Abstract
Purpose
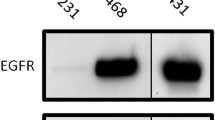
Nanobodies represent an interesting class of probes for the generic development of molecular imaging agents. We studied the relationship between tumor uptake of the epidermal growth factor receptor (EGFR)-specific nanobody 99mTc-7C12 and tumor burden and evaluated the possibility of using this probe to monitor tumor response to erlotinib.
Procedures
The specificity and affinity of 99mTc-7C12 was determined on A431 cells. Cells expressing firefly luciferase were used to evaluate tumor burden using bioluminescence imaging. We evaluated the effect of erlotinib on tumor burden and 99mTc-7C12 uptake in vitro as well as in vivo. In vivo bioluminescence imaging was performed followed by pinhole single-photon emission computed tomography/micro-computed tomography.
Results
99mTc-7C12 binds specifically to the receptor with high affinity (3.67 ± 0.59 nM). Erlotinib reduced tumor uptake and cell viability in a concentration-dependent manner. Tumor uptake of 99mTc-7C12 showed good correlation with tumor burden. Erlotinib treatment resulted in a progressive reduction of tumor burden and tumor uptake of 99mTc-7C12.
Conclusion
99mTc-7C12 binds to EGFR with high affinity and specificity. Tumor uptake is correlated with tumor burden. Quantification of 99mTc-7C12 uptake is promising for monitoring therapy response of EGFR-expressing tumors.






Similar content being viewed by others
References
Yarden Y, Sliwkowski MX (2001) Untangling the ErbB signalling network. Nat Rev Mol Cell Biol 2(2):127–137
Rocha-Lima CM, Soares HP, Raez LE, Singal R (2007) EGFR targeting of solid tumors. Cancer Control 14(3):295–304
Marshall J (2006) Clinical implications of the mechanism of epidermal growth factor receptor inhibitors. Cancer 107(6):1207–1218
Fan Z, Masui H, Altas I, Mendelsohn J (1993) Blockade of epidermal growth factor receptor function by bivalent and monovalent fragments of 225 anti-epidermal growth factor receptor monoclonal antibodies. Cancer Res 53:4322–4432
Kimura H, Sakai K, Arao T, Shimoyama T, Tamura T, Nishio K (2007) Antibody-dependent cellular cytotoxicity of cetuximab against tumor cells with wild-type or mutant epidermal growth factor receptor. Cancer Sci 98(8):1275–1280
Paez JG, Jänne PA, Lee JC et al (2004) EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science 304(5676):1497–1500
Lynch TJ, Bell DW, Sordella R et al (2004) Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med 350(21):2129–2139
Pao W, Miller V, Zakowski M et al (2004) EGF receptor gene mutations are common in lung cancers from “never smokers” and are associated with sensitivity of tumors to gefitinib and erlotinib. Proc Natl Acad Sci USA 101(36):13306–13311
Mancl EE, Kolesar JM, Vermeulen LC (2009) Clinical and economic value of screening for Kras mutations as predictors of response to epidermal growth factor receptor inhibitors. Am J Health Syst Pharm 66(23):2105–2112
Pao W, Wang TY, Riely GJ et al (2005) KRAS mutations and primary resistance of lung adenocarcinomas to gefitinib or erlotinib. PLoS Med 2(1):e17
Cai W, Chen K, He L, Cao Q, Koong A, Chen X (2007) Quantitative PET of EGFR expression in xenograft-bearing mice using 64Cu-labeled cetuximab, a chimeric anti-EGFR monoclonal antibody. Eur J Nucl Med Mol Imaging 34(6):850–858
Eiblmaier M, Meyer LA, Watson MA et al (2008) Correlating EGFR expression with receptor-binding properties and internalization of 64Cu-DOTA-cetuximab in 5 cervical cancer cell lines. J Nucl Med 49(9):1472–1479
Xu N, Cai G, Ye W et al (2009) Molecular imaging application of radioiodinated anti-EGFR human Fab to EGFR-overexpressing tumor xenografts. Anticancer Res 29(10):4005–4011
Velikyan I, Sundberg AL, Lindhe O et al (2005) Preparation and evaluation of (68)Ga-DOTA-hEGF for visualization of EGFR expression in malignant tumors. J Nucl Med 46(11):1881–1888
Reilly RM, Kiarash R, Sandhu J et al (2000) A comparison of EGF and MAb 528 labeled with 111In for imaging human breast cancer. J Nucl Med 41(5):903–911
Huang L, Gainkam LO, Caveliers V et al (2008) SPECT imaging with 99mTc-labeled EGFR-specific nanobody for in vivo monitoring of EGFR expression. Mol Imaging Biol 10(3):167–175
Gainkam LO, Huang L, Caveliers V et al (2008) Comparison of the biodistribution and tumor targeting of two 99mTc-labeled anti-EGFR nanobodies in mice, using pinhole SPECT/micro-CT. J Nucl Med 49(5):788–795
Lauwereys M, Arbabi Ghahroudi M et al (1998) Potent enzyme inhibitors derived from dromedary heavy-chain antibodies. EMBO J 17(13):3512–3520
Vincke C, Loris R, Saerens D, Martinez-Rodriguez S, Muyldermans S, Conrath K (2009) General strategy to humanize a camelid single-domain antibody and identification of a universal humanized nanobody scaffold. J Biol Chem 284(5):3273–3284
Roovers RC, Laeremans T, Huang L et al (2007) Efficient inhibition of EGFR signaling and of tumour growth by antagonistic anti-EFGR nanobodies. Cancer Immunol Immunother 56(3):303–317
Vanhove C, Defrise M, Bossuyt A, Lahoutte T (2009) Improved quantification in single-pinhole and multiple-pinhole SPECT using micro-CT information. Eur J Nucl Med Mol Imaging 36(7):1049–1063
Vanhove C, Defrise M, Lahoutte T, Bossuyt A (2008) Three-pinhole collimator to improve axial spatial resolution and sensitivity in pinhole SPECT. Eur J Nucl Med Mol Imaging 35(2):407–415
Loening AM, Gambhir SS (2003) AMIDE: a free software tool for multimodality medical image analysis. Mol Imaging 2(3):131–137
Keyaerts M, Verschueren J, Bos TJ et al (2008) Dynamic bioluminescence imaging for quantitative tumour burden assessment using IV or IP administration of d-luciferin: effect on intensity, time kinetics and repeatability of photon emission. Eur J Nucl Med Mol Imaging 35(5):999–1007
O'Connor JP, Jackson A, Asselin MC, Buckley DL, Parker GJ, Jayson GC (2008) Quantitative imaging biomarkers in the clinical development of targeted therapeutics: current and future perspectives. Lancet Oncol 9:766–776
Sunaga N, Oriuchi N, Kaira K et al (2008) Usefulness of FDG-PET for early prediction of the response to gefitinib in non-small cell lung cancer. Lung Cancer 59(2):203–210
de Geus-Oei LF, Vriens D, van Laarhoven HW, van der Graaf WT, Oyen WJ (2009) Monitoring and predicting response to therapy with 18F-FDG PET in colorectal cancer: a systematic review. J Nucl Med 50(Suppl 1):43S–54S
Kubota K, Ito K, Morooka M et al (2009) Whole-body FDG-PET/CT on rheumatoid arthritis of large joints. Ann Nucl Med 23(9):783–791, Epub 2009 Oct 16
Nordberg E, Orlova A, Friedman M et al (2008) In vivo and in vitro uptake of 111In, delivered with the affibody molecule (ZEGFR:955)2, in EGFR expressing tumour cells. Oncol Rep 19(4):853–7.30
Tolmachev V, Friedman M, Sandström M et al (2009) Affibody molecules for epidermal growth factor receptor targeting in vivo: aspects of dimerization and labeling chemistry. J Nucl Med 50(2):274–283
Pal A, Glekas A, Doubrovin M et al (2006) Molecular imaging of EGFR kinase activity in tumors with 124I-labeled small molecular tracer and positron emission tomography. Mol Imaging Biol 8(5):262–277
Abourbeh G, Dissoki S, Jacobson O et al (2007) Evaluation of radiolabeled ML04, a putative irreversible inhibitor of epidermal growth factor receptor, as a bioprobe for PET imaging of EGFR-overexpressing tumors. Nucl Med Biol 34(1):55–70
De Groeve K, Deschacht N, De Koninck C et al (2010) Nanobodies as tools for in vivo imaging of specific immune cell types. J Nucl Med 51(5):782–789
Vaneycken I, Govaert J, Vincke C et al (2010) In vitro analysis and in vivo tumor targeting of a humanized, grafted nanobody in mice using pinhole SPECT/micro-CT. J Nucl Med 51(7):1099–1106
van Eerd JE, Vegt E, Wetzels JF et al (2006) Gelatin-based plasma expander effectively reduces renal uptake of 111In-octreotide in mice and rats. J Nucl Med 47(3):528–533
Vegt E, Wetzels JF, Russel FG et al (2006) Renal uptake of radiolabeled octreotide in human subjects is efficiently inhibited by succinylated gelatin. J Nucl Med 47(3):432–436
Li S, Schmitz KR, Jeffrey PD, Wiltzius JJ, Kussie P, Ferguson KM (2005) Structural basis for inhibition of the epidermal growth factor receptor by cetuximab. Cancer Cell 7(4):301–311
Nogawa M, Yuasa T, Kimura S et al (2005) Monitoring luciferase-labeled cancer cell growth and metastasis in different in vivo models. Cancer Lett 217(2):243–253
Craft N, Bruhn KW, Nguyen BD et al (2005) Bioluminescent imaging of melanoma in live mice. J Invest Dermatol 125(1):159–165
Ling YH, Lin R, Perez-Soler R (2008) Erlotinib induces mitochondrial-mediated apoptosis in human H3255 non-small-cell lung cancer cells with epidermal growth factor receptor L858R mutation through mitochondrial oxidative phosphorylation-dependent activation of BAX and BAK. Mol Pharmacol 74(3):793–806
Qian X, Li J, Ding J, Wang Z, Zhang W, Hu G (2009) Erlotinib activates mitochondrial death pathways related to the production of reactive oxygen species in the human non-small cell lung cancer cell line A549. Clin Exp Pharmacol Physiol 36(5-6):487–494
Li T, Ling YH, Perez-Soler R (2008) Tumor dependence on the EGFR signaling pathway expressed by the p-EGFR:p-AKT ratio predicts erlotinib sensitivity in human non-small cell lung cancer (NSCLC) cells expressing wild-type EGFR gene. J Thorac Oncol 3(6):643–647
Atkinson DM, Clarke MJ, Mladek AC, Carlson BL, Trump DP, Jacobson MS, Kemp BJ, Lowe VJ, Sarkaria JN (2008) Using fluorodeoxythymidine to monitor anti-EGFR inhibitor therapy in squamous cell carcinoma xenografts. Head Neck 30(6):790–799
Acknowledgments
The research at ICMI is funded by the Interuniversity Attraction Poles Programme—Belgian State—Belgian Science Policy. Lea Olive Tchouate Gainkam is a Ph.D. fellow of the Horizontal Research Axis (HOA) grant of the Vrije Universiteit Brussel. Tony Lahoutte is a Senior Clinical Investigator of the Research Foundation—Flanders (FWO). Marleen Keyaerts is a Ph.D. fellow of the Research Foundation—Flanders (FWO). The authors acknowledge Ms. Cindy Peleman for her technical assistance with the small animal pinhole SPECT/micro-CT imaging. The authors are grateful to Lieven Huang for producing the nanobody.
Conflict of Interest Disclosure
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Manuscript Category and Significance:
Original article that investigates the relationship between tumor burden and uptake of radiolabeled 7C12 nanobody in response to an EGFR tyrosine kinase inhibitor. The preclinical data presented here strongly suggest that it will be feasible to monitor tumor response to therapy in clinical trial using this molecular imaging probe.
Rights and permissions
About this article
Cite this article
Tchouate Gainkam, L.O., Keyaerts, M., Caveliers, V. et al. Correlation Between Epidermal Growth Factor Receptor-Specific Nanobody Uptake and Tumor Burden: A Tool for Noninvasive Monitoring of Tumor Response to Therapy. Mol Imaging Biol 13, 940–948 (2011). https://doi.org/10.1007/s11307-010-0428-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11307-010-0428-4