are of working age and there must be a negative economic impact on them being unable to do so. Although work activities are included as a score in the ASS; occupation, demographics, significant other diagnoses, impact on body image, and co-morbidities are not accounted for in the CCS, HerQLes, or short-form surveys. Gender impacts scores in the SF-36 and SF-12 QOL assessment methods with women regularly scoring lower than men [50], but its impact on disease-specific tools is unknown. There is limited evidence in the literature on abdominal wall repair in pregnancy and no consideration or assessment of pregnancy, fertility, or fecundity in hernia QOL tools.
Ultimately, assessing QOL is a patient-reported outcome and as such is subjective. Factors impacting most greatly on QOL are likely to vary from patient to patient. Including aspects important to patients, rather than clinicians, can only be achieved through patient participation and involvement in developing a universally accepted tool. For some patients, certain factors will hold more weight than others and pre-operative discussion and decision-making should be focussed towards an individual patient expectations. Decision-making in AWH surgery remains difficult. This said, the use of such a suitable and acceptable universal pre-operative QOL measurement and/or being able to predict subsequent QOL improvements in patients undergoing successful surgery would aid decision-making for the patient and the surgeon. QOL measurement can and should be a valuable adjunct in decision-making.
Limitations
Risk of bias
Existing reference tools were analysed and used to assess the methodology of the studies to determine if studies were at “low, “high”, or “unclear” risk of bias. The methodology of the studies was analysed the quality of the study which was evaluated using the Cochrane risk of bias tool for randomised-controlled studies and the ROBBINS-I tool for non-randomised or observational studies. However, this was not accounted for as part of the review as all studies that underwent full literature review and fulfilled the inclusion criteria were included.
Exclusion of non-English language studies
English language studies were excluded from this review. While inclusion may have led to perceived inaccuracies in translation and interpretation due to language barriers, we accept that there may be relevant data overlooked.
Conclusions
This review highlights significant variation in the adoption and utilisation of QOL tools in the AWH literature. No one tool has become dominant in this field. Hernia-specific QOL tools are becoming more popular. However, the most frequently used scale is still the generic SF-36 most likely due to perceived inadequacies in hernia-specific QOL tools or fears that without a well-known, validated, established tool being used the data will not be published. Regardless of which tool is used, there may be key aspects to being an AWH patient that are still not being captured by any of them.
Assessment, therefore, of the impact of repair, or different techniques, on quality of life remains difficult. More work is required to refine and develop these QOL tools to help guide management and to embed validated, structured QOL measurement into patient and surgeon peri-operative decision-making. A single, user friendly, tool incorporating components from disease-specific and generic QOL tools that is can be used for a standardised period of long-term follow-up may provide this.
References
Le Huu NR, Mege D, Quaissi M, Seilezneff I, Sustre B (2012) Incidence and prevention of ventral incisional hernias. J Visc Surg 149:e3–14
Blair L, Cox T, Huntington C, Groene S, Prasad T, Lincourt A, Kercher K, Heniford T, Augenstein V (2016) The effect of component separation technique on quality of life (QOL) and surgical outcomes in complex open ventral herniarepair (OVHR). Surg Endosc 31:3539–3546
Parker SG, Halligan S, Erotocritou M, Wood CPJ, Boulton RW, Plumb AAO, Windsor ACJ, Mallett S (2019) A systematic methodological review of non-randomised interventional studies of elective ventral hernia repair: clear definitions and a standardised minimum dataset are needed. Hernia 23(5):859–872
Aliotta RE, Gatherwright J, Krpata D, Rosenblatt S, Rosen M, Gurunluoglu R (2019) Complex abdominal wall reconstruction, harnessing the power of a specialised mulit-disciplinary team to improve pain and quality of life. Hernia 23:205–215
Muirhead LJ, Shaw AV, Kontovonisios C, Warren OJ (2019) Establishing a robust multi-disciplinary team process in complex abdominal wall reconstruction in a colorectal surgical unit. Tech Coloproctol 23(4):379–383
Hawn MT, Snyder CW, Graham LA (2010) Long-term follow-up of technical outcomes for incisional hernia repair. J Am Coll Surg 210:648–655
Luijendijk RW, Hop WC, van den Tol MP (2000) A comparison of suture repair with mesh repair for incisional hernia. N Eng J Med 343:392–398
Anthony T, Long J, Hynan LS, Sarosi GA, Nwariaku F, Huth J, Jones C, Parker BJ, Bege R (2003) Surgical complications exert a lasting effect on disease-specific health-related quality of life for patients with colorectal cancer. Surgery 134:119–125
Colavita PD, Tsirline VB, Belyansky I (2012) Prospective long-term comparison of quality of life in laparoscopic versus open ventral hernia repair. Ann Surg 256:714–722
Heniford BT, Walters AE, Lincourt AE, Novitsky YW, Hope WW, Kercher KW (2008) Comparison of generic versus specific quality-of-life scales for mesh hernia repairs. J Am Coll Surg 206(4):638–644
Heniford BT, Lincourt AE, Walters AL, Colavita PD, Belyansky I, Kercher KW, Sing RF, Augenstein VA (2018) Carolinas comfort scale as a measure of hernia repair quality of life. Ann Surg 267:171–176
Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault GG, Chelala E, Dietz UA, Eker HH, El Nakadi I, Hauters P, Hidalgo Pascual M, Hoeferlin A, Klinge U, Montgomery A, Simmermacher RK, Simons MP, Smietański M, Sommeling C, Tollens T, Vierendeels T, Kingsnorth A (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13(4):407–414
Krpata DM, Schnotzer BJ, Flocke S, Jin J, Blatnik J, Ermlich B, Novitsky YW, Rosen MJ (2012) Design and initial implementation of HerQLes: a hernia-related quality-of-life survey to assess abdominal wall function. J Am Coll Surg 215(5):635–642
Nissen AT, Henn D, Moshrefi S, Gupta D, Nazerali R, Lee GK (2019) Health-related quality of life after ventral hernia repair with biologic and synthetic mesh. Ann Plast Surg 2019(82):S332–S338
Feng MP, Baucom RB, Broman KK, Harris DA, Holzman MD, Huang LC, Kaiser JL, Kavalukas SL, Oyefule OO, Phillips SE, Poulose BK, Pierce RA (2018) Early repair of ventral incisional hernia may improve quality of life after surgery for abdominal malignancy: a prospective observational cohort study. Hernia 23:81–90
Criss CN, Petro CC, Krpata DM, Seafler CM, Lai N, Fiutem J, Novitsky YW, Rosen MJ (2014) Functional abdominal wall reconstruction improves core physiology and quality-of-life. Surgery 156(1):176–182
Cherla DV, Moses ML, Viso CP, Holihan JL, Flores-Gonzalez JR, Kao LS, Ko TC, Liang MK (2017) Impact of abdominal wall hernias and repair on patient quality of life. World J Surg 42:19–25
Ross SW, Wormer BA, Kim M, Oommen B, Bradley JF, Lincourt AE, Augenstein VA, Heniford BT (2015) Defining surgical outcomes and quality of life in massive ventral hernia repair: an international multicenter prospective study. Am J Surg 210:801–813
Kilma DA, Tsirline VB, Belyansky I, Dacey KT, Lincourt AE, Kercher KW, Heniford BT (2014) Quality of life following component separation versus standard open ventral hernia repair for large hernias. Surg Innov 21(2):147–154
Groene S, Huntington C, Blair L, Cox T, Prasad T, Lincourt A, Kercher K, Heniford BT, Augenstein V (2016) Long-term assessment of surgical and quality of life (QOL) outcomes in ventral hernia repair (VHR) in patients with and without an intraoperative enterotomy. Hernia 20(2):139–258
Snyder CW, Graham LA, Vick CC, Gray SH, Finan KR, Hawn MT (2011) Patient satisfaction, chronic pain and quality of life after elective incisional hernia repair: effect of recurrence and repair technique. Hernia 15:123–129
De Paep K, Berrevoet F (2015) Quality of life and cosmetic outcome following component separation for open ventral hernia repair for large hernias. Hernia (Supp I2):S3–S194
Alkhatib H, Tastaldi L, Krpata DM, Scheman J, Petro CC, Fafaj A, Rosenblatt S, Rosen MJ, Prabhu AS (2019) Prevalence of posttraumatic stress disorder (PTSD) in patients with an incisional hernia. Am J Surg 19:30139–30144
Langbach O, Bukholm I, Benth RS, Røkke O (2016) Long-term quality of life and functionality after ventral hernia mesh repair. Surg Endosc 30:5023–5033
Jensen K, Munim K, Kjaer M, Jorgensen LN (2017) Abdominal wall reconstruction for incisional hernia optimizes truncal function and quality of life. Ann Surg 2017(265):1235–1240
Nielsen K, Poelman MM, den Bakker FM, van der Ploeg T, Bonjer HJ, Schreurs WH (2014) Comparison of the Dutch and English versions of the Carolinas Comfort Scale: a specific quality-of-life questionnaire for abdominal hernia repairs with mesh. Hernia 18:459–464
Hope WW, Lincourt AE, Newcomb WL, Schmelzer TM, Kercher KW, Heniford BT (2008) Comparing quality-of-life outcomes in symptomatic patients undergoing laparoscopic or open ventral hernia repair. J Laparoendosc Adv Surg Tech 18:4
Poelman MM, Schellekens JF, Langenhorst BLAM, Schreurs WH (2010) Health-related quality of life in patients treated for incisional hernia with an onlay technique. Hernia 14:237–242
Bansal VK, Asuri K, Panaiyadiyan S, Kumar S, Subramaniam R, Ramachandran R, Sagar R, Misra MC (2016) Comparison of absorbable versus nonabsorbable tackers in terms of long-term outcomes, chronic pain, and quality of life after laparoscopic incisional hernia repair: a randomized study. Surg Laparosc Endosc Percutan Tech 26:476–483
Eriksen JR, Poornoroozy P, Jørgensen LN, Jacobsen B, Friis-Andersen HU, Rosenberg J (2009) Pain, quality of life and recovery after laparoscopic ventral hernia repair. Hernia 13:13–21
Rogmark P, Petersson U, Bringman S, Exra E, Osterberg J, Mongomery A (2016) Quality of life and surgical outcome 1 year after open and laparoscopic incisional hernia repair: PROLOVE: a randomised control study. Ann Surg 263:244–250
Van Ramshorst GH, Eker HH, Hop WGJ, Jeekel J, Lange JF (2012) Impact of incisional hernia on health related quality of life and body image: a prospective cohort study. Am J Surg 204:144–150
ZarZaur BL, DiCoco JM, Shahen CP, Emmett K, Magnotti LJ, Coce MA, Hathaway DK, Fabian TC (2011) Quality of life after open abdominal wall reconstruction following an open abdomen. J Trauma 70:285–291
Scott-Roth J, Zachem A, Lymale MA (2017) Complex ventral hernia repair with acellular dermal matrices: clinical and quality of life outcomes. Am Surg 83(2):141–147
Rosen MJ, Bauer JJ, Harmaty M, Carbonell AM, Cobb WS, Matthew B, Goldblatt MI, Selzer DJ, Poulose BK, Hansson BME, Rosmam C, Chao JJ, Jacobsen GR (2017) Multicenter, prospective, longitudinal study of the recurrence, surgical site infection, and quality of life after contaminated ventral hernia repair using biosynthetic absorbable mesh. Ann Surg 265:205–211
Aho JM, Nourallah A, Samaha MJ, Antiel RM, Dupont SL, Ballmann KV, Sloan JA, Bingener J (2016) Patient reported outcomes after laparoscopic ventral hernia repair. Ann Surg 82(6):550–556
Thomsen CO, Brondum TL, Jorgensen LN (2016) Quality of life after ventral hernia repair with endoscopic component separation technique. Scand J Surg 105(1):11–16
Juvany M, Hoyuela C, Carvajal F, Trias M, Martat A, Andid J (2018) Long term follow up (5 Years) of midline incisional hernia repairs using primary closure and prosthetic onlay techniques: recurrence and quality of life. Hernia 22:319–324
Bansal VK, Misra MC, Babu D, Singhal P, Rao K, Segar R, Kumar S, Rajeshwari S, Rewari V (2012) Comparison of long-term outcomes and quality of life after laparoscopic repair of incisional and ventral hernias with suture fixation with and without tacks: a randomised controlled study. Surg Endosc 26:3476–3485
Asti E, Sorini A, Lovece A, Bonitta G, Bonavina L (2016) Open vs laparoscopic management of incisional ventral hernia: cohort study comparing quality of life outcomes. J Laparoendosc Adv Surg Tech 26(4):249–255
McCarthy M, Jonasson O, Chang CH, Pickard AS, Giobbie-Herder A, Gibbs J, Edelman P, Fitzgibbons R, Neumayr L (2005) Assessment of patient functional status after surgery. J Am Coll Surg 201(5):826
Groene SA, Tanushree Prasad T, Lincourt AE, Augenstein VA, Sing R, Heniford BT (2016) Prospective, multi-institutional surgical and quality-of-life outcomes comparison of heavyweight, midweight, and lightweight mesh in open ventral hernia repair. Am J Surg 212:1054–1062
Barber MD, Kenton K, Janz NK, Hsu Y, Dyer KY, Greer WJ, Ye W (2012) Validation of the activities assessment scale in women undergoing pelvic reconstructive surgery. Female Pelvic Med Reconstr Surg 18(4):205–210
Jensen KK, Henriksen NA, Harling H (2014) Standardised measurement of quality of life after incisional hernia repair: a systematic review. Am J Surg 28:485–493
Parker SG, Wood CPJ, Sanders DL, Windsor ACJ (2017) Nomenclature in abdominal wall hernias: is it time for consensus? World J Surg 41(10):2488–2491
Jenkinson C, Layte R, Jenkinson D, Lawrence K, Petersen S, Paice C, Stradling J (1997) A Shorter form health survey: can the SF-12 replicate results from the SF-36 in longitudinal studies? J Public Health 19(2):179–186
Velanovich V (1998) Comparison of generic (SF-36) and disease-specific (GERD-HRQOL) quality of life scales for gastro-oesophageal reflux disease. J Gastroint Surg 2:141–145
Cummings A, Grimmet C, Calman L, Patel M, Permykova NV, Winter J, Carner J, Din A, Fenlon D, Richardson A, Smith PW, Members of the CREW Study Advisory Committee, Foster C (2018) Co-morbidities are associated with poorer quality of life and functioning and worse symptoms in the 5 years following colorectal cancer surgery: results of the ColoREctal Well-being (CREW) study. Psychooncology 27(10):2427–2453
Ware J Jr, Kosinski M, Keller SD (1997) A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. MedCare 34:220–233
Hemingway H, Stafford M, Stansfeld S, Shipley M, Marmot M (1997) Is the SF-36 a valid measure of change in population health? Results from the Whitehall II study. BMJ 315:1273–1279
Acknowledgements
To the best of our knowledge, there are no conflicts of interest and no author has received funding for this review or has any affiliation
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Ethical approval
Ethical approval for this review study was not required.
Informed consent
None.
Human and animal rights
This study does not involve human or animal participations. It is a review of available literature only.
Research involving human participants and/or animals
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Grove, T.N., Muirhead, L.J., Parker, S.G. et al. Measuring quality of life in patients with abdominal wall hernias: a systematic review of available tools. Hernia 25, 491–500 (2021). https://doi.org/10.1007/s10029-020-02210-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-020-02210-w