Abstract
Background
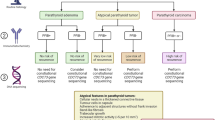
The sequencing of the renal cell carcinoma (RCC) genome has detected several mutations with prognostic meaning. The association between visceral adipose tissue (VAT) and clear cell renal cell carcinoma (ccRCC) is well known. The relationship among abdominal adipose tissue distribution and ccRCC-VHL and KDM5C genetic mutations is, to the knowledge of the authors, not known.
Methods
In this retrospective study, we enrolled 97 Caucasian male patients divided into three groups: the control group (n = 35), the ccRCC-VHL group (n = 52) composed of ccRCC patients with VHL mutations and ccRCC-KDM5C group (n = 10) composed of ccRCC patients with KDM5C mutation. Total adipose tissue (TAT) area, VAT area and subcutaneous adipose tissue (SAT) area were measured in the groups. VAT/SAT ratio was calculated for each subject.
Results
Statistically significant differences between ccRCC-KDM5C group and ccRCC-VHL group were obtained for TAT area (p < 0.05), VAT area (p < 0.05) and VAT/SAT ratio (p < 0.05); between ccRCC-VHL group and control group for TAT area (p < 0.001) and VAT area (p < 0.01); and between ccRCC-KDM5C group and control group for TAT area (p < 0.0001), VAT area (p < 0.0001) and SAT area (p < 0.01).
Conclusions
This study demonstrates for the first time an increased amount of TAT, especially VAT, in the ccRCC-VHL and ccRCC-KDM5C groups. The effect was greater for the ccRCC-KDM5C group.


Similar content being viewed by others
References
Kuo MD, Jamshidi N (2014) Behind the numbers: decoding molecular phenotypes with radiogenomics-guiding principles and technical considerations. Radiology 270(2):320–325
Lander ES, Linton LM, Birren B, Nusbaum C, Zody MC, Baldwin J et al (2001) Initial sequencing and analysis of the human genome. Nature 409(6822):860–921
Alessandrino F, Krajewski KM, Shinagare AB (2016) Update on radiogenomics of clear cell renal cell carcinoma. Eur Urol Focus 2(6):572–573
Pinker K, Shitano F, Sala E, Do Richard K, Young Robert J, Wibmer Andreas G et al (2018) Background, current role, and potential applications of radiogenomics. J Magn Reson Imaging 47:604–620
Sala E, Mema E, Himoto Y, Veeraraghavan H, Brenton JD, Snyder A et al (2017) Unravelling tumour heterogeneity using next-generation imaging: radiomics, radiogenomics, and habitat imaging. Clin Radiol 72(1):3–10
The Cancer Genome Atlas Research Network (2013) Comprehen- sive molecular characterization of clear cell renal cell carcinoma. Nature 499(7456):43–49
Karlo CA, Di Paolo PL, Chaim J, Ari Hakimi A, Ostrovnaya I, Russo P et al (2014) Radiogenomics of clear-cell renal cell carcinoma: associations between CT imaging features and mutations. Radiology 270(2):464–471
Shinagare AB, Vikram R, Jaffe C, Akin O, Kirby J, Huang E et al (2015) Radiogenomics of clear cell renal cell carcinoma: preliminary findings of The Cancer Genome Atlas-Renal Cell Carcinoma (TCGA–RCC) Imaging Re- search Group. Abdom Imaging 40(6):1684–1692
Seizinger BR, Rouleau GA, Ozelius LJ, Lane AH, Farmer GE, Lamiell JM et al (1988) Von Hippel– Lindau disease maps to the region of chromosome 3 associated with renal cell carcinoma. Nature 332(6161):268–269
Alessandrino F, Shinagare AB, Bossé D, Choueiri CK (2019) Krajewski KM (2019) Radiogenomics in renal cell carcinoma. Abdom Radiol (NY) 44(6):1990–1998
Ibrahim MM (2020) Subcutaneous and visceral adipose tissue: structural and functional differences. Obes Rev Off J Int Assoc Study Obes 11(1):11–18
Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich-Horvat P, Liu CY et al (2007) Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation 116(1):39–48
Greco F, Cirimele V, Mallio CA, Beomonte Zobel B, Grasso RF (2018) Increased visceral adipose tissue in male patients with clear cell renal cell carcinoma. Clin Cancer Investig J 7(4):132–136
Del Buono R, Sabatino L, Greco F (2018) Neck fat volume as a potential indicator of difficult intubation: a pilot study. Saudi J Anaesth 12:67–71
Greco F, Mallio CA, Cirimele V, Grasso RF, Beomonte Zobel B (2019) Subcutaneous adipose tissue as a biomarker of pancreatic cancer: a pilot study in male patients. Clin Cancer Investig J 8(3):10–19
Mallio CA, Greco F, Pacella G, Schena E, Beomonte Zobel B (2018) Gender-based differences of abdominal adipose tissue distribution in non-small cell lung cancer patients. Shanghai Chest 2(20)
Despres JP, Lemieux I (2006) Abdominal obesity and metabolic syndrome. Nature 444(7121):881–887
Zhang HP, Zou J, Xu ZQ, Ruan J, Yang SD, Yin Y et al (2017) Association of leptin, visfatin, apelin, resistin and adiponectin with clear cell renal cell carcinoma. Oncol Lett 13:463–468
Buechler C, Krautbauer S, Eisinger K (2015) Adipose tissue fibrosis. World J Diabetes 6(4):548–553
de Cubas AA, Rathmell WK (2018) Epigenetic modifers: activities in renal cell carcinoma. Nat Rev Urol 15(10):599–614
NIH National Cancer Institute: https://cancergenome.nih.gov/
Akin O, Elnajjar P, Heller M, Jarosz R, Erickson BJ, Kirk S et al (2016) Radiology data from the cancer genome atlas kidney renal clear cell carcinoma [TCGA-KIRC] collection. Cancer Imaging Arch. https://doi.org/10.7937/K9/TCIA.2016.V6PBVTDR
Clark K, Vendt B, Smith K, Freymann J, Kirby J, Koppel P et al (2013) The Cancer Imaging Archive (TCIA): maintaining and Operating a Public Information Repository. J Digit Imaging 26(6):1045–1057
Noumura Y, Kamishima T, Sutherland K, Nishimura H (2017) Visceral adipose tissue area measurement at a single level: can it represent visceral adipose tissue volume? Br J Radiol 90(1077):20170253
Greco F, Quarta LG, Grasso RF, Beomonte Zobel B, Mallio CA (2020) Increased visceral adipose tissue in clear cell renal cell carcinoma with and without peritumoral collateral vessels. Br J Radiol 93(1112):20200334
Greco F, Mallio CA, Grippo R, Messina L, Vallese S, Rabitti C et al (2020) Increased visceral adipose tissue in male patients with non-clear cell renal cell carcinoma. Radiol Med 125:538–543
Fischer-Posovszky P, Wabitsch M, Hochberg Z (2007) Endocrinology of adipose tissue: An update. Horm Metab Res 39(5):314–321
Raucci R, Rusolo F, Sharma A, Colonna G, Castello G, Costantini S et al (2013) Functional and structural features of adipokine family. Cytokine 61(1):1–14
Bolinder J, Kerckhoffs DA, Moberg E, Toft E, Arner P (2000) Rates of skeletal muscle and adipose tissue glycerol release in nonobese and obese subjects. Diabetes 49:797–802
Pasarica M, Sereda OR, Redman LM, Albarado DC, Hymel DT, Roan LE, Rood JC, Burk DH, Smith SR (2009) Reduced adipose tissue oxygenation in human obesity: evidence for rarefaction, macrophage chemotaxis, and inflammation without an angiogenic response. Diabetes 58:718–725
Brahimi-Horn MC, Pouysségur J (2007) Oxygen, a source of life and stress. FEBS Lett 581:3582–3591
Goossens GH, Moors CCM, van der Zijl NJ, Venteclef RA, Jocken JWE, Essers Y, Cleutjens JP, Clément K, Diamant M, Blaak EE (2012) Valsartan improves adipose tissue function in humans with impaired glucose metabolism: A randomized placebo-controlled double-blind trial. PLoS One 7:e39930
Goossens GH, Blaak EE (2015) Adipose tissue dysfunction and impaired metabolic health in human obesity: a matter of oxygen? Front Endocrinol 6:55
García-Fuentes E, Santiago-Fernández C, Gutiérrez-Repiso C, Mayas MD, Oliva-Olivera W, Coín-Aragüez L et al (2015) Hypoxia is associated with a lower expression of genes involved in lipogenesis in visceral adipose tissue. J Transl Med 13:373
Masoud GN, Li W (2015) HIF-1α pathway: role, regulation and intervention for cancer therapy. Acta Pharm Sin B 5(5):378–389
Brugarolas J (2014) Molecular genetics of clear-cell renal cell carcinoma. J Clin Oncol 32(18):1968–1976
Stebbins CE, Kaelin WG Jr, Pavletich NP (1999) Structure of the VHL-ElonginC–ElonginB complex: implications for VHL tumor suppressor function. Science 284:455–461
Maxwell PH, Wiesener MS, Chang GW, Clifford SC, Veux EC, Cockman ME (1999) The tumor suppressor protein VHL targets hypoxia-inducible factors for oxygen-dependent proteolysis. Nature 399(6733):271–275
Cancer Genome Atlas Research Network (2013) Comprehensive molecular characterization of clear cell renal cell carcinoma. Nature 499:43–49. https://doi.org/10.1038/nature12222PMID: 23792563
Niu X, Zhang T, Liao L, Zhou L, Lindner DJ, Zhou M et al (2012) The Von Hippel-Lindau tumor suppressor protein regulates gene expression and tumor growth through histone demethylase JARID1C. Oncogene 31:776–786. https://doi.org/10.1038/onc.2011.266PMID: 21725364
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. FG, CAM helped in conception and design, definition of intellectual content, literature search, clinical studies, experimental studies, data analysis, statistical analysis. FG contributed to data acquisition, manuscript preparation. CAM was involved in manuscript editing and manuscript review. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
Institutional review board was not required because this is an observational retrospective study, and only existing information collected from human participants are used, and there are not any identifiers linking individual to the data. This article does not contain any studies with animals performed by any of the authors.
Informed consent
The study was performed in accordance with the Declaration of Helsinki. The institutional ethical committee approved the study. All subjects enrolled provided a written informed consent to use their anonymized data for research purposes.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Greco, F., Mallio, C.A. Relationship between visceral adipose tissue and genetic mutations (VHL and KDM5C) in clear cell renal cell carcinoma. Radiol med 126, 645–651 (2021). https://doi.org/10.1007/s11547-020-01310-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-020-01310-y