Abstract
Background
Pancreatic redo procedures belong to the most difficult abdominal operations because of altered anatomy, significant adhesions, and the potential of recurrent disease. We report on our experience with 15 redo procedures among a series of 350 consecutive pancreatic operations.
Patient and Methods
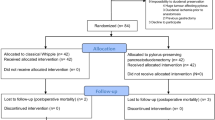
From January 1, 2004 to May 31, 2006 a total of 350 patients underwent pancreatic surgery in our department. There were 15 patients identified who had pancreatic redo surgery for benign (14) or malignant (1) disease. Perioperative parameters and outcome of 15 patients undergoing redo surgery after pancreatic resections were evaluated.
Results
Operative procedures included revision and redo of the pancreaticojejunostomy after resection of the pancreatic margin (6), completion pancreatectomy (3), conversion from duodenum-preserving pancreatic head resection to pylorus-preserving pancreaticoduodenectomy (3), classic pancreaticoduodenectomy after nonresective pancreatic surgery (1), redo of left-sided pancreatectomy (1), and classic pancreaticoduodenectomy after left-sided pancreatectomy (1). Histology revealed chronic pancreatitis in 14 and a mucinous adenocarcinoma of the pancreas in 1 patient. Median operative time was 335 min (235–615 min) and median intraoperative blood loss was 600 ml (300–2,800 ml). Median postoperative ICU stay was 20 h (4–113 h) and median postoperative hospital stay was 15 days (7–30 days). There was no perioperative mortality and morbidity was 33%.
Conclusion
Pancreatic redo surgery can be performed with low morbidity and mortality. Redo surgery has a defined spectrum of indications, but to achieve good results surgery may be performed at high-volume centers.





Similar content being viewed by others
References
Winter JM, Cameron JL, Lillemoe KD, Campbell KA, Chang D, Riall TS, Coleman J, Sauter PK, Canto M, Hruban RH, Schulick RD, Choti MA, Yeo CJ. Periampullary and pancreatic incidentaloma: a single institution’s experience with an increasingly common diagnosis. Ann Surg 2006;243:673–680; discussion 680–683.
Van Heek NT, Kuhlmann KF, Scholten RJ, de Castro SM, Busch OR, Van Gulik TM, Obertop H, Gouma DJ. Hospital volume and mortality after pancreatic resection: a systematic review and an evaluation of intervention in The Netherlands. Ann Surg 2005;242:781–788; discussion 788–790.
Hannan EL, Radzyner M, Rubin D, Dougherty J, Brennan MF. The influence of hospital and surgeon volume on in-hospital mortality for colectomy, gastrectomy, and lung lobectomy in patients with cancer. Surgery 2002;131:6–15.
Dimick JB, Pronovost PJ, Cowan JA, Lipsett PA. Surgical volume and quality of care for esophageal resection: do high-volume hospitals have fewer complications? Ann Thorac Surg 2003;75:337–341.
Schrag D, Panageas KS, Riedel E, Cramer LD, Guillem JG, Bach PB, Begg CB. Hospital and surgeon procedure volume as predictors of outcome following rectal cancer resection. Ann Surg 2002;236:583–592.
Fong Y, Gonen M, Rubin D, Radzyner M, Brennan MF. Long-term survival is superior after resection for cancer in high-volume centers. Ann Surg 2005;242:540–544; discussion 544–547.
Sohn TA, Lillemoe KD, Cameron JL, Pitt HA, Huang JJ, Hruban RH, Yeo CJ. Reexploration for periampullary carcinoma: resectability, perioperative results, pathology, and long-term outcome. Ann Surg 1999;229:393–400.
Belyaev O, Herzog T, Chromik A, Muller CA, Uhl W. Surgery of the pancreas: The surgeon as the crucial prognostic factor. Der Gastroenterologe 2006;1:34–42.
Keith RG, Keshavjee SH, Kerenyi NR. Neuropathology of chronic pancreatitis in humans. Can J Surg 1985;28:207–211.
Beger HG, Witte C, Krautzberger W, Bittner R. Experiences with duodenum-sparing pancreas head resection in chronic pancreatitis. Chirurg 1980;51:303–307.
Frey CF, Smith GJ. Description and rationale of a new operation for chronic pancreatitis. Pancreas 1987;2:701–707.
Strate T, Taherpour Z, Bloechle C, Mann O, Bruhn JP, Schneider C, Kuechler T, Yekebas E, Izbicki JR. Long-term follow-up of a randomized trial comparing the Beger and Frey procedures for patients suffering from chronic pancreatitis. Ann Surg 2005;241:591–598.
McGuire GE, Pitt HA, Lillemoe KD, Niederhuber JE, Yeo CJ, Cameron JL. Reoperative surgery for periampullary adenocarcinoma. Arch Surg 1991;126:1205–10; discussion 1210–1212.
Tyler DS, Evans DB. Reoperative pancreaticoduodenectomy. Ann Surg 1994;219:211–221.
Shukla PJ, Qureshi SS, Shrikhande SV, Jagannath P, Desouza LJ. Reoperative pancreaticoduodenectomy for periampullary carcinoma. ANZ J Surg 2005;75:520–523.
Schnelldorfer T, Lewin DN, Adams DB. Reoperative surgery for chronic pancreatitis: is it safe? World J Surg 2006;30:1321–1328.
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 2005;138:8–13.
House MG, Cameron JL, Schulick RD, Campbell KA, Sauter PK, Coleman J, Lillemoe KD, Yeo CJ. Incidence and outcome of biliary strictures after pancreaticoduodenectomy. Ann Surg 2006;243:571–576; discussion 576–578.
Buchler MW, Friess H, Muller MW, Wheatley AM, Beger HG. Randomized trial of duodenum-preserving pancreatic head resection versus pylorus-preserving Whipple in chronic pancreatitis. Am J Surg 1995;169:65–69; discussion 69–70.
Whitcomb DC. Inflammation and Cancer V. Chronic pancreatitis and pancreatic cancer. Am J Physiol Gastrointest Liver Physiol 2004;287:G315–G319.
Acknowledgement
Matthias H. Seelig and Ansgar M. Chromik have contributed equally to the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Seelig, M.H., Chromik, A.M., Weyhe, D. et al. Pancreatic Redo Procedures: To do or Not To Do—This is the Question. J Gastrointest Surg 11, 1175–1182 (2007). https://doi.org/10.1007/s11605-007-0159-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-007-0159-2